预约演示
更新于:2025-01-23

Pacific Center For Reproductive Medicine
更新于:2025-01-23
概览
关联
3
项与 Pacific Center For Reproductive Medicine 相关的临床试验NCT02106689
Needle Free Injections of Gonadotropins for Patients Undergoing Superovulation - A Randomized, Pilot Study
The daily injections required for superovulation, a fertility treatment using injections to stimulate a women's ovaries to produce multiple eggs, can be an anxiety provoking process for many women and a deterrent to treatment. Alternative needle-free injection systems have been developed with the intention of reducing needle phobia and pain, while providing similar results. However, these needle-free systems are not yet being widely used for women with infertility.
The purpose of this study is to assess whether the pain and apprehension patients often associate with needles and injections, can be alleviated by using a new, Health Canada approved, needle-free system. The purpose of the current study is to assess whether patient satisfaction is improved in patients using a needle free injection system for the daily self injections required for superovulation induction as compared to patients using the standard needle and syringe.
The purpose of this study is to assess whether the pain and apprehension patients often associate with needles and injections, can be alleviated by using a new, Health Canada approved, needle-free system. The purpose of the current study is to assess whether patient satisfaction is improved in patients using a needle free injection system for the daily self injections required for superovulation induction as compared to patients using the standard needle and syringe.
开始日期2014-02-01 |
申办/合作机构 |
NCT01983423
Effect of Endometrial Biopsy on in Vitro Fertilization Pregnancy Rates - a Randomized, Multicenter Study
Animal and clinical studies have suggested that local tissue trauma can promote the process of an embryo implanting in the uterine cavity. The clinical studies have been performed in patients with a history of previously failed treatments using in vitro fertilization; a process of stimulating many eggs from a women and removing them from the body, to allow fertilisation with sperm to occur in a laboratory setting. The embryos are then replaced into the uterine cavity.
This study questions whether endometrial biopsy (placing a small straw like catheter through the cervix and into the uterine cavity to take a sample of tissue via suction into the bore of the catheter), within 5-10 days of starting a cycle of in vitro fertilization, will improve pregnancy outcome for patients in the first or second cycle of treatment. The hypothesis is that endometrial biopsy will improve pregnancy outcome.
The study is a randomized multicentre study involving 3 Canadian fertility centres.
This study questions whether endometrial biopsy (placing a small straw like catheter through the cervix and into the uterine cavity to take a sample of tissue via suction into the bore of the catheter), within 5-10 days of starting a cycle of in vitro fertilization, will improve pregnancy outcome for patients in the first or second cycle of treatment. The hypothesis is that endometrial biopsy will improve pregnancy outcome.
The study is a randomized multicentre study involving 3 Canadian fertility centres.
开始日期2013-01-01 |
NCT01616225
Adjuvant Growth Hormone in Infertile Women With Prior Poor IVF Response: a Randomized, Controlled, Open-label Study
This study (the "Adjuvant Growth Hormone Study") is being done to see the effects of adding Growth Hormone (GH) during fertility treatment (also called in vitro fertilization or IVF). Growth Hormone is a protein that your body normally produces. Growth Hormone can act on several different organs, including the ovaries, where eggs are made. From evidence gathered from studies done by fertility doctors over the years, researchers believe that women who have not become pregnant through IVF in the past might have better results if they go on a course of Growth Hormone during the IVF treatment. However, more research needs to be done to confirm whether adding Growth Hormone is beneficial and also to find out the best time to start Growth Hormone treatment during IVF.
We hope that our Adjuvant Growth Hormone study will help answer these questions.
We hope that our Adjuvant Growth Hormone study will help answer these questions.
开始日期2012-06-01 |
申办/合作机构 |
100 项与 Pacific Center For Reproductive Medicine 相关的临床结果
登录后查看更多信息
0 项与 Pacific Center For Reproductive Medicine 相关的专利(医药)
登录后查看更多信息
25
项与 Pacific Center For Reproductive Medicine 相关的文献(医药)2023-09-27·2023 IEEE 25th International Workshop on Multimedia Signal Processing (MMSP)
Time Series Classification for Modality-Converted Videos: A Case Study on Predicting Human Embryo Implantation from Time-Lapse Images
作者: Abbasi, Mehryar ; Saeedi, Parvaneh ; Havelock, Jon ; Au, Jason
2022-12-01·Microbiome1区 · 生物学
Endometrial microbiota composition is associated with reproductive outcome in infertile patients
1区 · 生物学
ArticleOA
作者: Simon, Carlos ; Chavez, Alejandro ; Leondires, Mark ; Gomez, Carlos ; Dimattina, Michael ; Bau, Davide ; Izquierdo, Alexandra ; Bahçeci, Mustafa ; Seethram, Ken ; Gonzalez-Monfort, Marta ; Lim, Mei Wei ; Taguchi, Sagiri ; Meneghini, Georgina ; Barrionuevo, Marcelo J ; Garcia-Grau, Iolanda ; Vilella, Felipe ; Aubuchon, Mira ; Moreno, Inmaculada ; Valbuena, Diana ; Puente, Elena ; Perez-Olgiati, Martina ; Perez-Villaroya, David
2022-09-01·Breast Cancer Research and Treatment
Risk of recurrence and pregnancy outcomes in young women with breast cancer who do and do not undergo fertility preservation
Article
作者: Perdizet, Kirstin ; Lim, Chloe ; Tesch, Megan E ; Wang, Ying ; Lohrisch, Caroline A ; Lee, Shaina ; Warner, Ellen ; Yokom, Dan ; Xu, Ying Hui ; Roberts, Jeffery
100 项与 Pacific Center For Reproductive Medicine 相关的药物交易
登录后查看更多信息
100 项与 Pacific Center For Reproductive Medicine 相关的转化医学
登录后查看更多信息
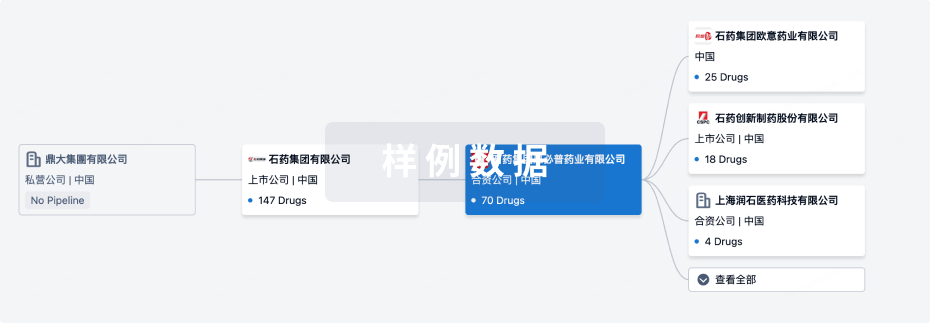
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年04月02日管线快照
无数据报导
登录后保持更新
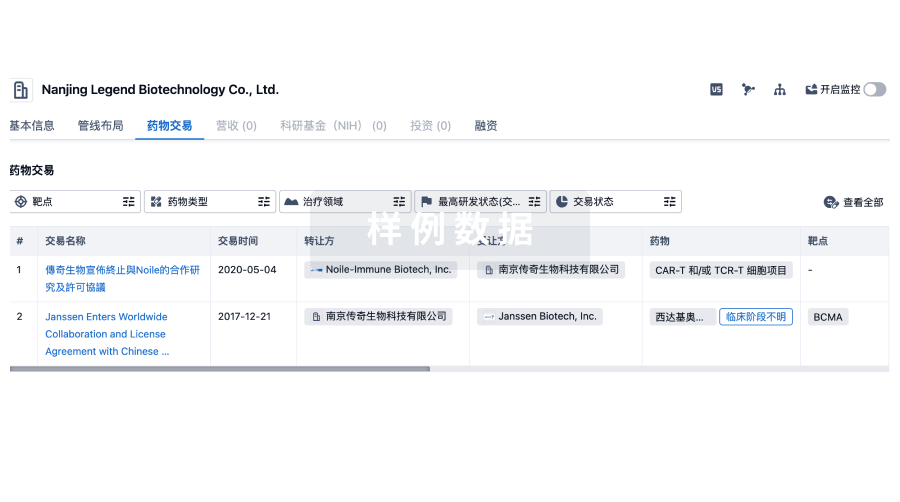
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
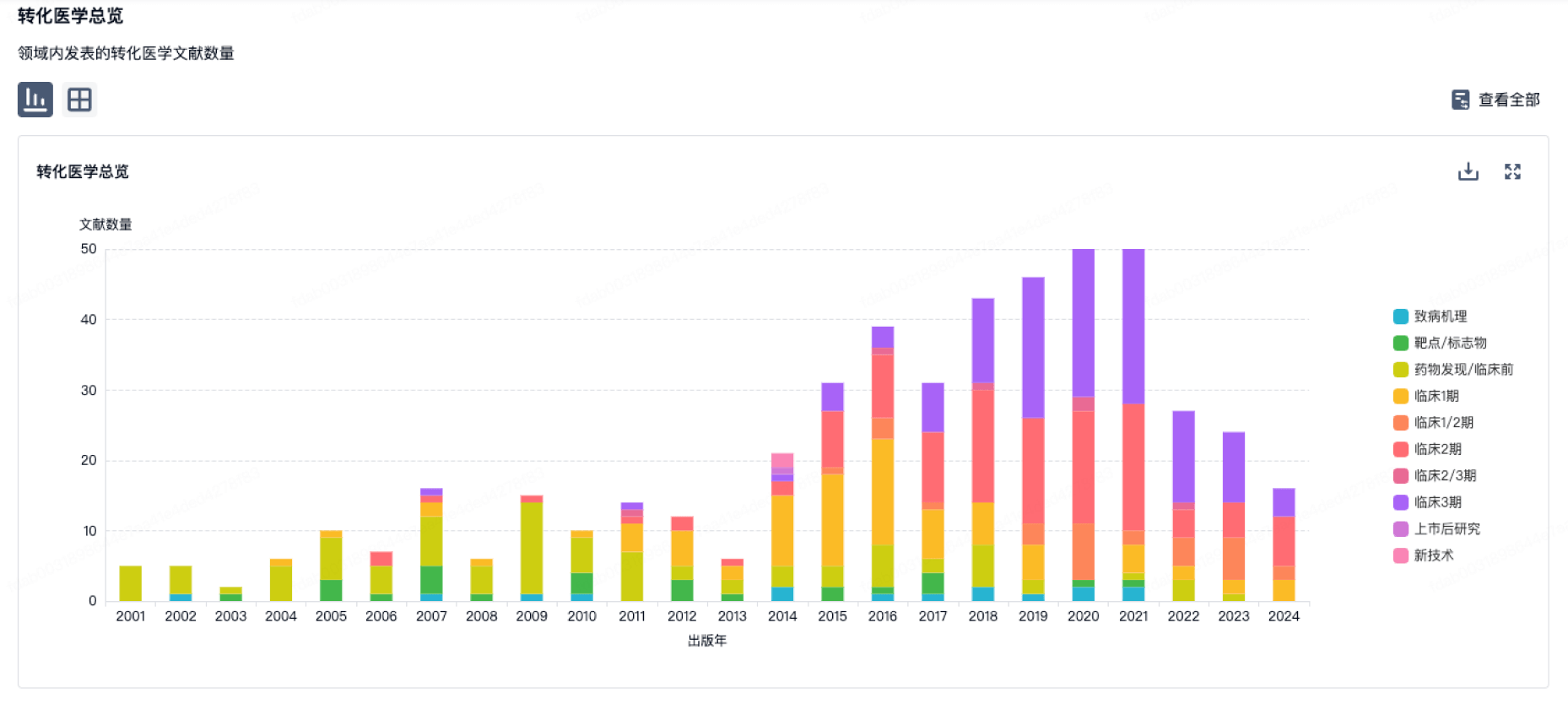
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
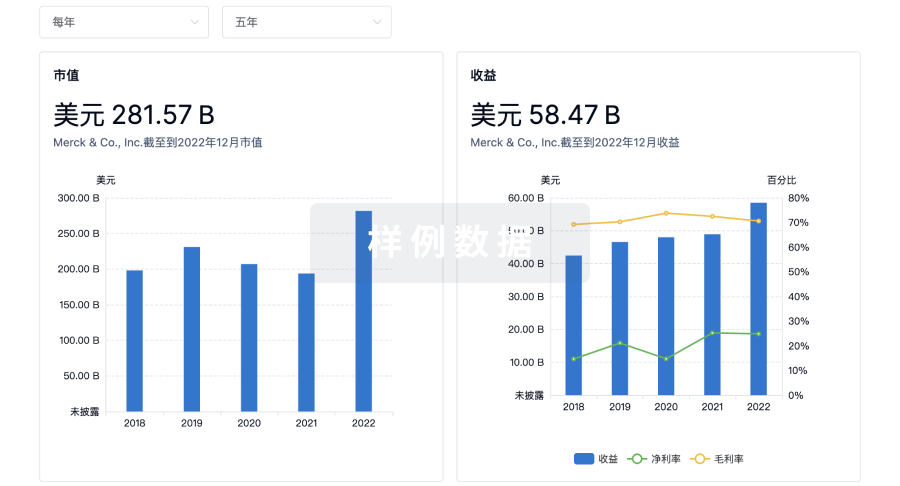
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
来和芽仔聊天吧
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
