预约演示
更新于:2025-05-07
PolyNovo Biomaterials Pty Ltd.
子公司|2004|Australia
子公司|2004|Australia
更新于:2025-05-07
概览
关联
7
项与 PolyNovo Biomaterials Pty Ltd. 相关的临床试验NCT05477225
A Randomized, Controlled Trial Comparing the Use of a Biodegradable Temporizing Matrix to Cadaver Skin in the Reconstruction of Hidradenitis Suppurativa Excisions
This will be a prospective, interventional, single-center, randomized, controlled, comparative study comparing a total of 10 patients treated with BTM and SOC in wounds diagnosed with Hidradenitis suppurativa (5 in each group).
开始日期2022-10-01 |
NCT05506215
A Prospective, Multicenter, Open Label, Randomized, Controlled Clinical Study Evaluating the Effect of NovoSorb ® SynPath™ Dermal Matrix Compared to Standard of Care (SOC) In the Treatment of Nonresponsive, Chronic Diabetic Foot Ulcers.
The study will evaluate the efficacy of SynPath™, a synthetic dermal matrix, in the treatment of diabetic foot ulcers in subjects with diabetes mellitus versus Standard of Care treatment.
Half the subjects with be treated using SynPath™ while the other half will receive Standard of Care treatment
Half the subjects with be treated using SynPath™ while the other half will receive Standard of Care treatment
开始日期2022-07-10 |
NCT04090424
A Pivotal Study to Assess the Safety and Effectiveness of NovoSorb® Biodegradable Temporizing Matrix (BTM) in the Treatment of Severe Burn Skin Injuries
This is a multi-center, pivotal study to assess the safety and effectiveness of a new method of treating severe burns using NovoSorb® Biodegradable Temporizing Matrix (BTM).
开始日期2021-09-21 |
申办/合作机构 |
100 项与 PolyNovo Biomaterials Pty Ltd. 相关的临床结果
登录后查看更多信息
0 项与 PolyNovo Biomaterials Pty Ltd. 相关的专利(医药)
登录后查看更多信息
5
项与 PolyNovo Biomaterials Pty Ltd. 相关的文献(医药)2023-11-01·Burns
Clinical outcomes and resource utilisation in patients with major burns treated with NovoSorb® BTM
Article
作者: Maher, Declan ; Brown, Jason ; Betar, Noah ; Wheatley, Lucas ; Barker, Timothy
2023-09-01·JPRAS Open
Long-term scarring outcomes and safety of patients treated with NovoSorbⓇ Biodegradable Temporizing Matrix (BTM): An observational cohort study
Article
作者: Cleland, H ; Lo, C H ; Concannon, E ; Barker, T M ; Holden, D ; Heath, K ; Salerno, S ; Coghlan, P ; Wagstaff, M J D ; Damkat-Thomas, L
2022-09-02·Journal of Wound Care
Use of a bilayer biodegradable synthetic dermal matrix for the management of defects arising from necrotising fasciitis
Article
作者: Barker, Timothy ; Ricketts, Sophie ; Wagstaff, Marcus ; Bruscino-Raiola, Frank
100 项与 PolyNovo Biomaterials Pty Ltd. 相关的药物交易
登录后查看更多信息
100 项与 PolyNovo Biomaterials Pty Ltd. 相关的转化医学
登录后查看更多信息
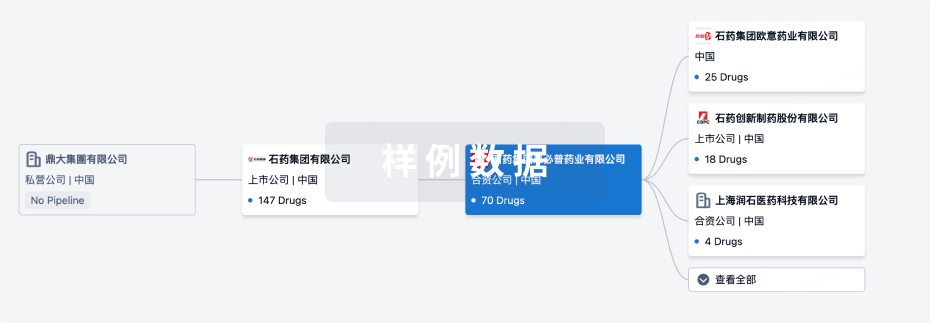
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年07月04日管线快照
无数据报导
登录后保持更新
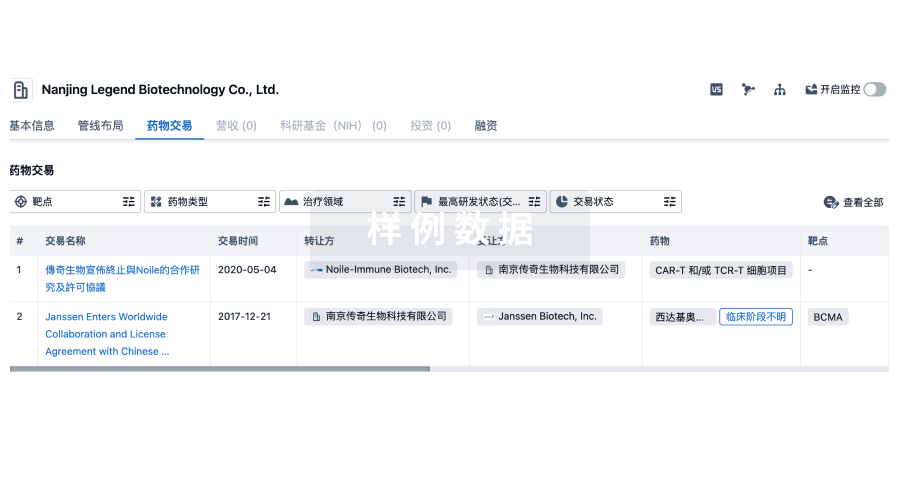
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
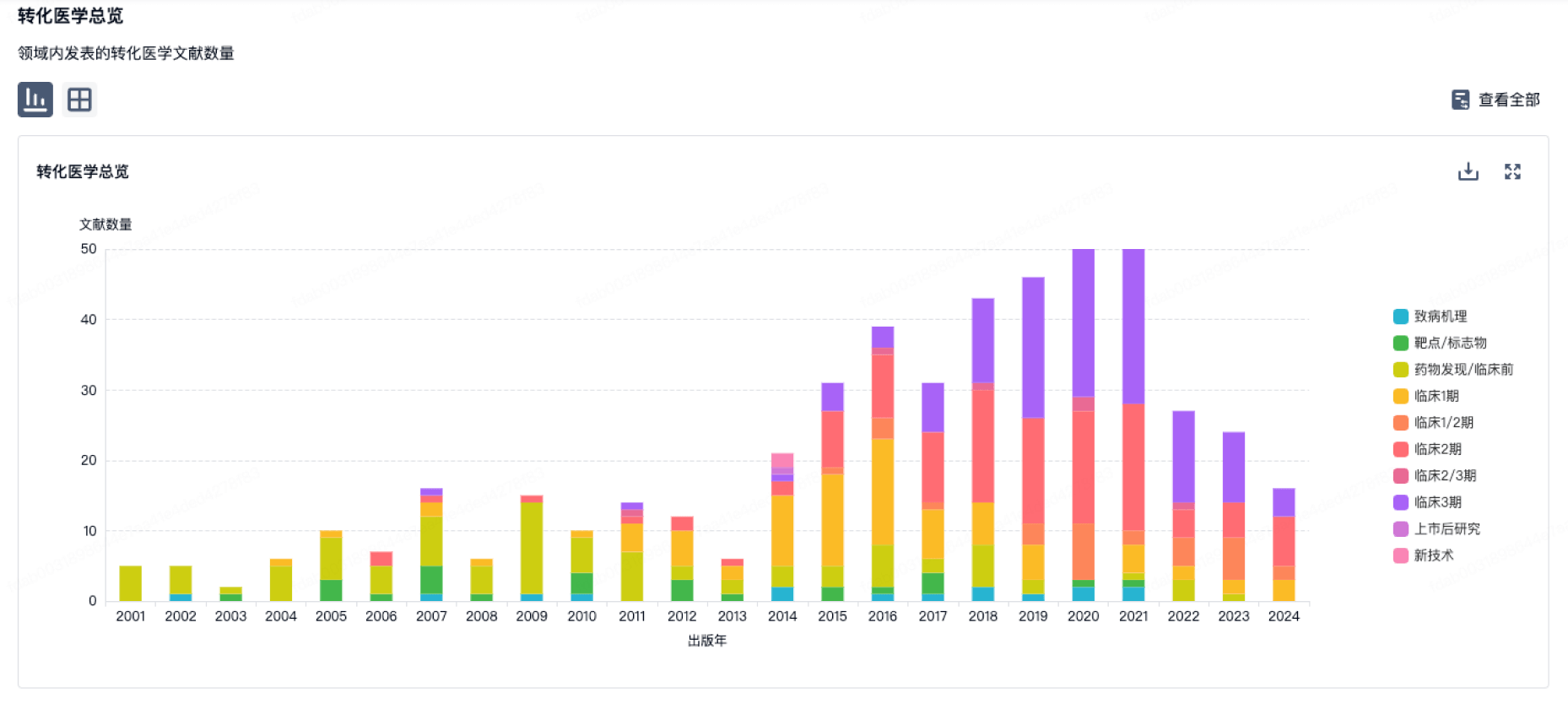
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
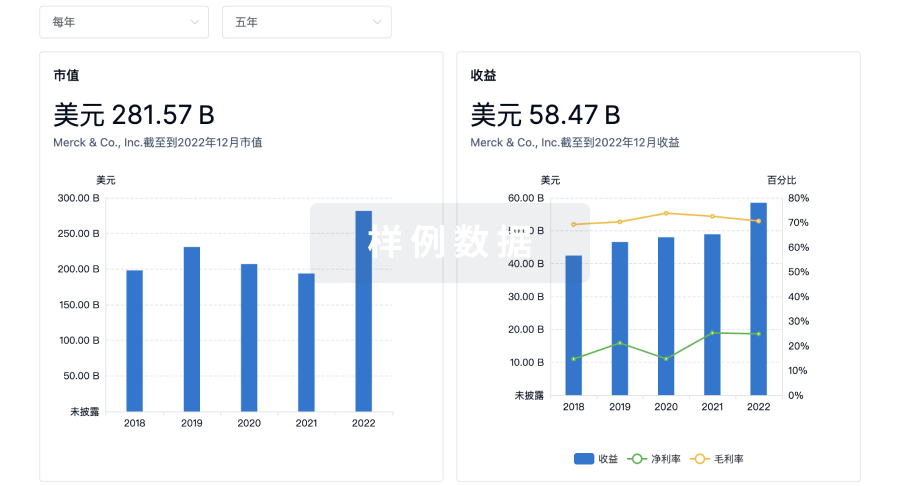
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用