预约演示
更新于:2025-07-06

Centre Hospitalier Universitaire de Grenoble
更新于:2025-07-06
概览
标签
肿瘤
其他疾病
感染
小分子化药
单克隆抗体
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 小分子化药 | 1 |
| 单克隆抗体 | 1 |
| 排名前五的靶点 | 数量 |
|---|---|
| BET(溴结构域和超末端结构蛋白家族) | 1 |
关联
2
项与 Centre Hospitalier Universitaire de Grenoble 相关的药物靶点- |
作用机制- |
在研适应症 |
非在研适应症- |
最高研发阶段临床阶段不明 |
首次获批国家/地区- |
首次获批日期- |
WO2022248475
专利挖掘靶点 |
作用机制- |
非在研适应症- |
最高研发阶段药物发现 |
首次获批国家/地区- |
首次获批日期- |
865
项与 Centre Hospitalier Universitaire de Grenoble 相关的临床试验NCT06960356
Development of Follow-up Nursing Consultations for Children at Risk of Post-resuscitation Syndrome
The investigator hypothesize that, during an IPDE consultation 3 months after discharge from critical care, the investigator will identify PTSD in approximately one-third of children, and show an association between this syndrome and quality of life in children admitted to pediatric intensive care.
开始日期2025-12-01 |
NCT07031089
City-hospital Collaboration for the Early Screening of Hepatic Fibrosis in Primary Care: a Secondary Prevention Project in the Grenoble Health Basin
Cirrhosis and hepatocellular carcinoma (HCC) are responsible for 25,000 deaths per year in France. The main causes are excessive alcohol consumption, metabolic steatosis, and hepatitis B and C. Fibrosis, classified from F0 (absence of fibrosis) to F4 (cirrhosis), is the sole determinant of liver-related mortality, particularly from stage F3. The incidence of metabolic steatosis is increasing, associated with a rise in mortality from chronic liver diseases (CLD). CLDs, often asymptomatic, are diagnosed late, reducing patient survival. Recommendations exist for the screening of hepatic fibrosis in at-risk patients (alcohol, diabetes, metabolic syndrome). This screening relies on calculating the FIB-4 score (calculated from widely prescribed variables: AST, ALT, platelets, age), followed by Fibroscan® (a non-invasive test for hepatic fibrosis) if FIB-4 > 1.3.
A Fibroscan® result <8kPa excludes advanced fibrosis, while a result >9.6kPa suggests advanced fibrosis and ≥15kPa indicates cirrhosis. The appropriate care pathway includes a risk reduction program, a specialized consultation for patients with Fibroscan® ≥8kPa, and semi-annual screening for HCC in the case of cirrhosis. Indeed, it has been shown in a French cohort of patients with viral C cirrhosis that adherence to semi-annual screening is associated with better survival.
Eligible patients are primarily seen in primary care, and INCA has published a recommendation intended for general practitioners to improve the screening of fibrosis [13]. However, FIB-4 is poorly known among general practitioners [14], and access to Fibroscan® remains limited [15], hindering the implementation of the recommendations. Therefore, a care pathway has been established in the Grenoble area, initiated by Professor Costentin, in collaboration with Dr. Hyerle (CPTS Sud Est Grenoblois), allowing access to Fibroscan® for patients in primary care, starting from 2022 at the CHU, and then in 2024 at the CPTS. Dr. Hyerle has been trained in the use of Fibroscan® and training sessions have been organized to promote this pathway to practitioners in Grenoble. The objective is to evaluate the completion of the pathway, particularly the management of MCF risk factors and referral to specialized consultation for patients with Fibroscan® ≥8 kPa.
A Fibroscan® result <8kPa excludes advanced fibrosis, while a result >9.6kPa suggests advanced fibrosis and ≥15kPa indicates cirrhosis. The appropriate care pathway includes a risk reduction program, a specialized consultation for patients with Fibroscan® ≥8kPa, and semi-annual screening for HCC in the case of cirrhosis. Indeed, it has been shown in a French cohort of patients with viral C cirrhosis that adherence to semi-annual screening is associated with better survival.
Eligible patients are primarily seen in primary care, and INCA has published a recommendation intended for general practitioners to improve the screening of fibrosis [13]. However, FIB-4 is poorly known among general practitioners [14], and access to Fibroscan® remains limited [15], hindering the implementation of the recommendations. Therefore, a care pathway has been established in the Grenoble area, initiated by Professor Costentin, in collaboration with Dr. Hyerle (CPTS Sud Est Grenoblois), allowing access to Fibroscan® for patients in primary care, starting from 2022 at the CHU, and then in 2024 at the CPTS. Dr. Hyerle has been trained in the use of Fibroscan® and training sessions have been organized to promote this pathway to practitioners in Grenoble. The objective is to evaluate the completion of the pathway, particularly the management of MCF risk factors and referral to specialized consultation for patients with Fibroscan® ≥8 kPa.
开始日期2025-11-02 |
NCT07034404
Effects of a Digital Adapted Physical Activity Program on Physical Activity Levels and Sleep Quality in Patients With Spondyloarthritis: A Randomized, Controlled, Multicenter Study.
The goal of this clinical trial is to assess whether a tailored digital Adapted Physical Activity (APA) program can improve physical activity levels and sleep quality in adults diagnosed with spondyloarthritis (SpA).
The main questions it aims to answer are:
Does participation in a 6-month digital APA program increase average daily step count (measured with an activity tracker)? Does the program improve sleep quality (measured with the Pittsburgh Sleep Quality Index)? Researchers will compare participants receiving general physical activity advice (control group) to those following a structured digital APA program (intervention group) to see if the tailored digital support leads to better outcomes.
Participants will:
Complete baseline assessments including physical activity, sleep, pain, and quality of life measures.
Be randomly assigned to a control group or intervention group. For the intervention group, follow an individualized exercise program delivered through a virtual platform with support from an APA professional over 10 virtual sessions.
Wear a connected activity tracker (Withings) to monitor physical activity throughout the study.
Complete follow-up assessments at 6 and 12 months.
The main questions it aims to answer are:
Does participation in a 6-month digital APA program increase average daily step count (measured with an activity tracker)? Does the program improve sleep quality (measured with the Pittsburgh Sleep Quality Index)? Researchers will compare participants receiving general physical activity advice (control group) to those following a structured digital APA program (intervention group) to see if the tailored digital support leads to better outcomes.
Participants will:
Complete baseline assessments including physical activity, sleep, pain, and quality of life measures.
Be randomly assigned to a control group or intervention group. For the intervention group, follow an individualized exercise program delivered through a virtual platform with support from an APA professional over 10 virtual sessions.
Wear a connected activity tracker (Withings) to monitor physical activity throughout the study.
Complete follow-up assessments at 6 and 12 months.
开始日期2025-07-01 |
100 项与 Centre Hospitalier Universitaire de Grenoble 相关的临床结果
登录后查看更多信息
0 项与 Centre Hospitalier Universitaire de Grenoble 相关的专利(医药)
登录后查看更多信息
2,007
项与 Centre Hospitalier Universitaire de Grenoble 相关的文献(医药)2025-08-01·Anaesthesia Critical Care & Pain Medicine
Acute traumatic coagulopathy: What you should know, what is debated and what should come next
Review
作者: Bouzat, Pierre ; James, Arthur ; Cole, Elaine ; Gauss, Tobias ; Dünser, Martin
Managing acute traumatic coagulopathy involves several interventions, including tranexamic acid, plasma transfusion, factor administration, or coagulation therapy guided by viscoelastic methods. However, the range of evidence to support these strategies is variable or needs more consensus, and translation to clinical practice is challenging. To address these challenges, we propose a narrative review of randomized controlled trials published during the last two decades. This review will clarify how interventions have been evaluated, the specific populations involved, and the potential benefits and risks identified. By synthesizing the evidence from these randomized controlled trials, this review aims to provide clinicians with a clearer understanding of which strategies should change their clinical practices. Finally, this review also seeks to highlight gaps in the current literature, guiding future research and helping to establish more definitive clinical guidelines.
2025-07-01·JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Defibrillation Testing During Implantation of Subcutaneous Implantable Cardioverter Defibrillators
Article
作者: Champ Rigot, Laure ; Fauchier, Laurent ; Ait Said, Mina ; Peyrol, Michaël ; Kerkouri, Fawzi ; Maury, Philippe ; Garcia, Rodrigue ; Guenancia, Charles ; Hermida, Alexis ; Chauvin, Michel ; Boveda, Serge ; Leclercq, Christophe ; Pasquié, Jean Luc ; Khattar, Pierre ; Anselme, Frédéric ; Badoz, Marc ; Marijon, Eloi ; Lellouche, Nicolas ; Guy-Moyat, Benoît ; El Bouazzaoui, Rim ; Amara, Walid ; Sellal, Jean Marc ; Laredo, Mikael ; Sadoul, Nicolas ; Bordachar, Pierre ; Gourraud, Jean-Baptiste ; Behar, Nathalie ; Hourdain, Jérôme ; Defaye, Pascal ; Chevalier, Philippe ; Ploux, Sylvain ; Da Costa, Antoine ; Deharo, Jean Claude ; Pierre, Bertrand ; Fareh, Samir ; Potelle, Charlotte ; Jesel, Laurence ; Marquié, Christelle ; Varlet, Emilie ; de Guillebon, Maxime ; Jacon, Peggy ; Eschalier, Romain ; Mansourati, Vincent ; Mondoly, Pierre ; Gitenay, Edouard ; Gandjbakhch, Estelle ; Probst, Vincent
BACKGROUND:
Defibrillation testing (DT) remains recommended during subcutaneous implantable cardioverter defibrillator (S-ICD) implantation due to limited supporting evidence.
OBJECTIVES:
The objective of this study was to evaluate the long-term impact of DT during S-ICD implantation.
METHODS:
The HONEST (coHOrte fraNcaise des dEfibrillateurs Sous cuTanés) study is a nationwide, ongoing observational study, including all S-ICD recipients in France (2012-2019). Five-year endpoints were centrally adjudicated, and propensity score-weighted analyses compared outcomes by DT status.
RESULTS:
Among 4,924 patients, DT was performed in 4,066 (82.6%), decreasing from 85.4% (2012-2014) to 66.9% in 2019 (P < 0.001). Nontested patients were older (51.2 vs 49.6 years; P = 0.007), had lower left ventricular ejection fraction (37.6% vs 43.3%; P < 0.001), and were more frequently implanted for primary prevention (68.0% vs 62.4%; P = 0.002) and structural heart disease (84.9% vs 76.8%; P < 0.001). DT-related complications occurred in 0.1%, including 2 deaths. Failure rate was 1.0%, with 87.8% undergoing corrective reinterventions. Independent predictors of DT failure were elevated shock impedance (≥89 Ω; OR: 4.60; 95% CI: 2.32-9.66; P < 0.001) and obesity (body mass index ≥30 kg/m2; OR: 2.17; 95% CI: 1.01-4.55; P = 0.007). After adjustment, DT omission was not associated with increased risks of overall mortality (HR: 1.17; 95% CI: 0.86-1.61; P = 0.313), cardiovascular mortality (HR: 1.04; 95% CI: 0.70-1.56; P = 0.846), sudden cardiac death (HR: 0.27; 95% CI: 0.04-1.72; P = 0.167), and appropriate (HR: 1.01; 95% CI: 0.78-1.30; P = 0.945) or inappropriate shocks (HR: 0.98; 95% CI: 0.78-1.23; P = 0.865). Combined rates of ineffective shocks or undetected ventricular arrhythmias were similar (0.05 vs 0.06 per 100 person-years).
CONCLUSIONS:
Our findings suggest that DT can be safely omitted in the majority of S-ICD recipients, whereas selective DT may be considered in higher-risk subgroups. (S-ICD French Cohort Study (HONEST); NCT05302115).
2025-06-01·JOURNAL OF PEDIATRIC SURGERY
Ovarian Torsion in Prepubertal Girls: Clinical Characteristics, Biological and Radiological Features, Reccurency Rate
Article
作者: Le Pabic, Estelle ; Bousquet, Marie ; Clermidi, Pauline ; Bourezma, Mélina ; Vérot, Pierre-Louis ; Hild, Olivier ; Bey, Marie ; François-Coridon, Hélène ; Bonnin, Yannis ; Glenisson, Mathilde ; Messelod, Charlène ; Arnaud, Alexis P ; Defert, Coralie ; Haraux, Elodie ; Lubet, Alexis ; Zislin, Manon ; Cartault, Audrey ; Deleforterie, Thomas ; Bourg, Agate ; Breaud, Jean ; Haffreingue, Aurore ; Scalabre, Aurélien ; Schmitt, Françoise ; Jochault-Ritz, Sandy ; Cousin, Ianis ; Olland, Adèle ; Belgacem, Alexis ; Péré, Morgane ; Lefébure, Chloé
INTRODUCTION:
The diagnosis of ovarian torsion is made with delay among pre-pubertal girls and the management after the surgical detorsion is poorly codified. We interested in the French experience during the last two decades.
METHODS:
Retrospective study in French pediatric surgery centers from January 2000 to December 2022 concerning girls who presented with at least 1 episode of ovarian torsion in the prepubertal period. Data collected included patient history, symptomatology, biological and imaging assessment at first episode, emergency surgery, follow-up including recurrence.
RESULTS:
Thirty centers participated and we included 502 girls diagnosed with ovarian torsion during a surgical procedure performed due to abdominal pain (with or without ovarian mass). The girls had a mean age of 7.9 years (±2.8) and a median age of 8.3 years (Q1 5.97; Q3 10.12) at the time of the first episode of torsion. Nausea or vomiting was present in 71 % of cases. Fever was present in 23 % of cases and was more displayed 24 h after the onset of abdominal pain (p < 0.0001). Mean follow-up was 2.1 (±2.61) years. Only 42 out of 142 (30 %) girls with enlarged ovaries (>97th percentile) were referred to the endocrinologist to assess the existence of hormonal anomalies. Of the 482 girls without oophoropexy after the first episode of torsion, 71 (14.7 %) experienced at least one recurrence. Among them: 10 (7.5 %) had an ovarian mass and 42 (55 %) enlarged ovaries.
CONCLUSION:
Symptoms of ovarian torsion in pre-pubertal girls are not specific and clinicians should be aware of this insidious presentation in this group. These girls should be systematically referred to endocrinologists.
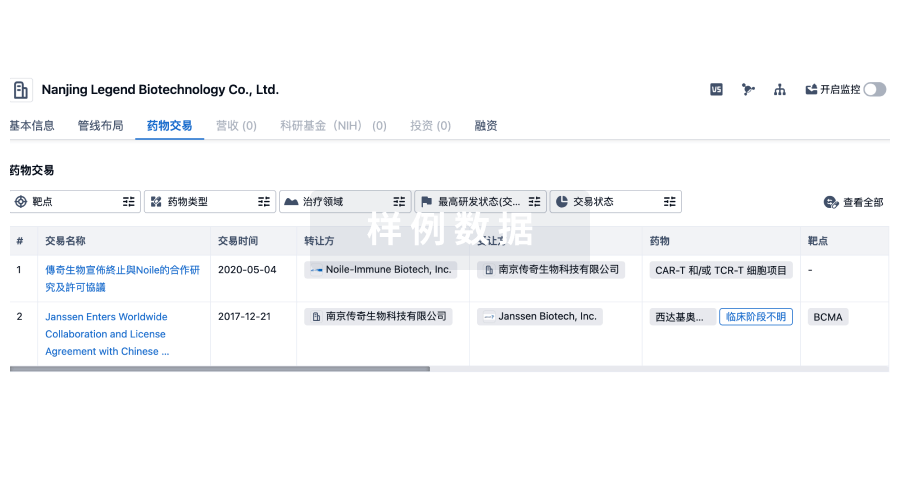
100 项与 Centre Hospitalier Universitaire de Grenoble 相关的药物交易
登录后查看更多信息
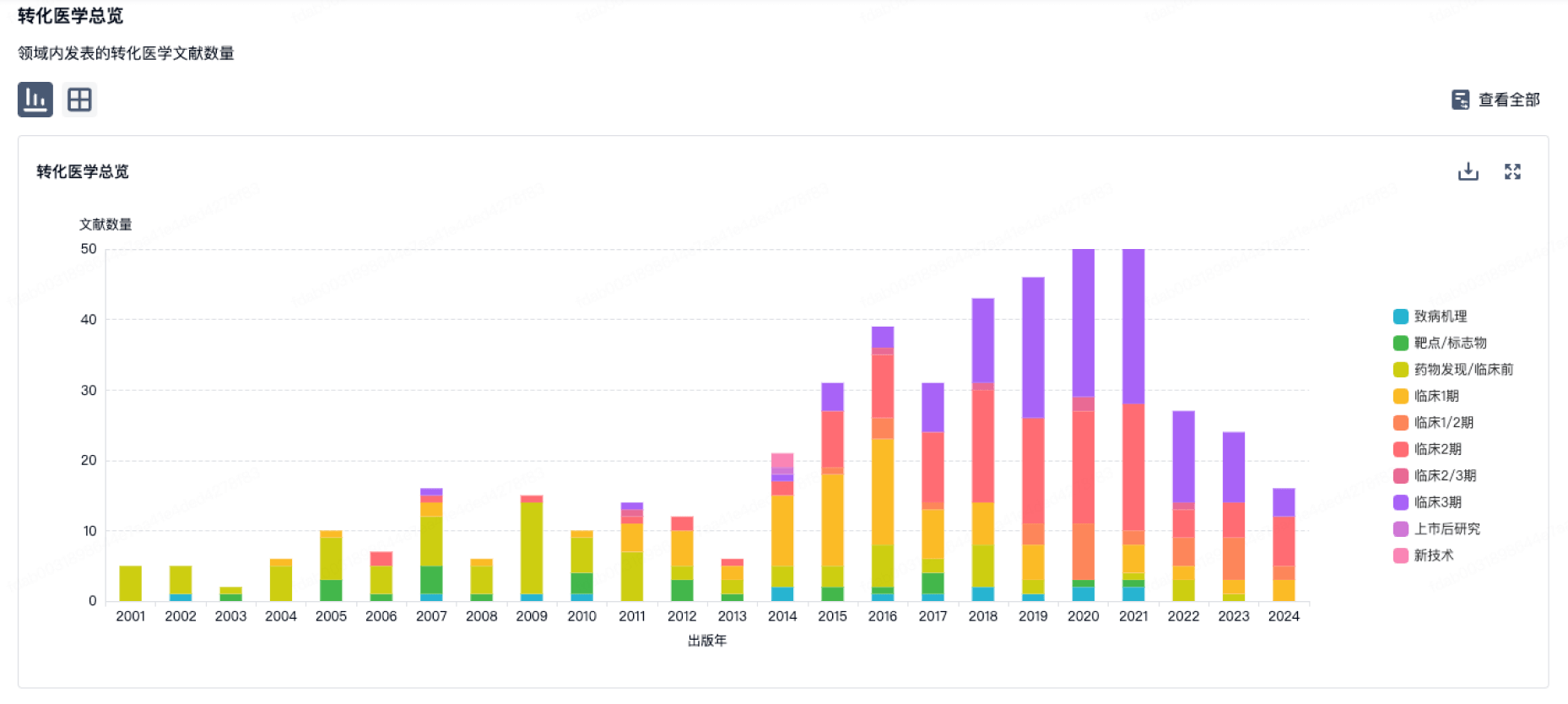
100 项与 Centre Hospitalier Universitaire de Grenoble 相关的转化医学
登录后查看更多信息
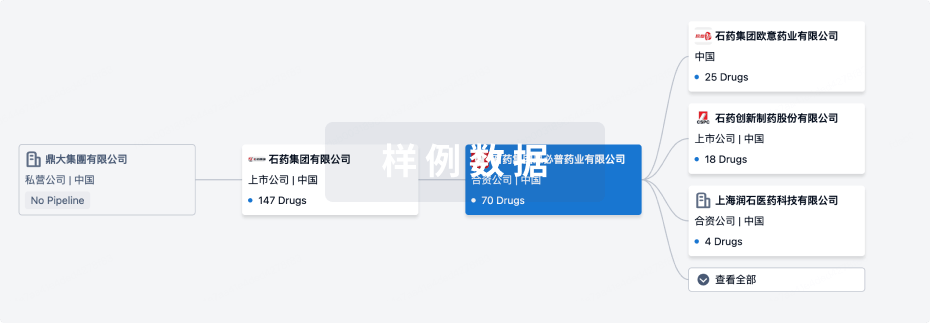
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年08月24日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
药物发现
1
3
其他
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
Anti-Pseudomonas antibodies(University Hospital, Grenoble) | 假单胞菌感染 更多 | 临床阶段不明 |
WO2022248475 ( BET )专利挖掘 | 炎症 更多 | 药物发现 |
99mTc-cAbVCAM1-5 ( VCAM1 ) | 动脉粥样硬化斑块 更多 | 无进展 |
GeniusVacMel4 | 转移性黑色素瘤 更多 | 无进展 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
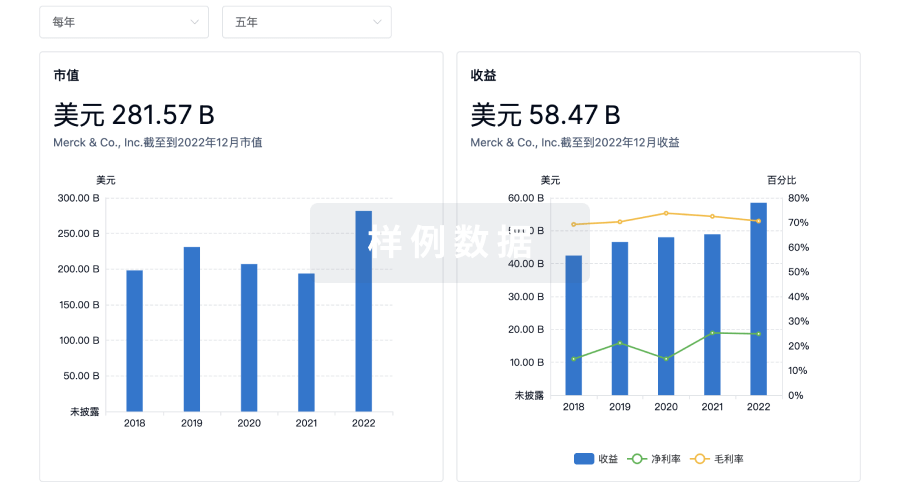
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用

