预约演示
更新于:2025-08-29

Alba Therapeutics Corp.
更新于:2025-08-29
概览
关联
1
项与 Alba Therapeutics Corp. 相关的临床试验EUCTR2008-000415-14-ES
Ensayo de fase IIb, aleatorizado, doble ciego, controlado con placebo, para eltratamiento de la enfermedad celíaca activa con AT-1001
开始日期2008-10-06 |
申办/合作机构 |
100 项与 Alba Therapeutics Corp. 相关的临床结果
登录后查看更多信息
0 项与 Alba Therapeutics Corp. 相关的专利(医药)
登录后查看更多信息
4
项与 Alba Therapeutics Corp. 相关的文献(医药)2012-10-01·The American journal of gastroenterology1区 · 医学
A Randomized, Double-Blind Study of Larazotide Acetate to Prevent the Activation of Celiac Disease During Gluten Challenge
1区 · 医学
Article
作者: L A Arterburn ; J A Murray ; H Z Abdallah ; Daniel Alexander Leffler ; L A Harris ; B M Paterson ; Ciaran Patrick Kelly ; F Leon ; A M Colatrella ; Z H Lan
OBJECTIVES:
In patients with celiac disease, enteropathy is caused by the entry of gluten peptides into the lamina propria of the intestine, in which their immunogenicity is potentiated by tissue transglutaminase (tTG) and T-helper type 1-mediated immune responses are triggered. Tight junction disassembly and paracellular permeability are believed to have an important role in the transport of gluten peptides to the lamina propria. Larazotide acetate is a tight-junction regulator peptide that, in vitro, prevents the opening of intestinal epithelial tight junctions. The aim of this study was to evaluate the efficacy and tolerability of larazotide acetate in protecting against gluten-induced intestinal permeability and gastrointestinal symptom severity in patients with celiac disease.
METHODS:
In this dose-ranging, placebo-controlled study, 86 patients with celiac disease controlled through diet were randomly assigned to larazotide acetate (0.25, 1, 4, or 8 mg) or placebo three times per day with or without gluten challenge (2.4 g/day) for 14 days. The primary efficacy outcome was the urinary lactulose/mannitol (LAMA) fractional excretion ratio. Secondary endpoints included gastrointestinal symptom severity, quality-of-life measures, and antibodies to tTG.
RESULTS:
LAMA measurements were highly variable in the outpatient setting. The increase in LAMA ratio associated with the gluten challenge was not statistically significantly greater than the increase in the gluten-free control. Among patients receiving the gluten challenge, the difference in the LAMA ratios for the larazotide acetate and placebo groups was not statistically significant. However, larazotide acetate appeared to limit gluten-induced worsening of gastrointestinal symptom severity as measured by the Gastrointestinal Symptom Rating Scale at some lower doses but not at the higher dose. Symptoms worsened significantly in the gluten challenge-placebo arm compared with the placebo-placebo arm, suggesting that 2.4 g of gluten per day is sufficient to induce reproducible gluten toxicity. Larazotide acetate was generally well tolerated. No serious adverse events were observed. The most common adverse events were headache and urinary tract infection.
CONCLUSIONS:
LAMA variability in the outpatient setting precluded accurate assessment of the effect of larazotide acetate on intestinal permeability. However, some lower doses of larazotide acetate appeared to prevent the increase in gastrointestinal symptom severity induced by gluten challenge.
2012-05-01·Peptides3区 · 医学
Larazotide acetate regulates epithelial tight junctions in vitro and in vivo
3区 · 医学
Article
作者: Sefik S. Alkan ; Blake M. Paterson ; Shobha Gopalakrishnan ; Malarvizhi Durai ; Elena F. Verdu ; Robert Somerville ; Amir P. Tamiz ; Mark Ginski ; Kelly Kitchens ; Niranjan B. Pandey ; Joseph A. Murray
Tight junctions (TJs) control paracellular permeability and apical-basolateral polarity of epithelial cells, and can be regulated by exogenous and endogenous stimuli. Dysregulated permeability is associated with pathological conditions, such as celiac disease and inflammatory bowel disease. Herein we studied the mechanism by which larazotide acetate, an 8-mer peptide and TJ regulator, inhibits the cellular changes elicited by gliadin fragments, AT-1002, and cytokines. Previously, we demonstrated that AT-1002, a 6-mer peptide derived from the Vibrio cholerae zonula occludens toxin ZOT, caused several biochemical changes in IEC6 and Caco-2 cells resulting in decreased transepithelial electrical resistance (TEER) and increased TJ permeability. In this study, larazotide acetate inhibited the redistribution and rearrangement of zonula occludens-1 (ZO-1) and actin caused by AT-1002 and gliadin fragments in Caco-2 and IEC6 cells. Functionally, larazotide acetate inhibited the AT-1002-induced TEER reduction and TJ opening in Caco-2 cells. Additionally, larazotide acetate inhibited the translocation of a gliadin 13-mer peptide, which has been implicated in celiac disease, across Caco-2 cell monolayers. Further, apically applied larazotide acetate inhibited the increase in TJ permeability elicited by basolaterally applied cytokines. Finally, when tested in vivo in gliadin-sensitized HLA-HCD4/DQ8 double transgenic mice, larazotide acetate inhibited gliadin-induced macrophage accumulation in the intestine and preserved normal TJ structure. Taken together, our data suggest that larazotide acetate inhibits changes elicited by AT-1002, gliadin, and cytokines in epithelial cells and preserves TJ structure and function in vitro and in vivo.
2008-07-01·Journal of the American Dietetic Association
Algal-Oil Capsules and Cooked Salmon: Nutritionally Equivalent Sources of Docosahexaenoic Acid
Article
作者: Hamersley, Jacqueline ; Oken, Harry A. ; Hall, Eileen Bailey ; Hoffman, James P. ; Kuratko, Connye N. ; Arterburn, Linda M.
Food and nutrition professionals question whether supplement-sourced nutrients appear to be equivalent to those derived from natural food sources. We compared the nutritional availability of docosahexaenoic acid (DHA) from algal-oil capsules to that from assayed cooked salmon in 32 healthy men and women, ages 20 to 65 years, in a randomized, open-label, parallel-group study. In this 2-week study comparing 600 mg DHA/day from algal-oil capsules to that from assayed portions of cooked salmon, mean change from baseline in plasma phospholipids and erythrocyte DHA levels was analyzed and DHA levels were compared by Student's t tests. In post-hoc analyses to determine bioequivalence, least-squares mean ratios of percent change from baseline in plasma phospholipid and erythrocyte DHA levels were compared. DHA levels increased by approximately 80% in plasma phospholipids and by approximately 25% in erythrocytes in both groups. Changes in DHA levels in plasma phospholipids and erythrocytes were similar between groups. As measured by delivery of DHA to both plasma and erythrocytes, fish and algal-oil capsules were equivalent. Both regimens were generally well-tolerated. These results indicate that algal-oil DHA capsules and cooked salmon appear to be bioequivalent in providing DHA to plasma and red blood cells and, accordingly, that algal-oil DHA capsules represent a safe and convenient source of non-fish-derived DHA.
3
项与 Alba Therapeutics Corp. 相关的新闻(医药)2008-07-28
Baltimore Business Journal -- At the University of Maryland, Baltimore BioPark, one of the city’s newest life science research centers, getting biotechnology companies interested in the space isn’t a problem. Rather, when it comes to closing a lease deal, a handful of biotechs -- at least three from Baltimore -- have told UMB they are waiting to take new space until they land needed venture funding. However, those investment deals are fewer and farther between in Baltimore and the rest of the Washington, D.C. region, according to a report that says the number and value of venture deals for biotechs in the area fell by half during the second quarter of this year.
Venture capital investment in the biotech sector for the Washington, D.C., region -- which includes Maryland, Northern Virginia and Washington -- dipped to second quarter, according to the report released July 19 by the National Venture Capital Association and PricewaterhouseCoopers. That compares with 11 deals for $84.2 million for the same period in 2007.
“It’s taking longer than they would like” to woo venture capitalists, Jim Hughes, vice president of research and development for UMB, said of the biopark’s prospective tenants. “It’s been a challenge to raise money.”
Venture capitalists say a sluggish economy, slower federal approvals for drugs and medical products and even the popularity of investments in clean energy technologies could be siphoning some dollars from life sciences, which, according to the report, includes drug discovery and medical devices companies.
Some fear less venture money for startup and emerging biotech companies could be a stumbling block in Maryland’s quest to be knighted the next biotech hot spot. As venture capital firms grow more cautious in a tight economy, new jobs and growth in the state’s $29 billion biotech industry are at risk, industry observers say, as are large biotech research park developments in Baltimore. In addition to the UMB BioPark, a new research center is in the works near Johns Hopkins Hospital in East Baltimore.
Meanwhile, Maryland has proposed investing $1.1 billion by 2020 in state programs and incentives to grow the industry. State and regional economic development leaders say Maryland’s proposed investment is the financial bait needed to lure venture capital to the region and will be a lifesaver for companies waiting for an infusion of venture cash.
“Investments are down, but we still want investors to come to our state,” said Larry Mahan, senior strategic advisor for biosciences with the Maryland Department of Business and Economic Development (DBED). “Now is the time to fuel the demand for state incentives for the biotech industry.”
The drop in venture capital investments in metro Washington’s biotech companies follows a nationwide decline in venture capital investments in the life science sector. Venture capital investments throughout the country fell 14 percent in the second quarter to $1.9 billion, compared with $2.2 billion invested in the first quarter, according to the national venture association’s report.
Maryland had 43 venture deals in the life science sector in 2006 for about $286 million, according to PricewaterhouseCoopers. The deal flow dipped to 32 deals for roughly $149 million in 2007. Baltimore-born Amplimmune and Alba Therapeutics raked in a portion of those investments.
“Rather than a go-go time for biotech, it’s a more cautious time,” said Dana Callow, managing general partner for Boston Millennia Partners, a venture capital firm that invests in health care information technology and life sciences.
Decision-making on deals has slowed, he said, as investors take more time to consider risks and returns linked to investments. In the biotech sector, the Food and Drug Administration approval of drugs and products also is taking longer.
Some Maryland biotech executives say the pace of investments is a concern.
“For small companies and startups, the money isn’t there,” said Arkesh Mehta, CEO of Germantown-based Chikujee Therapeutics. Mehta should know; he is looking for $3 million in venture capital.
Mehta said some venture capitalists have told him that if he wants to lure their funds he should move his company to San Diego or Ohio to be closer to the firms’ partners. He said he isn’t considering a move.
The metro Washington region has leaned heavily on early-stage biotech companies coming out of research institutions like Johns Hopkins University and UMB. But some investors are putting more money into later-stage technology that is more ripe for commercialization and a lucrative return on investment.
As the deal flow moves from younger to older companies, local biotech observers say VC investments in this region’s companies could slip further. In response, the region needs to develop more later-stage companies to attract top biotech executives who can spin off new technology and startup companies, said Aris Melissaratos, senior adviser of enterprise development for Johns Hopkins University and former DBED secretary.
2007-09-19
BALTIMORE, Sept. 19 /PRNewswire/ -- Alba Therapeutics Corporation today announced that it has dosed its first patient in a six-week Phase IIb trial with oral AT-1001, an inhibitor of gastrointestinal barrier dysfunction, for the maintenance of remission in patients with Celiac Disease (CD). The multi-center, double-blind, placebo-controlled, dose ranging study will evaluate the efficacy, safety and tolerability of AT-1001 in CD subjects during a six-week gluten challenge, while also testing components of a Celiac Disease activity rating index, a new patient-reported outcomes instrument. "This is Alba's fifth human trial with AT-1001 and highlights our efforts to develop paradigms for the treatment of CD and for the assessment of activity in this neglected disease" stated Dr. Blake Paterson, CEO of Alba. "Since there is no effective treatment for CD and no validated means of measuring disease progression, the successful completion of this study will be a tremendous step forward for Celiac patients."
About Celiac Disease
Celiac Disease ("CD") is a T-cell mediated auto-immune disease that occurs in genetically susceptible individuals and is characterized by small intestinal inflammation, injury and intolerance to gluten. According to the National Institutes of Health, CD affects approximately 3 million Americans. The only current treatment for CD is complete elimination of gluten from the diet, which results in remission for some patients.
About AT-1001
AT-1001 is an inhibitor of barrier dysfunction that has been shown to block intestinal permeability and the genesis of some autoimmune diseases, either as a result of reduction of antigen presentation to the body's immune system, or through some unknown inhibitory, direct effect on gastrointestinal associated lymphoid tissue. AT-1001 is orally formulated, has been granted "Fast Track" designation by the U.S. Food and Drug Administration for the treatment of Celiac Disease, and is also being evaluated for the treatment of Type 1 Diabetes and Crohn's Disease. Results of the Company's first study in celiac patients are available online at:
About Alba
Alba Therapeutics Corporation is a privately held, clinical-stage biopharmaceutical company based in Baltimore, Maryland. Alba is dedicated to development and commercialization of disease-modifying therapeutics to treat autoimmune and inflammatory disease, drug delivery agents and mucosal vaccine adjuvants by exploiting its technology to regulate the assembly and disassembly of tight junctions in cell barriers throughout the body.
Contact: Bernard McDonald, PhD
Phone: 410-319-0780
E-mail: info@albatherapeutics.com
Web site:
Alba Therapeutics Corporation
CONTACT: Bernard McDonald, PhD of Alba Therapeutics Corporation,+1-410-319-0780
Web site:
疫苗快速通道
2005-10-26
BALTIMORE, Oct. 26 /PRNewswire/ -- Alba Therapeutics Corporation ("Alba") today announced successful completion of its first Phase I trial for the drug candidate AT-1001, and that the FDA has granted "Fast Track" designation to AT-1001 for treatment of Celiac Disease (CD). "We are pleased to have concluded our first human study of oral AT-1001 and delighted that the FDA has granted fast track status to AT-1001. These two events are important additional milestones in our efforts to help those suffering from CD, a disease for which there is no effective treatment," said Blake Paterson, MD, President and CEO of Alba. Alba plans to begin a proof of concept study demonstrating efficacy of AT-1001 in celiac patients within the next few months.
Fast track process is designed to facilitate development and expedite the review of new drugs with the potential to address significant unmet medical needs for the treatment of serious or life-threatening conditions. Potential fast track benefits include FDA input into development, submitting new drug applications in sections rather than all at once and the option of requesting Accelerated Approval.
About Celiac Disease
Celiac Disease is a T-cell mediated auto-immune disease that occurs in genetically susceptible individuals and is characterized by small intestinal inflammation, injury and intolerance to gluten. Gluten is a mixture of proteins found in common food grains such as wheat, rye and barley. According to the NIH, CD affects approximately 3 million Americans, although the diagnosis is rarely made. The only treatment for CD is complete elimination of gluten from the diet, which results in remission for some patients.
About Zonulin
Zonulin is an endogenous signaling protein that transiently and reversibly opens the tight junctions ("tj") between the cells of epithelial and endothelial tissues such as the intestinal mucosa, blood brain barrier and pulmonary epithelia. Discovered by Alba co-founder Dr. Alessio Fasano, zonulin appears to be involved in many disease states in which leakage occurs via paracellular transport across epithelial and endothelial tight junctions (tj), and thus may play an important potential role in the treatment of auto-immune diseases.
About Alba
Alba Therapeutics Corporation is a privately held biopharmaceutical company based in Baltimore, Maryland. Alba is dedicated to commercializing disease-modifying therapeutics and drug delivery adjuvants based on the zonulin pathway. Alba's lead molecule, AT-1001, is targeted towards the treatment of Celiac Disease and Type 1 Diabetes.
Contact: Dr. Blake Paterson
Alba Therapeutics Corporation
410-522-8708
Alba Therapeutics Corporation
CONTACT: Dr. Blake Paterson of Alba Therapeutics Corporation,+1-410-522-8708
Web site:
快速通道加速审批
100 项与 Alba Therapeutics Corp. 相关的药物交易
登录后查看更多信息
100 项与 Alba Therapeutics Corp. 相关的转化医学
登录后查看更多信息
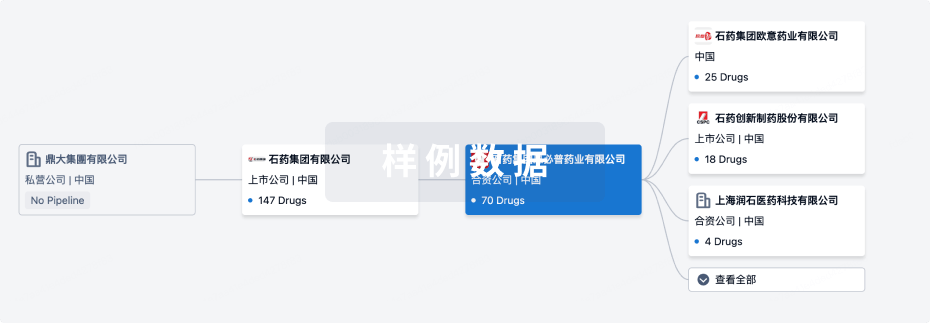
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年09月10日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
其他
4
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
拉雷佐肽 ( EGFR x PAR-2 ) | 克罗恩病 更多 | 无进展 |
AT-1005 | 哮喘 更多 | 无进展 |
AT-1004 | 免疫系统疾病 更多 | 无进展 |
AT-1003 ( haptoglobin ) | 哮喘 更多 | 无进展 |
登录后查看更多信息
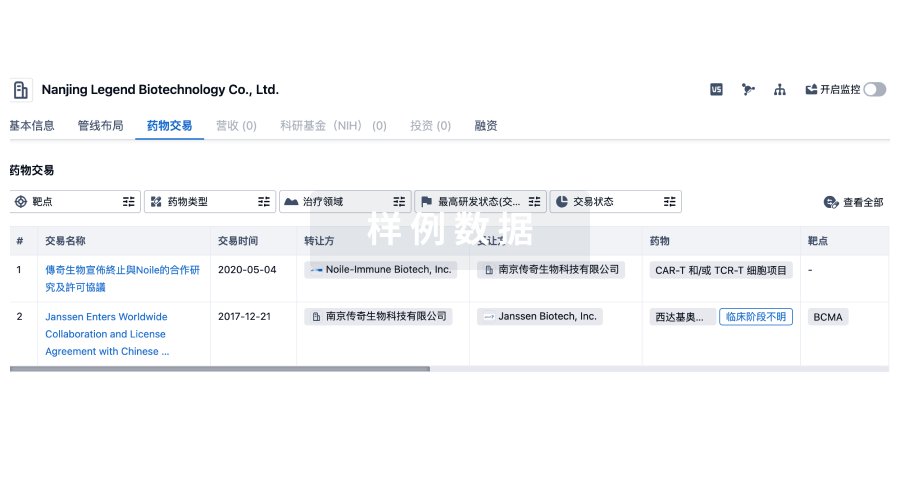
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
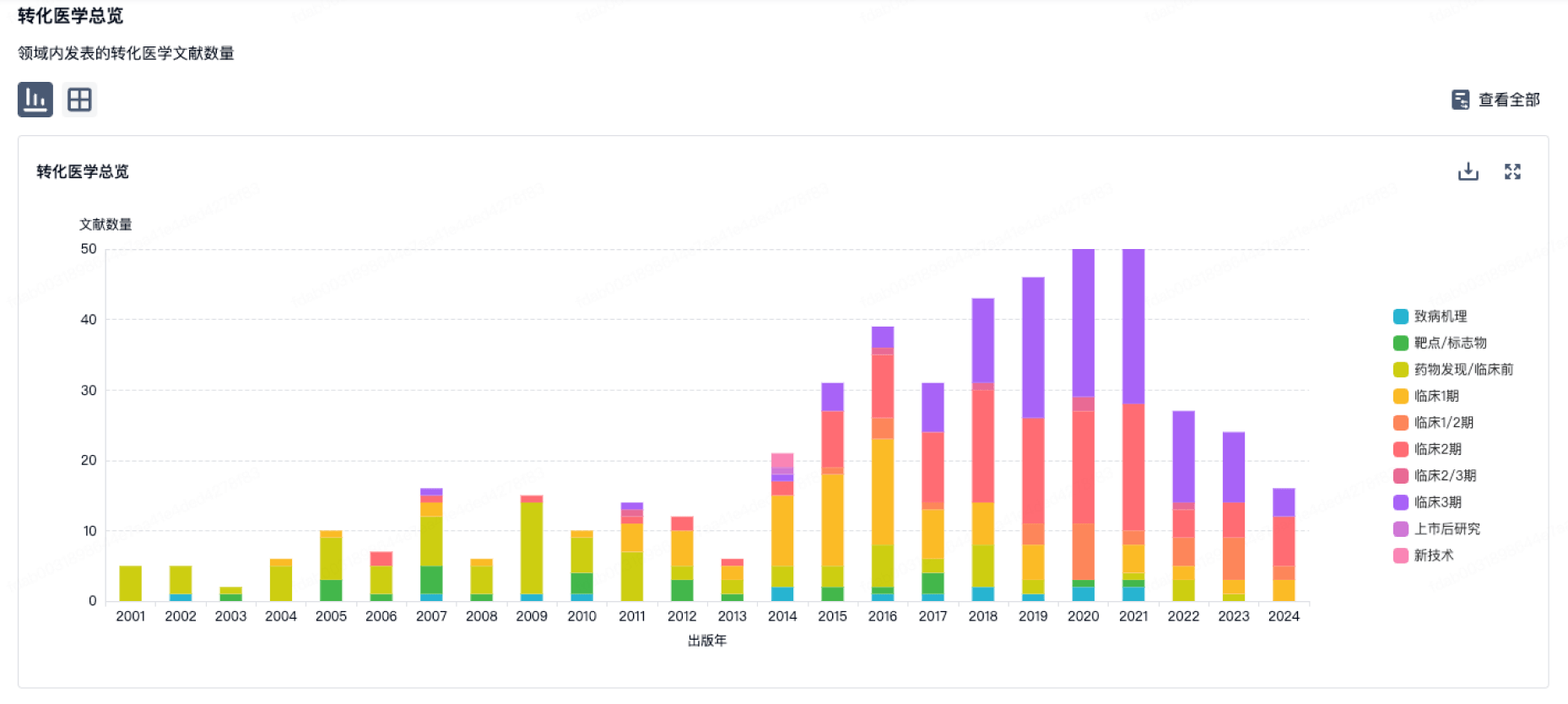
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
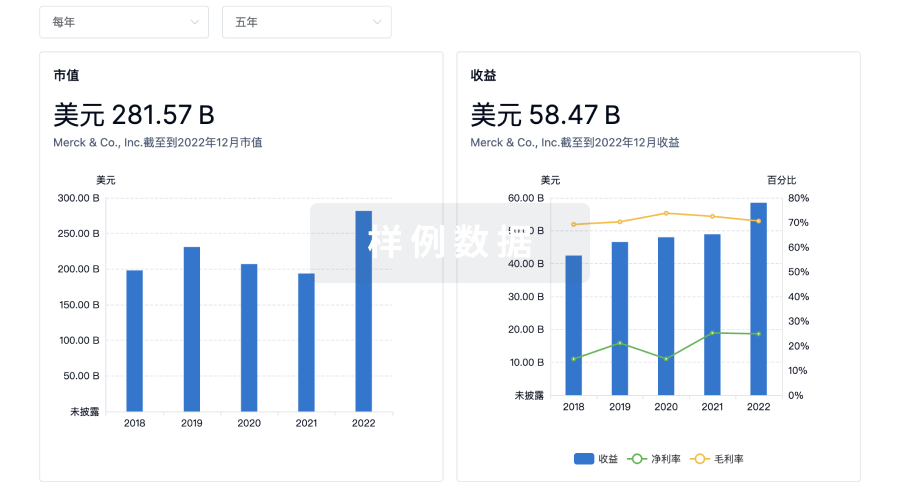
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用