预约演示
更新于:2025-05-07
Chongqing Public Health Medical Center
更新于:2025-05-07
概览
关联
17
项与 Chongqing Public Health Medical Center 相关的临床试验NCT05256459
Clinical Intervention Strategy for High-risk Hepatitis B Related Hepatocellular Carcinoma Based on Liquid Biopsy Screening Technique
This study aims to explore whether there is difference in the incidence rate and incidence rate of HCC in patients with chronic hepatitis B who are screened for high risk of liver cancer. Whether the timely intervention can be used to reduce the incidence of HCC for the early screening and early warning patients can provide evidence-based medical evidence for the selection or adjustment of anti HBV drugs in high-risk patients with liver cancer. To provide evidence for whether patients with liver nodules at high risk of liver cancer need to deal with liver nodules in advance.
开始日期2022-05-10 |
申办/合作机构  重庆医科大学附属第二医院 重庆医科大学附属第二医院 [+1] |
ChiCTR2200058014
Pharmacokinetics, Safety and Efficacy of Albuvirtide in HIV-1 Patients with End Stage Renal Disease Requiring Hemodialysis
开始日期2022-04-25 |
NCT05265507
Comparison of Anti-nausea and Vomiting Effect After Elective Surgery Undergoing General Anesthesia Between Glycopyrronium and Ondansetron: a Multi-center Study
To compare the anti-nausea and vomiting effect between glycopyrronium and ondansetron for patients receiving elective surgery under general anesthesia. Based on this study the investigators intend to explore the feasibility of using glycopyrronium to prevent postoperative nausea and vomiting.
开始日期2022-03-21 |
申办/合作机构  重庆医科大学附属第二医院 重庆医科大学附属第二医院 [+5] |
100 项与 Chongqing Public Health Medical Center 相关的临床结果
登录后查看更多信息
0 项与 Chongqing Public Health Medical Center 相关的专利(医药)
登录后查看更多信息
452
项与 Chongqing Public Health Medical Center 相关的文献(医药)2025-12-31·Cell Adhesion & Migration
Brief biology and pathophysiology of Tekt bundles
Review
作者: Liu, Wei ; Ni, Bing ; Yu, Zhongying ; Cheng, Yimei ; He, Wenjuan ; Wang, Xiao ; Miao, Hongming ; Zhang, Qinghua ; Yin, Jun ; Liu, Min ; Bai, Jialian
2025-04-09·Journal of Clinical Microbiology
Nanopore sequencing for precise detection of
Mycobacterium tuberculosis
and drug resistance: a retrospective multicenter study in China
Article
作者: Liu, Ning ; Gu, Hongcang ; Yu, Shanshan ; Xu, Peisong ; Li, Liang ; Wang, Yunfei ; Sun, Jinhao ; Li, Peibo ; Zhu, Qingdong ; Gao, Weiwei ; Wang, Hua ; Pang, Yu ; Liu, Fuyou ; Xie, Zhouhua ; Li, Haoran ; Zeng, Yi ; Wang, Qian
2025-04-01·Naunyn-Schmiedeberg's Archives of Pharmacology
Inhibitory effects characteristics of polysaccharide of Polygonati Rhizome on cytochrome P450 enzymes
Article
作者: Wang, Ruidong ; Zhu, Lijun ; Zai, Jian ; Wang, Xiaohong ; Du, Yue ; Fu, Yao ; Duan, Yan ; Zuo, Tian ; Zhan, Qi
1
项与 Chongqing Public Health Medical Center 相关的新闻(医药)2024-06-26
2024年5月,全球首位被CAR-T免疫细胞疗法治愈的女孩Emily已经无癌生存12周年。每一年,Emily都会在社交平台分享自己的抗癌照,如今的她,已进入名校宾夕法尼亚大学求学,除了“CAR-T抗癌治愈第一位患者”的身份,她也成为细胞免疫疗法治愈癌症的代言人,把创新药物治疗的慰藉、抗癌过程的勇气和信心传递给全世界。
图1 Emily历年抗癌打卡照
CAR-T疗法虽然取得了巨大的成功,也面临着一些挑战,主要与副作用、T细胞耗竭和恶性肿瘤微环境(TME)等有关。在放大生产中的制造过程目前既耗时又昂贵,因此,使尽可能多的患者接受CAR-T细胞免疫治疗成为一个更大的挑战。
图2 CAR-T疗法面临的挑战
CAR-T疗法的升级版本CAR-NK疗法因其机制上具有更强的肿瘤特异性靶向性和细胞毒性、NK细胞获取更廉价易得、大规模生产周期短、对实体瘤治疗效果更好等优势,近年来获得学术圈和药企的广泛关注。
在智慧芽新药情报库中输入关键词CAR-NK可以得到最近30日的包括药物、适应症、靶点、机构、临床试验、临床结果、转化医学、药物交易等多条信息。为了查找信息方便、全面,可以通过芽仔将页面内容整理成报告导出。
图3 智慧芽新药情报库搜索CAR-NK
根据导出的报告将关键信息概括如下。CAR-NK这种新型的免疫细胞治疗技术,具有以下优势:1.由自然杀伤细胞改造而成,具有更低的毒副作用和更高的安全性;2.对于肿瘤细胞的识别和杀伤能力更强,治疗效果更显著;3.更容易实现个性化治疗,适用范围更广。 然而,CAR-NK技术也存在一些缺点,包括:1.目前研究和临床应用仍处于早期阶段,需要更多的时间和资源来完善和验证;2.相对于CAR-T技术,CAR-NK的研究和发展相对滞后,市场竞争压力较大,也蕴藏着机会。
药物
靶点
药物
类型
在研机构
适应症
最高
阶段
AB-101(Artiva Biotherapeutics)
CAR-NK
Artiva Biotherapeutics, Inc., Affimed GmbH
CD30阳性外周T细胞淋巴瘤, 复发性霍奇金淋巴瘤, 难治性霍奇金淋巴瘤
临床2期
NKG2D-ACE2 CAR-NK cell therapy(Sidemu Biotechnology Technology)
NKG2D
CAR-NK
重庆市公共卫生医疗中心, 斯德姆生物
新型冠状病毒感染
临床2期
AB-201(Artiva Biotherapeutics)
HER2
CAR-NK
Artiva Biotherapeutics, Inc., GC Cell Corp.
乳腺癌, 胃食管交界处腺癌, HER2阳性实体瘤
临床1/2期
Anti-BCMA CAR-NK(Shahid Beheshti University of Medical Sciences)
BCMA
CAR-NK
Shahid Beheshti University of Medical Sciences
浆细胞骨髓瘤难治
临床1/2期
CAR.70/IL15-transduced CB-NK cells(M.D. Anderson Cancer Center)
CD70 x IL15R
CAR-NK
The University of Texas MD Anderson Cancer Center
晚期肾细胞癌, 间皮瘤, 骨肉瘤
临床1/2期
CD123 targeted CAR-NK cells(Chongqing Precision Biotech)
CD123
CAR-NK
重庆精准生物技术有限公司
急性髓性白血病, Blastic浆细胞样树突状细胞肿瘤
临床1/2期
dualCAR-NK19/70 cell(Shanghai Tongji Hospital)
CD19 x CD70
CAR-NK
上海市同济医院
复发性B细胞淋巴瘤, 难治性B细胞淋巴瘤
临床1/2期
INKmune
CAR-NK
INmune Bio, Inc.
转移性去势抵抗性前列腺癌, 急性髓性白血病, 难治性贫血伴原始细胞过多
临床1/2期
SAR445514
BCMA x CD16a x NKp46
CAR-NK
Sanofi, Innate Pharma SA
免疫球蛋白轻链淀粉样变性, 浆细胞骨髓瘤难治, 复发性多发性骨髓瘤
临床1/2期
Sitocabnagene loxiveluecel
CD19
CAR-NK
The University of Texas MD Anderson Cancer Center, Takeda Pharmaceutical Co., Ltd.
急性淋巴细胞白血病, B细胞淋巴瘤, 慢性淋巴细胞白血病
临床1/2期
据智慧芽新药情报库统计,截止2024年06月25日,全球共有256个CAR-NK药物,来自144个机构,覆盖69个靶点和124个适应症,开展101个临床试验。 研发进度靠前的Top 10药物如上表。
下文将根据CAR-NK机制的不同介绍其具体治疗优势以及靶点、适应症上出现的一些新机会。
图4 NK细胞来源广泛
NK细胞是免疫系统中的一种淋巴细胞,在人体抵御肿瘤和病毒感染方面起着至关重要的作用。NK细胞在功能上类似于CD8+细胞毒性T细胞,并通过类似的细胞毒性机制杀死靶细胞,但缺乏体细胞重排和抗原特异性的TCR。人白细胞抗原(HLA)表达较低的肿瘤细胞可能更容易受到NK细胞的杀伤,这是由于KIR介导的抑制作用降低。
如图4所示,NK细胞可以来自多种来源,如外周血单个核细胞、脐带血、永生化细胞系、造血干细胞和祖细胞(HSPCs)以及诱导多能干细胞(iPSCs)。
由于癌症患者的自体NK细胞表型失调,异体NK细胞往往优于自体NK细胞。NK细胞系如NK- 92mi也已被批准装载CAR结构以创建CAR-NK治疗系统并应用于临床。这进一步增加了NK细胞的来源和可用性。
图5 CAR-NK细胞治疗过程
NK-92细胞与其他来源的NK细胞相比,具有可预测的增殖动力学,可以在生物反应器中生长,在几周内产生数十亿个细胞。此外,NK细胞系可以很容易地高效转导。已经产生了表达CAR的NK-92靶向几种癌症表面受体,如CD19(一种B细胞受体),人表皮生长因子受体2(HER2/ErbB2)和表皮生长因子受体(EGFR)且许多这些经过改造的NK-92细胞目前正在临床试验中用于治疗癌症。CAR-NK细胞被改造成识别和攻击存在于癌细胞中的特定抗原。图5显示了以PBMC为例的CAR-NK细胞治疗过程。
多数肿瘤可能会产生几种不同的基因突变,其中一些可能更容易导致癌细胞扩散到身体的其他部位。例如,表皮生长因子受体的突变(EGFR)已被确定为转移的关键驱动因素,并且已经开发出安全有效的治疗方法来靶向EGFR突变并抑制癌症扩散。这些靶点也可以作为设计CAR-NK治疗抗原识别区域的基础。图6列出的一些靶点都是一些CAR-NK细胞疗法可潜在靶向的靶点。如HER2、EGFR、PD-L1、ROR1、GD2、MSLN等。
图6 CAR-NK可靶向靶点治疗肺癌等
那么CAR-NK和CAR-T有什么异同呢?二者都是通过利用人体的免疫系统来瞄准并摧毁癌细胞,从而彻底改变癌症治疗。与CAR-T相比,CAR-NK疗法最显著的优势之一是其固有的高特异性靶向癌细胞的能力,同时最大限度地减少脱靶效应。表1为CAR-T和CAR-NK技术的比较。NK细胞具有区分健康细胞和恶性细胞的天然能力,从而降低自身免疫反应和附带损伤的风险。并且,CAR-NK疗法在治疗实体肿瘤(如肺癌)方面已经证明了有前景的疗效,这对其他形式的免疫疗法来说是一个重大挑战。NK细胞浸润实体瘤的天然能力,结合CAR靶向的特异性,为实体瘤患者提供了一种有效的治疗方法。
与CAR-T疗法不同,CAR-NK疗法表现出更高的治疗安全性。CAR-t细胞疗法与细胞因子释放综合征(CRS)有关,这是一种潜在的致命免疫反应。CAR-NK细胞显示出较低的诱导CRS的倾向,使CAR-NK治疗成为一种更安全的选择。这种降低的风险提高了患者的安全性,并使其在临床环境中具备更广泛的适用性。
表1 CAR-T和CAR-NK对比
细胞治疗中细胞的来源往往成为限制临床应用的一个制约因素。CAR-T细胞通常是自体的(来自患者),这限制了它的推广。目前,许多公司试图制造现成的产品CAR-T细胞,如使用诱导多能干细胞(iPSCs)分化T细胞,正在开发中。与T细胞不同,NK细胞可以从同种异体来源(供体)中获得,这使得它们很容易“现成”使用。这种同种异体的能力大大减少了与CAR-NK细胞治疗相关的时间和成本,使其更容易被更广泛的患者群体所接受。NK细胞的主要来源包括外周血、脐带血、NK细胞系和诱导多能干细胞(iPSCs)。外周血是用于治疗目的的NK细胞最传统的来源。来源于外周血的NK细胞很容易获得,可以从患者(自体)或供体(异体)收集。外周血采集相对简单,自体使用可将免疫排斥的风险降至最低。除了外周血,还有脐带血(UCB)是NK细胞的另一种来源,由于其独特的性质而被探索。ucb来源的NK细胞表现出更高的不成熟程度,这导致输注后更好的扩增和长寿命。当异体使用时,它们引起移植物抗宿主病(GvHD)的风险也较低。
表1续CAR-T和CAR-NK对比
除了上述自然衍生的NK细胞外,通过细胞工程方法获得的NK细胞也已被证明能够装载CAR结构来构建CAR-NK疗法。iPSCs代表了NK细胞的尖端来源,能够分化成任何细胞类型,包括NK细胞。iPSCs提供了取之不尽的NK细胞来源,可以通过基因工程来增强其抗癌特性。虽然分化过程复杂且成本高昂,但ipsc衍生的NK细胞的长期安全性仍有待完全确定。一些人类NK细胞系,如NK-92,已经被基因改造以表达用于治疗。NK细胞系提供了一致和无限的NK细胞来源,可以很容易地在体外进行工程和扩增。细胞系源的使用使扩张和包装过程变得容易。同时,还能降低工程细胞的批效应和不稳定性。
总结
CAR- NK细胞疗法是治疗癌症的一个很有前途的途径,与传统疗法相比,它具有潜在的优势,包括降低CRS和GvHD的风险,以及通过先天免疫机制靶向和杀死癌细胞的能力。解决TME抑制、CAR-NK细胞持久性、抗原逃逸和可扩展性的挑战对于CAR-NK细胞疗法的成功开发和临床实施至关重要。
利用基因工程、免疫学和制造技术的进步,CAR-NK细胞疗法在提高疗效、安全性和可及性方面具有巨大潜力,有望为癌症患者带来新的希望。
参考文献:
1.https://mp.weixin.qq.com/s/NHPKOJts53CKlfgTeTKLaw.
2.Xiao song, et al;Advances in CAR-NK cell therapy for lung cancer: is it a better choice in the future? DOI 10.3389/fonc.2024.1390006.
3.Zhang et al, (2022). CAR-NK cells for cancer immunotherapy: from bench to bedside. Biomarker Research,https:/doi.org/10.1186/s40364-022-00364-6.
点击图片,免费GET海量新药信息
👇👇👇
免疫疗法细胞疗法临床2期临床1期
100 项与 Chongqing Public Health Medical Center 相关的药物交易
登录后查看更多信息
100 项与 Chongqing Public Health Medical Center 相关的转化医学
登录后查看更多信息
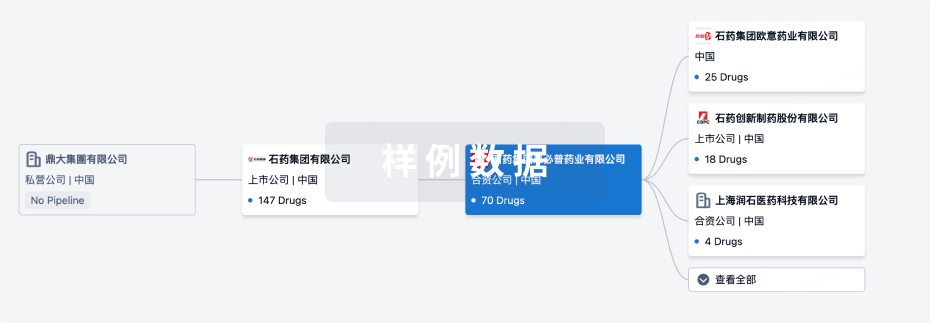
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年06月28日管线快照
无数据报导
登录后保持更新
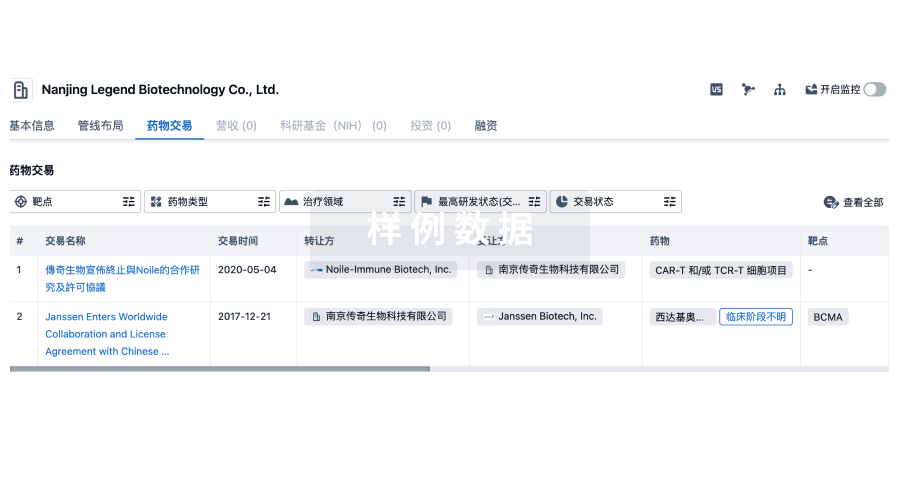
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
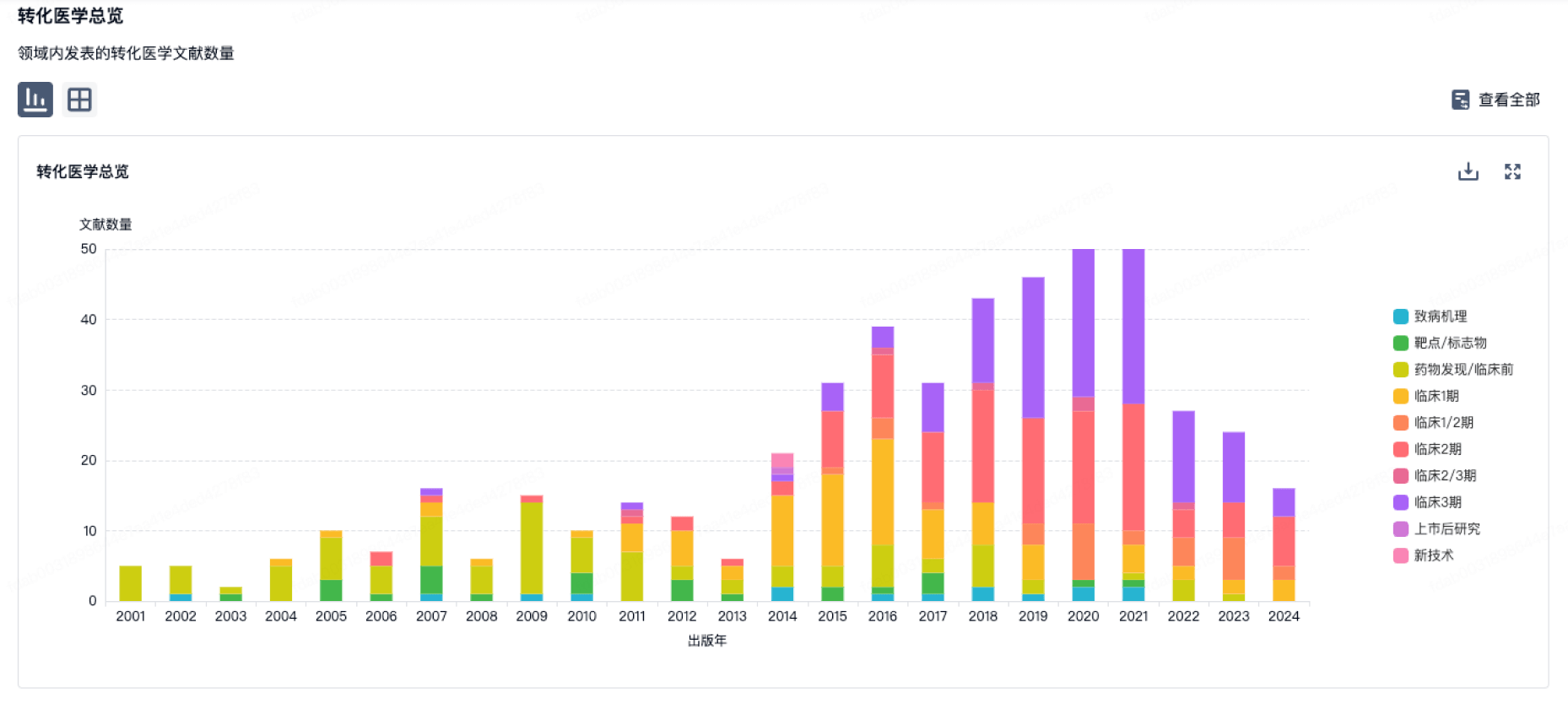
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
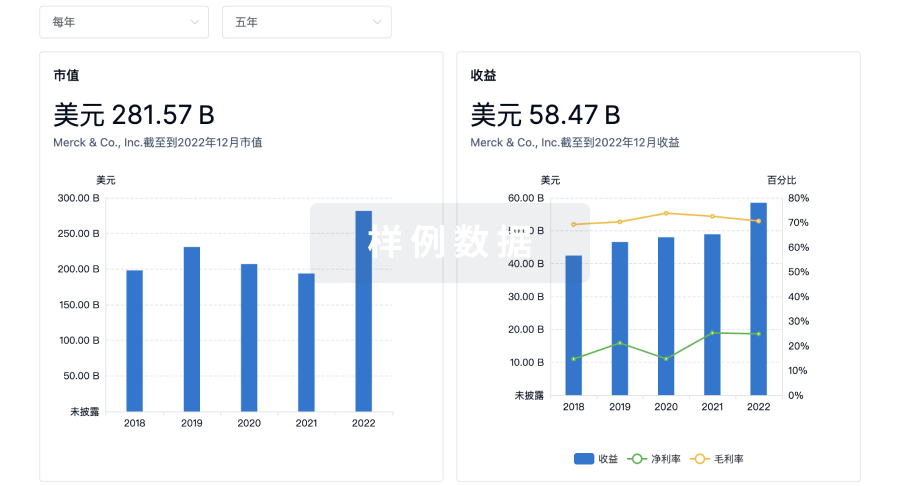
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用