预约演示
更新于:2025-07-06

Hungkuang University
更新于:2025-07-06
概览
标签
皮肤和肌肉骨骼疾病
免疫系统疾病
小分子化药
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 疾病领域 | 数量 |
|---|---|
| 免疫系统疾病 | 1 |
| 排名前五的药物类型 | 数量 |
|---|---|
| 小分子化药 | 1 |
| 排名前五的靶点 | 数量 |
|---|---|
| HSP70 heat-shock proteins x IL-17A | 1 |
关联
1
项与 弘光科技大学 相关的药物作用机制 HSP70热休克蛋白调节剂 [+1] |
原研机构 |
在研适应症 |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期- |
9
项与 弘光科技大学 相关的临床试验NCT06985121
Evaluation of the Scalp Skin Care Effects of Premium Scalp Revitalizing Essence、Premium Scalp Revitalizing Essence 2、Premium Scalp Revitalizing Essence 3
The study aims to evaluate the efficacy of the Premium Scalp Revitalizing Essence on human scalp skin. A total of 60 healthy adults, aged 18 to 60, will be recruited and randomly assigned into five groups receiving different formulations. Participants will use the product once daily for 56 days, and their scalp conditions will be assessed through skin texture tests at multiple time points. Key parameters such as sebum content, overall hair loss, hair density, scalp condition, and hair length will be measured.
开始日期2025-04-08 |
申办/合作机构 |
NCT06914323
The Effects of Acupressure on Pain, Swelling and Comfort in Patients With Femoral Fracture Surgery
Pain is a subjective and unpleasant sensory and emotional experience associated with actual or potential tissue damage. Fractures result from a disruption in the continuity of bone, where bones are subjected to traction, twisting, or compression, causing damage to the surrounding muscular tissues. The treatment of displaced or complex fractures typically requires internal fixation surgery. 89% of fracture patients experience postoperative pain and swelling by the second day following open reduction and internal fixation surgery. These negative sensations can lead to increased pain, limb deformity, and neurovascular compression injuries. If postoperative pain is not adequately managed, it can affect wound healing, increase metabolism and oxygen consumption, and place additional strain on cardiopulmonary function. It is necessary to integrate alternative, non-pharmacological, non-invasive pain relief measures. Effectively and safely alleviating acute postoperative pain can enhance comfort, promote early mobilization, improve adherence to postoperative physical therapy, enhance quality of life and shorten hospital stays.
开始日期2025-02-18 |
申办/合作机构 |
NCT06850935
Evaluation of the Skin Care Effects of Kristen Claire Supreme Rejuvenation Essence
The study evaluates the effects of a skin care formulation containing Centella asiatica extracellular vesicles as the main active ingredient on facial appearance and skin quality in healthy participants.
开始日期2024-09-04 |
申办/合作机构 |
100 项与 弘光科技大学 相关的临床结果
登录后查看更多信息
0 项与 弘光科技大学 相关的专利(医药)
登录后查看更多信息
1,727
项与 弘光科技大学 相关的文献(医药)2025-10-01·BRAIN BEHAVIOR AND IMMUNITY
Variation in anti-SARS-CoV-2 spike antibody responses by variants in patients with severe mental illness after COVID-19 vaccination
Article
作者: Lin, Chun-Yuan ; Yu, Ya-Yen ; Huang, Chih-Chia ; Song, Ying-Chyi ; Yeh, Po-Shou ; Yang, Chin-Chou
Research has shown that patients with psychiatric disorders are more susceptible to contracting SARS-CoV-2 and tend to experience worse outcomes from COVID-19. Therefore, vaccination is strongly suggested for these patients to enhance protection. However, there is limited research on how COVID-19 vaccines induce antibody responses, specifically in individuals with psychiatric conditions. Furthermore, the situation has become more complex with the emergence of variants of concern (VOCs), and the effectiveness of antibody responses against these variants is still poorly understood. To determine whether patients with severe mental illness (SMI) mount an adequate immune reaction to COVID-19 vaccination, we studied the immunization effect of two widely used vaccines, ChAdOx1-S (AstraZeneca) and mRNA-1273 (Moderna), in patients with SMI compared to healthy controls. We enrolled 163 patients with SMI (mainly schizophrenia) and 66 healthy controls, all of whom were negative for previous SARS-CoV-2 infection. We analyzed anti-SARS-CoV-2 spike antibody titers against wild-type (WT), Delta, and Omicron variants after full (two-dose) vaccination with either the ChAdOx1-S or mRNA-1273 COVID-19 vaccines. Patients with SMI exhibited significantly lower mean anti-SARS-CoV-2 spike antibody titers. These results were consistent across different vaccine types and VOCs. Vaccination with ChAdOx1-S consistently induced lower spike-binding antibodies against WT, Delta, and Omicron variants compared to the mRNA-1273 vaccine. While the antibody activities against Omicron are well preserved, they are weaker than those against the WT and Delta variants. Our findings explain why patients with SMI are particularly susceptible to SARS-CoV-2 infection, breakthrough infections, and poorer COVID-19 outcomes.
2025-08-01·COMPREHENSIVE PSYCHIATRY
Mapping psychiatric comorbidity network: A pilot multi-method weighted network analysis with a focus on key disorders
Article
作者: Liu, Yi-Chun ; Huang, Si-Sheng ; Chang, Yu ; Hsu, Wen-Yu
BACKGROUND:
Psychiatric comorbidity is a prevalent phenomenon that imposes a significant burden on patients, healthcare systems, and society. However, current research on psychiatric comorbidity is often limited to single disorders or partial associations. This study aims to utilize network analysis methods to construct a psychiatric comorbidity network and explore the network structural characteristics under different network weight definitions.
METHOD:
Based on the psychiatric outpatient data from Changhua Christian Hospital in Taiwan from January 1, 2016, to June 30, 2024, the ICD-10 diagnostic codes (F00-F99) of all patients that appeared at least three times were extracted. Three different comorbidity networks were constructed using co-occurrence counts, Jaccard index, and partial correlation coefficient estimated by the mixed graphical model (MGM) as the weights of the network edges. Network structure was analyzed using indicators such as degree centrality, modularity, and community detection.
RESULTS:
The dataset included 16,954 patients. The comorbidity frequency network showed that mood disorders (F34) and anxiety disorders (F41) had the highest weighted degree centrality. In the Jaccard coefficient network, the weighted degree centrality of developmental disorders (F8x) increased. The MGM network highlighted the central role of substance use disorders (F1x).
CONCLUSION:
Our findings suggested the roles and interrelationships of different disease categories in the comorbidity network. The results provide new perspectives and data support for clinical practice and future research.
2025-07-01·Journal of Plastic Reconstructive and Aesthetic Surgery
Automated 3D facial smile attractiveness assessment before and after orthognathic surgery using transfer learning: A preliminary study
Article
作者: Chiang, Wen-Chung ; Chen, Hui-Ling ; Lin, Hsiu-Hsia
The aesthetic appearance of the mouth during smiling significantly influences facial attractiveness, thereby, making smile analysis crucial in orthodontics, craniofacial surgery, and cosmetic dentistry. Accurate and quantitative evaluation of facial smile attractiveness is crucial for surgical planning and outcome assessment in orthognathic surgery (OGS). In this study, a transfer learning (TL) model using a convolutional neural network (CNN) based on three-dimensional (3D) contour line features was employed to assess facial smile attractiveness before and after OGS. A retrospective cohort study involving 135 patients was conducted between 2021 and 2024 to compare facial smile attractiveness before and after OGS. Using the 3dMD™ face system, 3D facial photos were captured in a natural head position with forward-facing eyes, relaxed facial muscles, and habitual dental occlusion, before and at least 6 months after surgery. Subsequently, 3D contour images were extracted from these photos for web-based automatic facial smile attractiveness assessment using TL with CNN model. Postoperatively, facial smile attractiveness significantly improved, with scores increasing from 2.62 to 3.27, representing a 25% enhancement as determined by the constructed machine learning model. The web-based system offered clinicians a user-friendly interface, providing rapid assessment of results and serving as an effective tool for doctor-patient communication. This study marks the first attempt to automatically evaluate facial smile attractiveness before and after surgery in an objective and quantitative manner, using a machine learning model based on the 3D contours feature map.
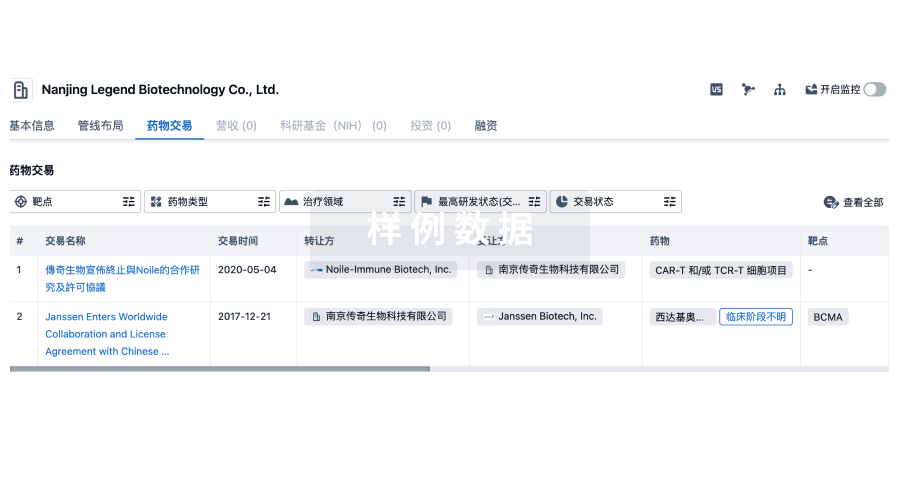
100 项与 弘光科技大学 相关的药物交易
登录后查看更多信息
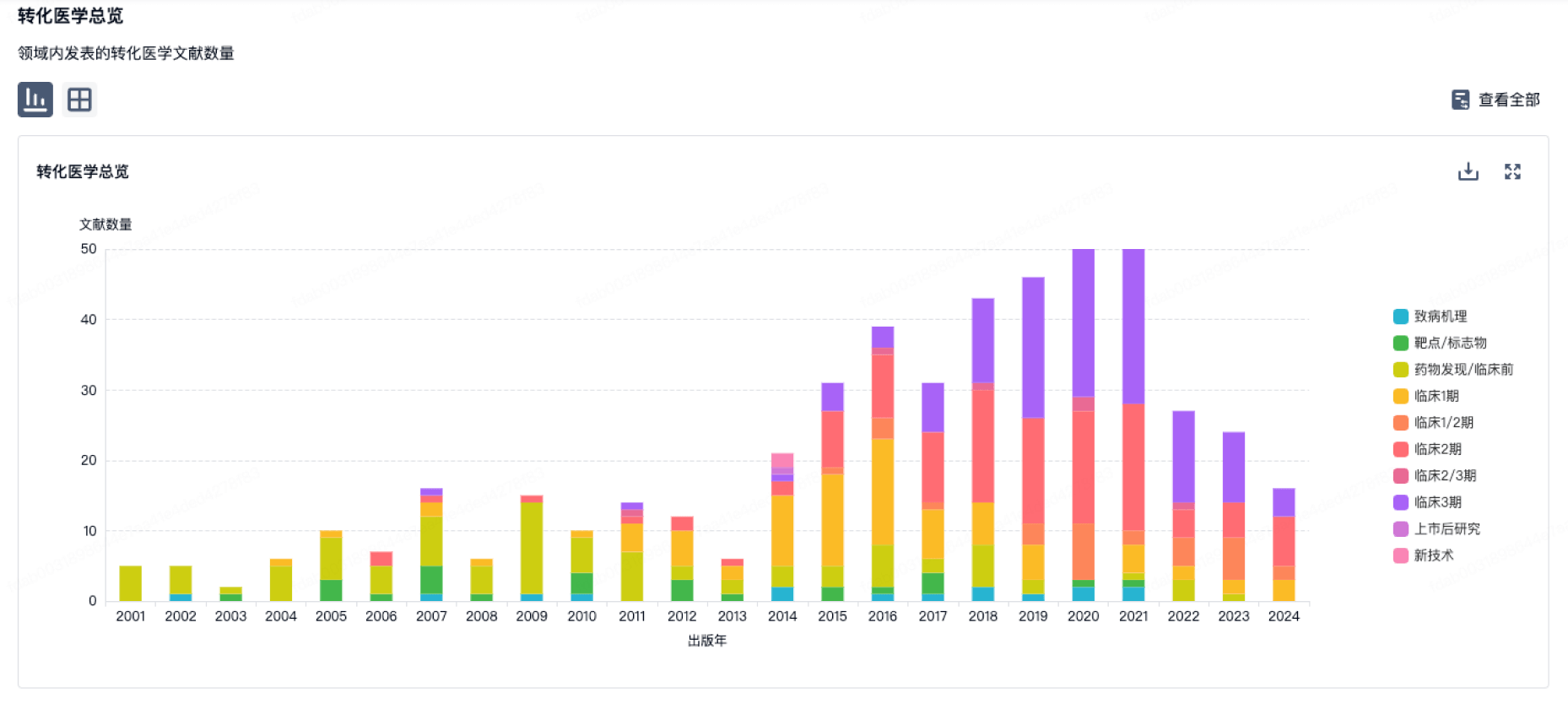
100 项与 弘光科技大学 相关的转化医学
登录后查看更多信息
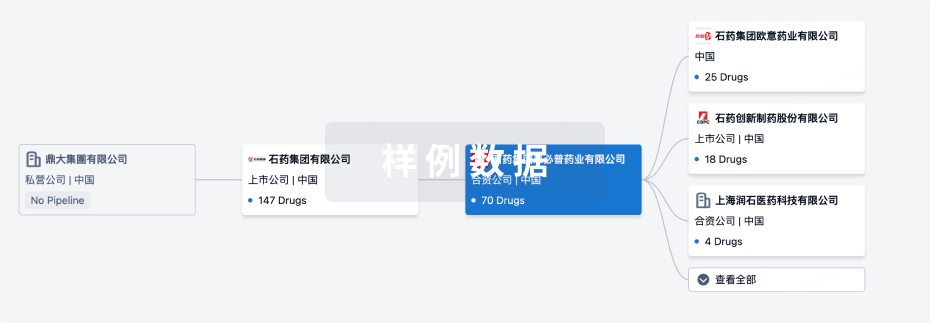
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年07月07日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
临床前
1
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
Brevilin A ( HSP70 heat-shock proteins x IL-17A ) | 银屑病 更多 | 临床前 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
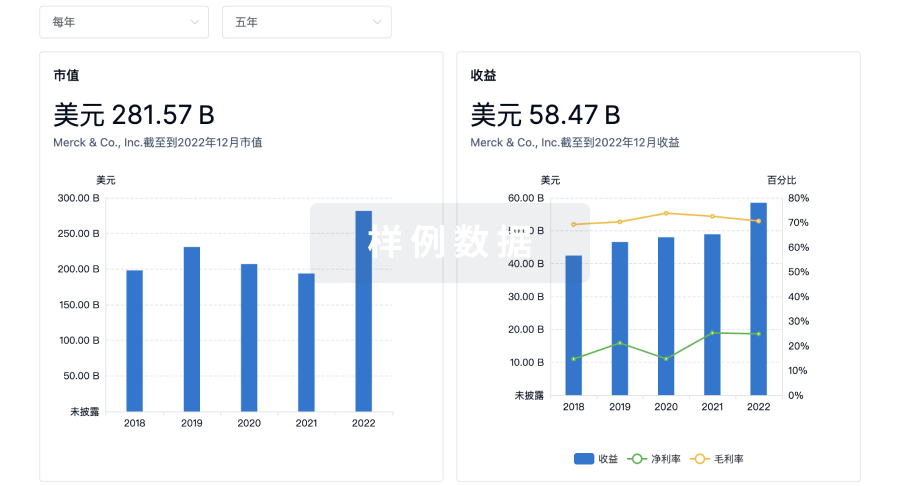
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用

