预约演示
更新于:2025-05-07

NHS Lanarkshire
更新于:2025-05-07
概览
关联
25
项与 NHS Lanarkshire 相关的临床试验NCT06928285
Community Rollout of Technology Enriched Rehabilitation After Stroke: An Implementation Study
The minimum guideline recommendations for rehabilitation after stroke are not being met. This compromises individual recovery and increasing the global burden of disability. A multi-technology solution, co-created with people living with stroke, has been shown to be feasible in both sub-acute and chronic populations but has not been implemented as an integrated rehabilitation service.
The aim of this implementation study is to assess the ability of a technology enriched model of rehabilitation to deliver guideline recommendations in a range of NHS and local authority settings that provide rehabilitation services to stroke survivors at different stages of their recovery. The findings will be used to co-create a scalable, adaptable, and sustainable model that meets rehabilitation guidelines.
The aim of this implementation study is to assess the ability of a technology enriched model of rehabilitation to deliver guideline recommendations in a range of NHS and local authority settings that provide rehabilitation services to stroke survivors at different stages of their recovery. The findings will be used to co-create a scalable, adaptable, and sustainable model that meets rehabilitation guidelines.
开始日期2025-08-01 |
申办/合作机构 |
NCT06908148
SALACIA: Randomised Control Trial of SALvesAn Neutral Electrolysed Water Versus Conventional Management of Non-healing dIAbetic Foot Wounds
Increasing prevalence of diabetes mellitus has led to increasing numbers of chronic non-healing foot ulcers (wounds).
Electrolysed water is a novel antiseptic which reduces bacterial load and appears to encourage wound healing. The investigators propose to compare electrolysed water against conventional management.
Electrolysed water is a novel antiseptic which reduces bacterial load and appears to encourage wound healing. The investigators propose to compare electrolysed water against conventional management.
开始日期2025-07-01 |
申办/合作机构 |
NCT06114732
Motivating Physical Activity With Behavioural interVention and Electrical Stimulation Remotely in People With Intermittent Claudication (MAvERIC): a Feasibility Randomised Controlled Trial
Peripheral Arterial Disease (PAD) is a common vascular disease which commonly causes limb pain and reduced exercise tolerance termed Intermittent Claudication (IC). People with PAD and IC have impaired quality of life, reduced walking ability, and increased mortality compared to those who do not have the condition.
Improving physical activity (PA) is important in individuals with IC it can improve function, morbidity and mortality rates. While supervised exercise classes are recommended by healthcare authorities they are geographically sparse, and not always accessible due to individuals walking limitations. While home-based exercise can be accessible and improve walking ability, it can be challenging for people with IC to initially plan, conduct, and stay motivated to complete a walking program unsupported, especially when they experience limb pain when walking.
Investigators have shown that Transcutaneous Electrical Nerve Stimulation (TENS), a non-invasive pain management device, with aims to improve pain and walking distances in patients with IC may be an acceptable modality alongside advice and support from a physiotherapist to overcome these challenges. Investigators have also shown that motivational interviewing, education, and goal-setting with a physiotherapist (physical therapist) has the potential to increase PA, and quality of life.
This study aims to conduct a feasibility trial of four telehealth physiotherapy sessions, alongside the provision of a CE-marked TENS device to reduce limb pain during physical activity. This will be compared to the usual care offered in NHS Lanarkshire
Improving physical activity (PA) is important in individuals with IC it can improve function, morbidity and mortality rates. While supervised exercise classes are recommended by healthcare authorities they are geographically sparse, and not always accessible due to individuals walking limitations. While home-based exercise can be accessible and improve walking ability, it can be challenging for people with IC to initially plan, conduct, and stay motivated to complete a walking program unsupported, especially when they experience limb pain when walking.
Investigators have shown that Transcutaneous Electrical Nerve Stimulation (TENS), a non-invasive pain management device, with aims to improve pain and walking distances in patients with IC may be an acceptable modality alongside advice and support from a physiotherapist to overcome these challenges. Investigators have also shown that motivational interviewing, education, and goal-setting with a physiotherapist (physical therapist) has the potential to increase PA, and quality of life.
This study aims to conduct a feasibility trial of four telehealth physiotherapy sessions, alongside the provision of a CE-marked TENS device to reduce limb pain during physical activity. This will be compared to the usual care offered in NHS Lanarkshire
开始日期2024-01-29 |
申办/合作机构 |
100 项与 NHS Lanarkshire 相关的临床结果
登录后查看更多信息
0 项与 NHS Lanarkshire 相关的专利(医药)
登录后查看更多信息
261
项与 NHS Lanarkshire 相关的文献(医药)2025-04-21·Neuropsychological Rehabilitation
The reliability and validity of brief cognitive screening tools used in traumatic brain injury: A systematic review
Review
作者: Fradera, Alexander ; Cullen, Breda ; McLaren, Jessica
2024-09-09·British Journal of Surgery
SP3.1 - Could shorter length of stay and oncological non inferiority justify a radical paradigm shift towards RAS to be the gold standard for all rectal cancer resections
作者: Qazalbash, Zeeshan Ali ; Tan, Chin ; Mukherjee, Arijit ; Khan, Junaid ; Khopekar, Faid
2024-09-09·British Journal of Surgery
ThP1.3 - Oncoplastic Surgery and Magseed Markers: A five-year snapshot of ambition and evolution in breast conserving surgery
作者: Murphy, Dermot ; Lannigan, Alison ; McIlhenny, Jennifer ; Lang, Anne ; Bell, Emma ; Gray, Karen
100 项与 NHS Lanarkshire 相关的药物交易
登录后查看更多信息
100 项与 NHS Lanarkshire 相关的转化医学
登录后查看更多信息
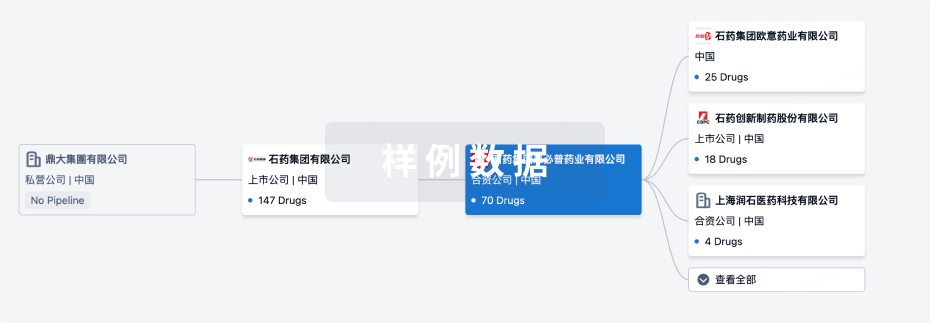
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年07月15日管线快照
无数据报导
登录后保持更新
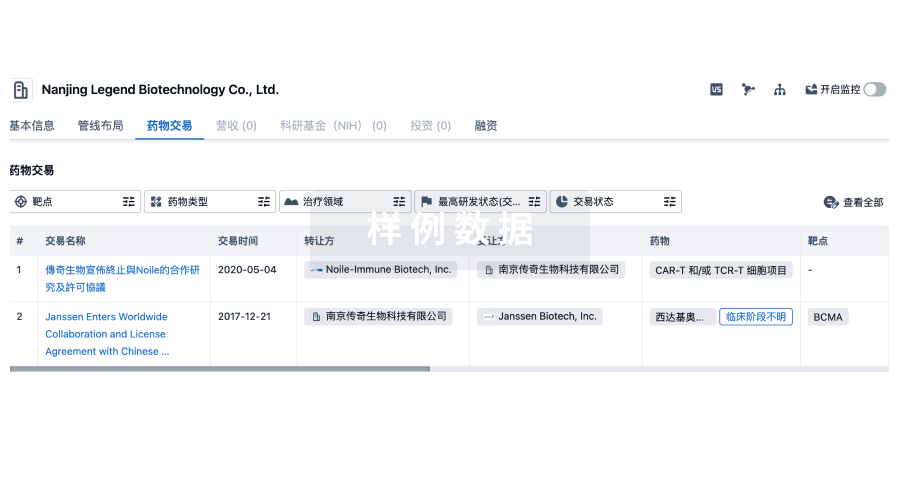
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
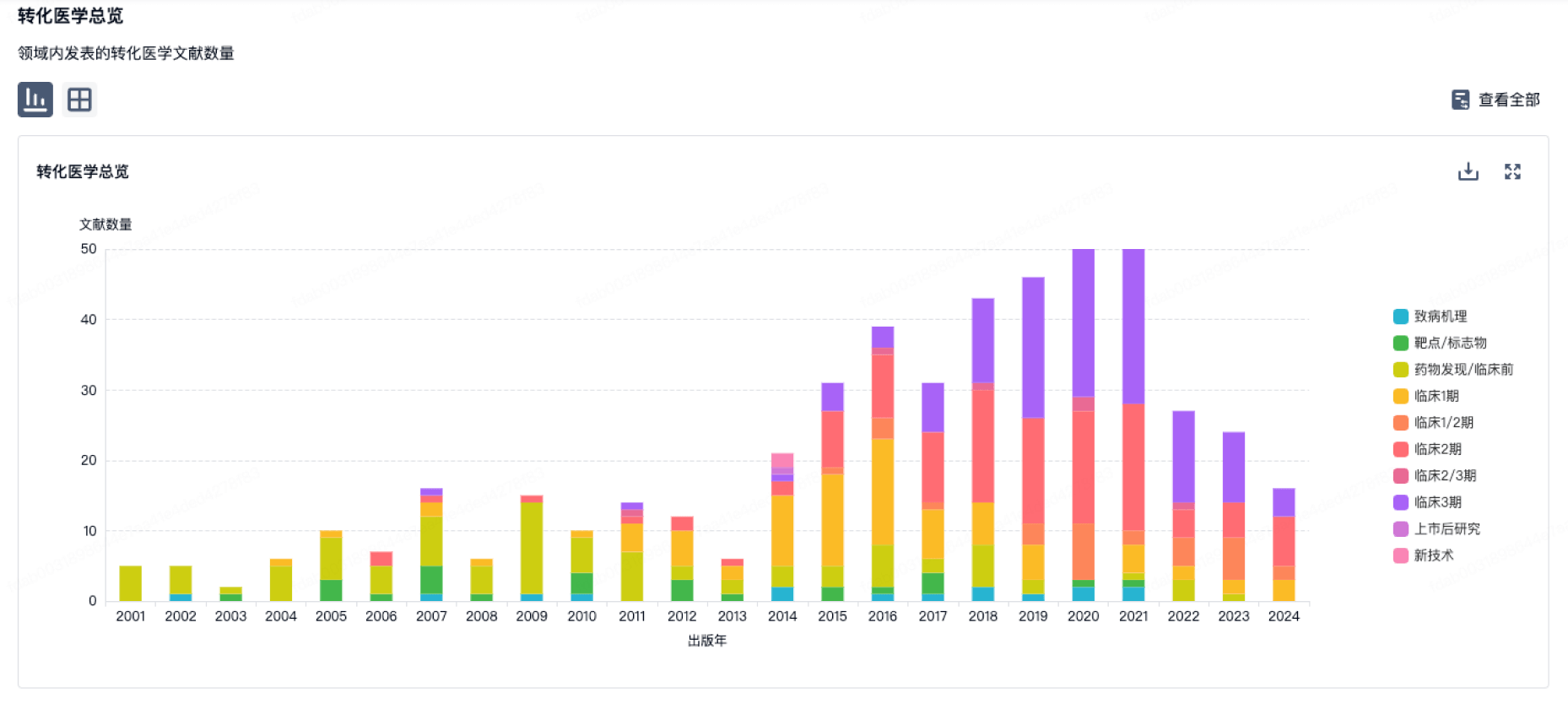
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
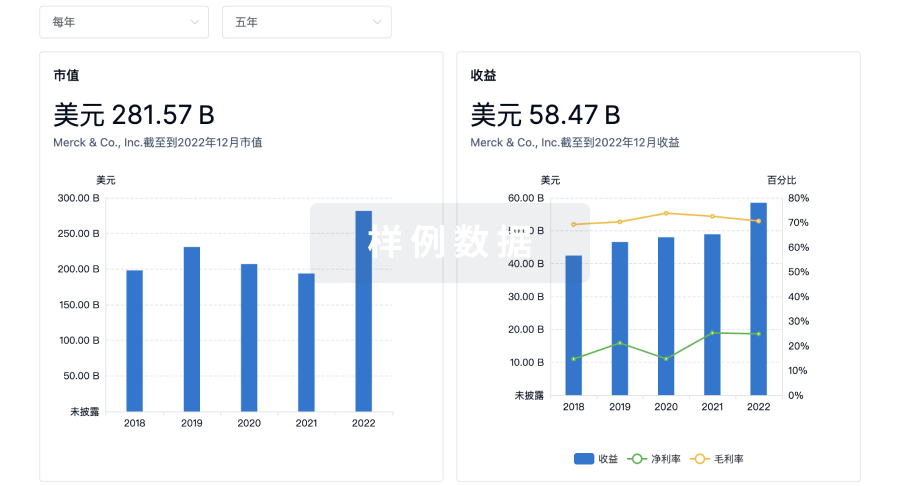
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

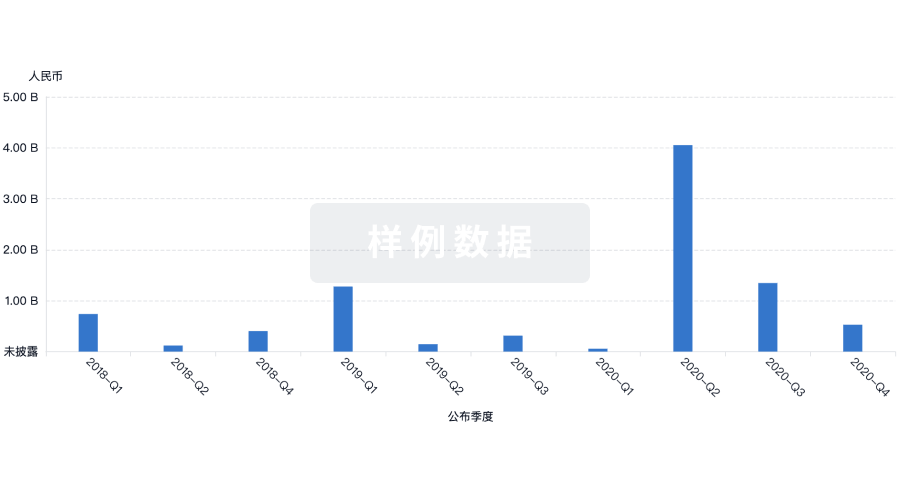
投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
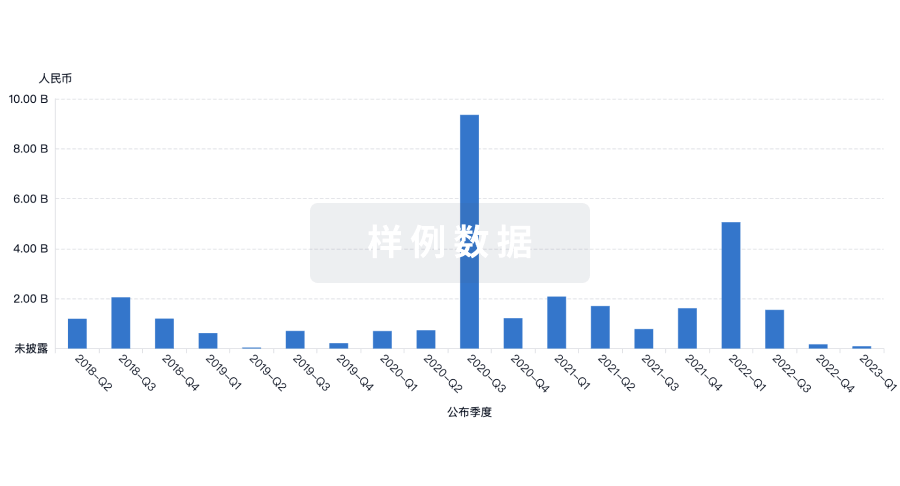
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用

