预约演示
更新于:2025-05-07
Immune Response Biopharma, Inc.
更新于:2025-05-07
概览
标签
免疫系统疾病
内分泌与代谢疾病
皮肤和肌肉骨骼疾病
治疗性疫苗
单克隆抗体
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 治疗性疫苗 | 1 |
| 单克隆抗体 | 1 |
| 排名前五的靶点 | 数量 |
|---|---|
| IL-1β(白细胞介素-1β) | 1 |
关联
10
项与 Immune Response Biopharma, Inc. 相关的药物靶点- |
作用机制 免疫刺激剂 |
在研适应症 |
非在研适应症- |
最高研发阶段临床3期 |
首次获批国家/地区- |
首次获批日期- |
靶点 |
作用机制 IL-1β调节剂 |
在研适应症 |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期- |
靶点- |
作用机制- |
在研机构- |
在研适应症- |
非在研适应症- |
最高研发阶段终止 |
首次获批国家/地区- |
首次获批日期- |
5
项与 Immune Response Biopharma, Inc. 相关的临床试验NCT02200718
A Phase I Study of NeuroVax™, a Novel Therapeutic TCR Peptide Vaccine for Pediatric Multiple Sclerosis
A Phase I Study of NeuroVax™, a Novel Therapeutic TCR Peptide Vaccine for Pediatric Multiple Sclerosis to demonstrate safety & efficacy
开始日期2020-12-31 |
NCT02057159
A Phase II Study of NeuroVax™, a Therapeutic TCR Peptide Vaccine for SPMS of Multiple Sclerosis
Multi-center, randomized , double-blind, placebo-controlled , two arm parallel design study of NeuroVax™ vs. Incomplete Freund's Adjuvant ( I F A) placebo. 200 subjects with Secondary Progressive SPMS
开始日期2020-03-09 |
NCT02149706
A Phase IIb Study of NeuroVax™, a Novel Therapeutic TCR Peptide Vaccine for SPMS of Multiple Sclerosis Slowing Disease Progression Via Vaccination
Multi-center, randomized , double-blind, placebo-controlled , two arm parallel design study of NeuroVax™ vs. Incomplete Freund's Adjuvant ( I F A) placebo. 150 subjects with Secondary Progressive SPMS.
开始日期2020-03-09 |
100 项与 Immune Response Biopharma, Inc. 相关的临床结果
登录后查看更多信息
0 项与 Immune Response Biopharma, Inc. 相关的专利(医药)
登录后查看更多信息
13
项与 Immune Response Biopharma, Inc. 相关的文献(医药)2008-06-28·Clinical and Experimental Immunology3区 · 医学
Autoproliferation in HIV-1-infected patients undergoing active HIV-1-specific immunotherapy
3区 · 医学
Article
作者: WORMSLEY, S ; JENSEN, F C ; TRAUGER, R J ; GIERMAKOWSKA, W ; CARLO, D J ; TURNER, J
2002-05-02·Clinical and Experimental Immunology3区 · 医学
Predictors of HIV-specific lymphocyte proliferative immune responses induced by therapeutic vaccination
3区 · 医学
Article
作者: DIVELEY, J P ; MOSS, R B ; GIERMAKOWSKA, W K ; MORRISON, S A ; STEIGBIGEL, R T ; NARDO, C J ; WALLACE, M R ; CARLO, D J
2001-10-01·HIV Clinical Trials
Long-Term Follow-Up of HIV-1–Infected Thai Patients Immunized with Remune Monotherapy
Article
作者: Sirawaraporn, W. ; Churdboonchart, V. ; Isarangkura Na Ayudthya, B. ; Rugpao, S. ; Kulpradist, S. ; Carlo, D. ; Moss, R.B. ; Sukeepaisarncharoen, W. ; Chandeying, V.
3
项与 Immune Response Biopharma, Inc. 相关的新闻(医药)2025-03-05
The increasing occurrence of chronic and infectious diseases is the main driver of the rising demand for interferon. Furthermore, advancements in interferon production and ongoing research and development of innovative interferon therapies are key factors fueling the expansion of the interferon market from 2025 to 2032.
LAS VEGAS, March 5, 2025 /PRNewswire/ -- DelveInsight's
Interferons Market Insights report provides the current and forecast market analysis, individual leading interferons companies' market shares, challenges, interferons market drivers, barriers, trends, and key market interferons companies in the market.
Key Takeaways from the Interferons Market Report
As per DelveInsight estimates, North America is anticipated to dominate the global interferons market during the forecast period.
In the application segment of the interferon market, the leukemia category captured a significant revenue share in 2024.
Notable interferons companies such as
Bayer AG, Amega Biotech, Biogen, Merck KGaA, Novartis AG, Pfizer Inc., F. Hoffmann-La Roche Ltd., Biosidus, AOP Orphan Pharmaceuticals GmbH, Reliance Life Sciences, and several others, are currently operating in the interferons market.
In
September 2022, Eiger BioPharmaceuticals, a commercial-stage biopharmaceutical company focused on the development of innovative therapies for hepatitis delta virus (HDV) and other serious diseases, provided an update on the status of its planned request for emergency use authorization (EUA) of peginterferon lambda for the treatment of patients with mild-to-moderate COVID-19 based on its most recent communications with the U.S. Food and Drug Administration (FDA).
To read more about the latest highlights related to the interferons market, get a snapshot of the key highlights entailed in the
Global Interferons Market Report
Interferons Overview
Interferons (IFNs) are a group of signaling proteins that play a critical role in the immune response, particularly in defending against viral infections and modulating the activity of immune cells. They are classified into three main types: Type I (such as IFN-α and IFN-β), Type II (IFN-γ), and Type III (IFN-λ). Type I interferons are primarily produced in response to viral infections and function by activating antiviral pathways in host cells, inhibiting viral replication, and enhancing the activity of natural killer (NK) cells. IFN-γ, the sole Type II interferon, is crucial for activating macrophages and promoting adaptive immune responses, particularly in bacterial and tumor immunity. Type III interferons share functional similarities with Type I IFNs but act more selectively on epithelial cells, making them important in mucosal immunity.
Beyond their antiviral properties, interferons have significant roles in cancer immunotherapy and autoimmune diseases. They enhance antigen presentation, stimulate cytotoxic T cells, and modulate the tumor microenvironment, contributing to immune surveillance against malignancies. Clinically, recombinant interferons have been used to treat conditions such as hepatitis B and C, multiple sclerosis, and certain cancers. However, prolonged interferon therapy can lead to adverse effects, including flu-like symptoms, fatigue, and autoimmune complications. Recent research is focused on optimizing interferon-based therapies and combining them with immune checkpoint inhibitors or other immunomodulators to improve efficacy while minimizing toxicity.
Interferons Market Insights
North America holds the largest interferons market share due to a strong presence of biopharmaceutical companies, robust R&D investments, and high healthcare expenditure. The U.S. market, in particular, benefits from a well-established regulatory framework and widespread adoption of advanced biotherapeutics. Meanwhile, Europe follows closely, with key contributions from Germany, France, and the UK, where government support for biotech innovation and access to novel biologics drive market expansion.
In the Asia-Pacific region, the interferon market is witnessing rapid growth, fueled by rising healthcare infrastructure, an increasing prevalence of infectious diseases, and government initiatives to boost biopharmaceutical production. China and India are emerging as major players, with domestic companies investing heavily in biosimilar development and expanding manufacturing capacities. Latin America and the Middle East & Africa are also showing potential, albeit at a slower pace, due to improving healthcare access and growing awareness of biologic treatments. However, market expansion in these regions is challenged by high drug costs and regulatory hurdles, which may impact the adoption of interferon therapies.
To know more about why North America is leading the market growth in the interferons market, get a snapshot of the
Interferons Market Outlook
Interferons Market Dynamics
The interferons market is driven by their critical role in
treating viral infections, autoimmune diseases, and various cancers. Interferons (IFNs) are a class of cytokines that modulate the immune response, making them valuable in antiviral therapies (such as hepatitis B and C), multiple sclerosis, and oncology applications. The
increasing prevalence of these diseases, along with rising research into novel interferon-based therapies, continues to fuel market growth. However, the market faces challenges due to the
emergence of alternative therapies, such as monoclonal antibodies and small-molecule inhibitors, which offer higher efficacy and fewer side effects.
One of the key factors influencing market dynamics is the
shift from traditional interferon therapies to newer, more targeted treatments. For instance, in the treatment of hepatitis C, direct-acting antiviral agents (DAAs) have largely replaced interferon-based regimens due to their superior cure rates and reduced adverse effects. Similarly, in multiple sclerosis, oral therapies and monoclonal antibodies such as ocrelizumab and natalizumab have overshadowed interferon-beta treatments. Despite this, interferons remain relevant in certain applications, such as
rare cancers and specific immune disorders where alternative treatments are not as effective.
Another factor shaping the interferons market is the regulatory landscape. Interferons are biologic drugs, meaning they are subject to
stringent approval processes and high production costs. The development of biosimilar interferons has the potential to make these therapies more accessible, especially in emerging markets. However,
biosimilars face challenges in gaining market traction due to concerns about immunogenicity and physician preference for established brands. Companies
investing in next-generation interferons with improved efficacy and safety profiles may have an opportunity to capture a share of this evolving market.
Looking ahead, the future of the interferons market will be shaped by ongoing innovation, competitive pressures, and the need for cost-effective biologics. While traditional interferon therapies may continue to decline in some areas, their role in niche indications and combination therapies could sustain market demand. Companies focusing on improving delivery methods, reducing side effects, and exploring novel interferon applications in immuno-oncology and rare diseases may unlock new growth opportunities in this evolving landscape.
Get a sneak peek at the interferons market dynamics @
Interferons Market Dynamics Analysis
Interferons Market Assessment
Interferons Market Segmentation
Interferons Market Segmentation By Type: Alpha, Beta, and Gamma
Interferons Market Segmentation By Application: Hepatitis B, Hepatitis C, Leukemia, Multiple Sclerosis, and Others
Interferons Market Segmentation By Distribution Channel: Hospital Pharmacies, Retail Pharmacies, and Others
Interferons Market Segmentation By Geography: North America, Europe, Asia-Pacific, and Rest of World
Porter's Five Forces Analysis, Product Profiles,
Case Studies, KOL's Views, Analyst's View
Which MedTech key players in the interferons market are set to emerge as the trendsetter explore @
Interferons Companies
Table of Contents
Interested in knowing the interferons market by 2032? Click to get a snapshot of the
Interferons Market Trends
Related Reports
Multiple Sclerosis Market
Multiple Sclerosis Market Insights, Epidemiology, and Market Forecast – 2034 report delivers an in-depth understanding of the disease, historical and forecasted epidemiology, as well as the market trends, market drivers, market barriers, and key multiple sclerosis companies, including
Immune Response BioPharma, Inc., Clene Nanomedicine, Sanofi, Merck Healthcare KGaA, TG Therapeutics, Inc., Apimeds Inc., Bayer HealthCare, Novartis, Biogen, Alkermes, Genentech, among others.
Multiple Sclerosis Pipeline
Multiple Sclerosis Pipeline Insight – 2025 report provides comprehensive insights about the pipeline landscape, pipeline drug profiles, including clinical and non-clinical stage products, and the key multiple sclerosis companies, including
Novartis, Sanofi, Immunic, Biocad, Apimeds, Genentech (Roche), Merck, AB Science, Apurano Pharmaceuticals, Biogen, Tiziana Life Sciences, Worg Pharmaceuticals, Antisense Therapeutics, RemeGen, Atara Biotherapeutics, Contineum Therapeutics, Stem Cell Medicine Ltd., Ever Supreme Bio Technology Co., Ltd., ImCyse, among others.
Chronic Hepatitis B Market
Chronic Hepatitis B Market Insights, Epidemiology, and Market Forecast – 2034 report delivers an in-depth understanding of the disease, historical and forecasted epidemiology, as well as the market trends, market drivers, market barriers, and key chronic hepatitis B companies, including
GlaxoSmithKline, Ionis Pharma, Beijing Continent Pharmaceutical, Ascletis Pharmaceuticals, Vir Biotechnology, Brii Biosciences, Janssen, Arrowhead Pharmaceuticals, among others.
Chronic Hepatitis B Pipeline
Chronic Hepatitis B Pipeline Insight – 2025 report provides comprehensive insights about the pipeline landscape, pipeline drug profiles, including clinical and non-clinical stage products, and the key chronic hepatitis B companies, including
Vedanta Biosciences, Gilead Sciences, Dong-A ST Co, Assembly Biosciences, Arbutus Biopharma, Vir Biotechnology, Antios Therapeutics, Ascletis Pharmaceuticals, Shanghai HEP Pharmaceutical, Romark Laboratories, Qilu Pharmaceutical, Golden Biotechnology, Sunshine Lake Pharma, Ascentage Pharma, GlaxoSmithKline, Janssen Sciences, Henlix, Enyo Pharma, Tasly Tianjin Biopharmaceutical, Brii Biosciences, Vaxine Pty Ltd, Vaccitech limited, Zhejiang Palo Alto Pharmaceuticals, Suzhou Ribo Life Science, PharmaEssentia, Nucorion Pharmaceuticals, Jiangsu HengRui Medicine, Enanta Pharmaceuticals, Chong Kun Dang Pharmaceutical, Guangzhou Lupeng Pharmaceutical, VenatoRx Pharmaceuticals, Zhimeng Biopharm, among others.
About DelveInsight
DelveInsight is a leading Business Consultant, and Market Research firm focused exclusively on life sciences. It supports pharma companies by providing comprehensive end-to-end solutions to improve their performance.
Contact Us
Shruti Thakur
[email protected]
+14699457679
Logo:
SOURCE DelveInsight Business Research, LLP
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
免疫疗法
2024-11-13
Multiple sclerosis (MS) is a chronic neurological disorder affecting the central nervous system (CNS), particularly the brain, spinal cord, and optic nerves. Continuous research has led to new drug developments, particularly disease-modifying therapies (DMTs) that slow MS progression. Monoclonal antibodies, oral therapies, and infusion treatments are among the most promising options and drives the multiple sclerosis market.
LAS VEGAS, Nov. 13, 2024 /PRNewswire/ -- DelveInsight's
'
Multiple Sclerosis Pipeline Insight 2024
' report provides comprehensive global coverage of pipeline multiple sclerosis therapies in various stages of clinical development, major pharmaceutical companies are working to advance the pipeline space and future growth potential of the multiple sclerosis pipeline domain.
Key Takeaways from the Multiple Sclerosis Pipeline Report
DelveInsight's multiple sclerosis pipeline report depicts a robust space with
75+ active players working to develop
80+ pipeline therapies for multiple sclerosis treatment.
Key multiple sclerosis companies such as
Mapi Pharma, Novartis, Immunic, Biocad, Apimeds, Genentech (Roche), AB Science, Celltrion, Clene Nanomedicine, InnoCare Pharma, Oryzon Genomics, GeNeuro SA, AbbVie, BrainStorm Cell Therapeutics, NeuroSense Therapeutics, Denali Therapeutics Inc., Sanofi, MediciNova, Biogen, Tiziana Life Sciences, Antisense Therapeutics, RemeGen, Atara Biotherapeutics, Contineum Therapeutics, Eli Lilly and Company, Axsome Therapeutics, Accure therapeutics, Stem Cell Medicine Ltd., Ever Supreme Bio-Technology Co., Ltd., ImCyse, Lucid Psycheceuticals, Immune Response BioPharma, Guangzhou Lupeng Pharmaceutical, Kyowa Kirin, Nura Bio, Bristol-Myers Squibb, ImStem Biotechnology, Hoffmann-La Roche, LAPIX Therapeutics, Motric Bio, Immunophage Biotech, NervGen, FibroBiologics, Kyverna Therapeutics, GlaxoSmithKline, PolTREG, Cyxone, Biohaven Pharmaceuticals, HuniLife Biotechnology, GlobeStar Therapeutics, Anokion, Medsenic, ZyVersa Therapeutics, Alumis Inc., Axoltis Pharma, Barricade Therapeutics, BioNxt Solutions, Eikonoklastes Therapeutics, 4D Pharma, Gossamer Bio, Pasithea Therapeutics, Synaptogenix, Monte Rosa Therapeutics, Immix Biopharma, f5 Therapeutics, Autobahn Therapeutics, Biosenic, Polpharma Biologics, Find Therapeutics, TeraImmun, AptaTargets, Trethera, Aditxt, SetPoint Medical, Sarepta Therapeutics, Nucleome Therapeutics, Vaccinex Inc., and others are evaluating new multiple sclerosis drugs to improve the treatment landscape.
Promising multiple sclerosis pipeline therapies such as
GA Depot, Remibrutinib, Tolebrutinib, IMU 838, BCD-132, Apitox, Fenebrutinib, SAR 441344, CT-P53, CNM-Au8, Orelabrutinib, Vafidemstat, Temelimab, Elezanumab, NurOwn (MSC-NTF cells), PrimeC, SAR4433820, Ibudilast, BIIB091, Foralumab, ATL1102, RC18, ATA188, PIPE-307, Pirtobrutinib, LY3541860, Solriamfetol, Act-01, SCM-010, UMSC01, IMCY-0141, Lucid-MS, NeuroVax, LP-168, NB-4746, CC-97540, IMS-001, RO7121932, BMS-986196, LPX-TI641, MTR-601, IPG-11406, IPG-1094, NVG-291, CYMS-101, KYV-101, PIPE-791, GSK 3888130B, PTG-007, T 20K, BHV-8000, HuL001, Amethyst™, ANK 700, Arscimed, A-005, NX210c, Research programme: CAR-TREG, TASIN-1, Cladribine ODF, ET-101, MRx0002, GB7208, PAS-002, Bryostatin-1, MRT-6160, NXC-201, Research Program: Cytokine reduction, ABX-002, Arsenic trioxide, LL-341070, PB018, FTX 101, TI-235, TRE 515, NT-0007, NT-0002, NVG300, and others are under different phases of multiple sclerosis clinical trials.
In
October 2024, Immunic, Inc. reported favorable results from the non-binding interim futility analysis of its Phase 3 ENSURE trial, which is evaluating its lead candidate, vidofludimus calcium (IMU-838), a nuclear receptor-related 1 (Nurr1) activator, for the treatment of relapsing multiple sclerosis (RMS).
In October 2024, Immunic, Inc. announced a positive outcome of the non-binding, interim futility analysis of its Phase III ENSURE program, investigating lead asset, nuclear receptor related 1 (Nurr1) activator, vidofludimus calcium (IMU-838), for the treatment of relapsing multiple sclerosis (RMS). Based on the outcome of the interim futility analysis, an unblinded Independent Data Monitoring Committee (IDMC) has recommended that the trials are not futile and should continue as planned.
In
September 2024, Roche, secured FDA approval for an injectable form of its blockbuster multiple sclerosis treatment, Ocrevus, reducing patient treatment time and potentially helping the company stay ahead of increasing competition.
In
September 2024, Sanofi announced the outcomes of Phase III clinical trials of its investigational oral brain-penetrant BTK inhibitor, tolebrutinib, aimed at treating multiple sclerosis (MS). These studies, namely HERCULES, GEMINI 1, and GEMINI 2, have provided mixed results, with the HERCULES trial meeting its primary endpoint while the GEMINI trials did not. The HERCULES study focused on the efficacy and safety of tolebrutinib in individuals with non-relapsing secondary progressive MS (nrSPMS) compared to a placebo.
In
August 2024, Abata Therapeutics announced that the U.S. Food and Drug Administration (FDA) has granted Fast Track designation for ABA-101 for the treatment of patients with progressive multiple sclerosis (MS). The FDA recently cleared ABA-101's Investigational New Drug (IND) application, and initiation of a first-in-human (FIH) Phase I study is imminent.
In
August 2024, TG Therapeutics announced that the FDA has cleared an investigational new drug (IND) application submitted by TG Therapeutics for azercabtagene zapreleucel (azer-cel), an investigational allogeneic chimeric antigen receptor T-cell (CAR-T) therapy, for a phase 1 clinical trial in patients with progressive multiple sclerosis (MS).
In
January 2024, Kyverna Therapeutics, Inc. announced it received fast-track designation by the U.S. Food and Drug Administration (FDA) for its autologous, fully human CD19 chimeric antigen receptor (CAR) T-cell product candidate, KYV-101, to be used for the treatment of multiple sclerosis (MS).
Request a sample and discover the recent advances in multiple sclerosis treatment drugs @
Multiple Sclerosis Pipeline Report
The multiple sclerosis pipeline report provides detailed profiles of pipeline assets, a comparative analysis of clinical and non-clinical stage multiple sclerosis drugs, inactive and dormant assets, a comprehensive assessment of driving and restraining factors, and an assessment of opportunities and risks in the multiple sclerosis clinical trial landscape.
Multiple Sclerosis Overview
Multiple sclerosis is a chronic autoimmune disorder that affects the central nervous system, leading to the deterioration or permanent damage of myelin, the protective sheath surrounding nerve fibers. While the exact cause of multiple sclerosis remains unclear, it is believed to involve a combination of genetic predisposition, environmental factors, and possibly viral infections. Common symptoms of multiple sclerosis include fatigue, difficulty walking, numbness or tingling in the limbs, muscle weakness, and vision problems, which can vary significantly among individuals and may evolve over time.
Diagnosis typically involves a combination of neurological examinations, magnetic resonance imaging (MRI) to detect lesions in the brain and spinal cord, and sometimes lumbar puncture to analyze cerebrospinal fluid for inflammatory markers. While there is no cure for multiple sclerosis, treatment options aim to manage symptoms, reduce the frequency and severity of relapses, and slow disease progression. This may include disease-modifying therapies (DMTs), corticosteroids for acute exacerbations, and symptomatic treatments such as physical therapy, pain management, and lifestyle modifications. Early diagnosis and a tailored treatment plan are crucial for improving the quality of life for those living with multiple sclerosis.
Find out more about multiple sclerosis treatment drugs @
Drugs for
Multiple Sclerosis Treatment
A snapshot of the Multiple Sclerosis Pipeline Drugs mentioned in the report:
Learn more about the emerging multiple sclerosis pipeline therapies @
Multiple Sclerosis Clinical Trials
Multiple Sclerosis Therapeutics Assessment
The multiple sclerosis pipeline report proffers an integral view of the multiple sclerosis emerging novel therapies segmented by stage, product type, molecule type, mechanism of action, and route of administration.
Scope of the Multiple Sclerosis Pipeline Report
Coverage: Global
Therapeutic Assessment By Product Type: Mono, Combination, Mono/Combination
Therapeutic Assessment By Clinical Stages: Discovery, Pre-clinical, Phase I, Phase II, Phase III
Therapeutics Assessment
By Route of Administration: Oral, Intravenous, Subcutaneous, Parenteral, Topical
Therapeutics Assessment
By Molecule Type: Recombinant fusion proteins, Small molecule, Monoclonal antibody, Peptide, Polymer, Gene therapy
Therapeutics Assessment
By Mechanism of Action: Immunomodulators, MHC class II gene modulators, Agammaglobulinaemia tyrosine kinase inhibitors, Dihydroorotate dehydrogenase inhibitors, Nuclear receptor subfamily 4 group A member 2 agonists, CD20 antigen inhibitors, Energy metabolism stimulants; Immunomodulators, Lysine-specific demethylase 1 inhibitors, Monoamine oxidase B inhibitors, Protein-arginine deiminase inhibitors, Immunostimulants
Key Multiple Sclerosis Companies: Mapi Pharma, Novartis, Immunic, Biocad, Apimeds, Genentech (Roche), AB Science, Celltrion, Clene Nanomedicine, InnoCare Pharma, Oryzon Genomics, GeNeuro SA, AbbVie, BrainStorm Cell Therapeutics, NeuroSense Therapeutics, Denali Therapeutics Inc., Sanofi, MediciNova, Biogen, Tiziana Life Sciences, Antisense Therapeutics, RemeGen, Atara Biotherapeutics, Contineum Therapeutics, Eli Lilly and Company, Axsome Therapeutics, Accure therapeutics, Stem Cell Medicine Ltd., Ever Supreme Bio-Technology Co., Ltd., ImCyse, Lucid Psycheceuticals, Immune Response BioPharma, Guangzhou Lupeng Pharmaceutical, Kyowa Kirin, Nura Bio, Bristol-Myers Squibb, ImStem Biotechnology, Hoffmann-La Roche, LAPIX Therapeutics, Motric Bio, Immunophage Biotech, NervGen, FibroBiologics, Kyverna Therapeutics, GlaxoSmithKline, PolTREG, Cyxone, Biohaven Pharmaceuticals, HuniLife Biotechnology, GlobeStar Therapeutics, Anokion, Medsenic, ZyVersa Therapeutics, Alumis Inc., Axoltis Pharma, Barricade Therapeutics, BioNxt Solutions, Eikonoklastes Therapeutics, 4D Pharma, Gossamer Bio, Pasithea Therapeutics, Synaptogenix, Monte Rosa Therapeutics, Immix Biopharma, f5 Therapeutics, Autobahn Therapeutics, Biosenic, Polpharma Biologics, Find Therapeutics, TeraImmun, AptaTargets, Trethera, Aditxt, SetPoint Medical, Sarepta Therapeutics, Nucleome Therapeutics, Vaccinex Inc., and others are evaluating new multiple sclerosis drugs to improve the treatment landscape.
Key Multiple Sclerosis Pipeline Therapies:GA Depot, Remibrutinib, Tolebrutinib, IMU 838, BCD-132, Apitox, Fenebrutinib, SAR 441344, CT-P53, CNM-Au8, Orelabrutinib, Vafidemstat, Temelimab, Elezanumab, NurOwn (MSC-NTF cells), PrimeC, SAR4433820, Ibudilast, BIIB091, Foralumab, ATL1102, RC18, ATA188, PIPE-307, Pirtobrutinib, LY3541860, Solriamfetol, Act-01, SCM-010, UMSC01, IMCY-0141, Lucid-MS, NeuroVax, LP-168, NB-4746, CC-97540, IMS-001, RO7121932, BMS-986196, LPX-TI641, MTR-601, IPG-11406, IPG-1094, NVG-291, CYMS-101, KYV-101, PIPE-791, GSK 3888130B, PTG-007, T 20K, BHV-8000, HuL001, Amethyst™, ANK 700, Arscimed, A-005, NX210c, Research programme: CAR-TREG, TASIN-1, Cladribine ODF, ET-101, MRx0002, GB7208, PAS-002, Bryostatin-1, MRT-6160, NXC-201, Research Program: Cytokine reduction, ABX-002, Arsenic trioxide, LL-341070, PB018, FTX 101, TI-235, TRE 515, NT-0007, NT-0002, NVG300, and others are under different phases of multiple sclerosis clinical trials.
Dive deep into rich insights for new drugs for multiple sclerosis treatment, visit @
Multiple Sclerosis Drugs
Table of Contents
For further information on the multiple sclerosis pipeline therapeutics, reach out @
Multiple Sclerosis Treatment Drugs
Related Reports
Multiple Sclerosis Market
Multiple Sclerosis Market Insights, Epidemiology, and Market Forecast – 2034 report deliver an in-depth understanding of the disease, historical and forecasted epidemiology, market share of the individual therapies, and key multiple sclerosis companies including
Immune Response BioPharma, Inc., Clene Nanomedicine, Genzyme, ImStem Biotechnology, Rho, Inc., Bristol-Myers Squibb, TG Therapeutics, Inc., Hoffmann-La Roche, Atara Biotherapeutics, Immunic AG, Celgene, Anokion SA, Sanofi, Actelion, Biogen, Supernus Pharmaceuticals, Inc., GeNeuro SA, HuniLife Biotechnology, Inc., Emerald Health Pharmaceuticals, RemeGen Co., Ltd., Antisense Therapeutics, Biocad, AB Science, Genentech, Novartis, Pipeline Therapeutics, ASLAN Pharmaceuticals, GlaxoSmithKline, Lucid Psycheceuticals, Voronoi, Hanmi Pharmaceutical, Mapi Pharma, f5 Therapeutics, Autobahn Therapeutics, AstraZeneca, ZyVersa Therapeutics, RedHill Biopharma, Gossamer Bio, Sarepta Therapeutics, BrainStorm Cell Limited, CytoDyn, Pear Therapeutics, Solstice Neurosciences, ProJenX, among others.
Multiple Sclerosis Epidemiology Forecast
Multiple Sclerosis Epidemiology Forecast – 2032 report delivers an in-depth understanding of the disease, historical and forecasted multiple sclerosis epidemiology in the 7MM, i.e., the United States, EU5 (Germany, Spain, Italy, France, and the United Kingdom), and Japan.
Relapsing Multiple Sclerosis Pipeline
Relapsing Multiple Sclerosis Pipeline Insight – 2024 report provides comprehensive insights about the pipeline landscape, pipeline drug profiles, including clinical and non-clinical stage products, and the key relapsing multiple sclerosis companies, including
ASLAN Pharmaceuticals, GlaxoSmithKline, Lucid Psycheceuticals, Voronoi, Hanmi Pharmaceutical, among others.
Relapsing-Remitting Multiple Sclerosis Pipeline
Relapsing-Remitting Multiple Sclerosis Pipeline Insight – 2024 report provides comprehensive insights about the pipeline landscape, pipeline drug profiles, including clinical and non-clinical stage products, and the key RRMS companies, including
TG Therapeutics, Novartis, Sanofi, Cinnagen, Polpharma Biologics, Immunic, Mapi Pharma, Biocad, Apimeds, Genentech (Roche), Merck, Immune Response BioPharma, Clene Nanomedicine, InnoCare Pharma, Oryzon Genomics, GeNeuro SA, AbbVie, Emerald Health Pharmaceuticals, GlaxoSmithKline, RedHill Biopharma, among others.
About DelveInsight
DelveInsight is a leading Business Consultant and Market Research firm focused exclusively on life sciences. It supports pharma companies by providing comprehensive end-to-end solutions to improve their performance. Get hassle-free access to all the healthcare and pharma market research reports through our subscription-based platform PharmDelve
.
Contact Us
Shruti Thakur
[email protected]
+14699457679
Logo:
SOURCE DelveInsight Business Research, LLP
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED

临床3期临床结果快速通道细胞疗法免疫疗法
2014-08-07
New Jersey’s Immune Response BioPharma, Inc. Unveils Plans To Develop In House Sales Force For HIV Blockbuster Remune
var switchTo5x=true;
stLight.options({publisher: "0341611e-38a4-415d-9e18-75e093ff27e0", doNotHash: false, doNotCopy: false, hashAddressBar: false});
August 7, 2014
By
Krystle Vermes
, BioSpace.com Breaking News Staff
Today, New Jersey-based
Immune Response BioPharma, Inc.
announced its plans
to create an in-house sales force for Remune, its HIV vaccine.
Remune is a therapeutic vaccine that is designed to block the immune system’s response to HIV antigens in people with the virus. The vaccination consists of dead HIV-1 particles that have been emulsified with Incomplete Freund’s Adjuvant, a mixture of mannide mono-oleate and a highly purified mineral oil.
In past trials, Remune has shown positive results in HIV-1 infected patients who were undergoing treatment. Previous tests show that Remune may also be administered safely in combination with other antiviral drugs.
“IRBP plans to develop its own sales force for Remune HIV/AIDS vaccine once the FDA approves our BLA application,” said IRBP CEO David Buswell. “Once approved and cleared for marketing authorization by the FDA, the teller window will open for us we may go it alone or partner with several big pharma players. We have an infrastructure in place to handle CGMP manufacturing with a total of six vendors.”
In the past, Remune has been administered to more than 2,000 patients in approximately 25 separate clinical trials. It has been well tolerated by patients, giving it a positive safety profile. Remune is also easy to give to patients through an injection in the deltoid muscle.
Clinical studies of Remune have induced an HIV-specific response, which researchers believe is necessary to controlling HIV replication. Patients receiving injections of Remune have demonstrated improvements in their percentage of CD4 cells, HIV-1 DNA in PBMCs, and weight.
“Those who bet against IRBP will lose and lose badly, especially those big pharma HIV drug makers,” Buswell continued. “They are like the dinosaur soon headed to extinction, they are goners and doomed once Remune is approved. I would get off those drugs if I had HIV once Remune is available, they are risky and too toxic to take indefinitely.”
IRBP has a
goal
of becoming the world leader in saving lives through vaccine technology. The company currently owns 100 percent of its drugs, treatments and vaccines through patents. IRBP believes that Remune should be considered a
vital part
of any treatment course for HIV/AIDS because of its proven track record in increasing the production of CD4+ T cell counts.
Read more recent
drug product news
.
var switchTo5x=true;
疫苗免疫疗法临床研究临床结果
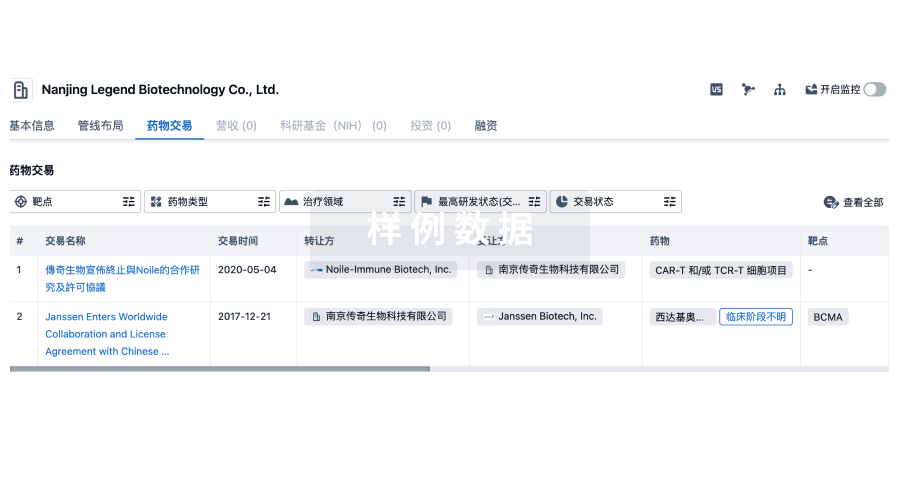
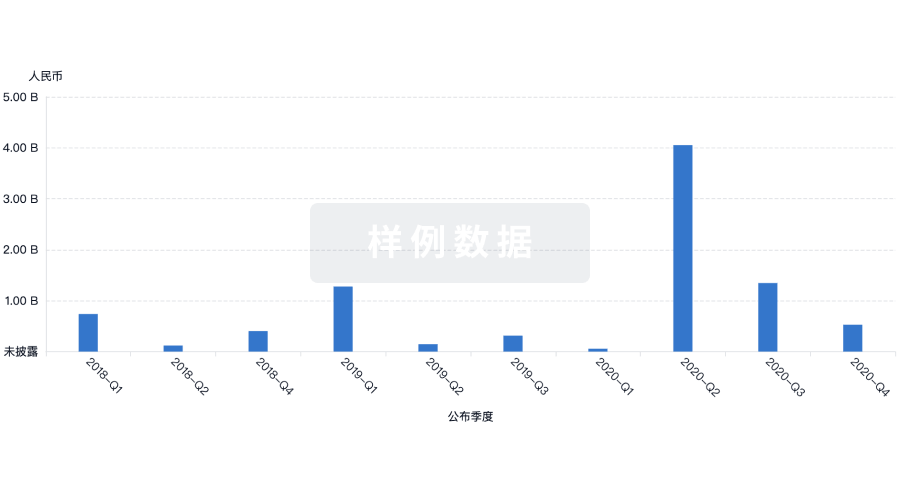
100 项与 Immune Response Biopharma, Inc. 相关的药物交易
登录后查看更多信息
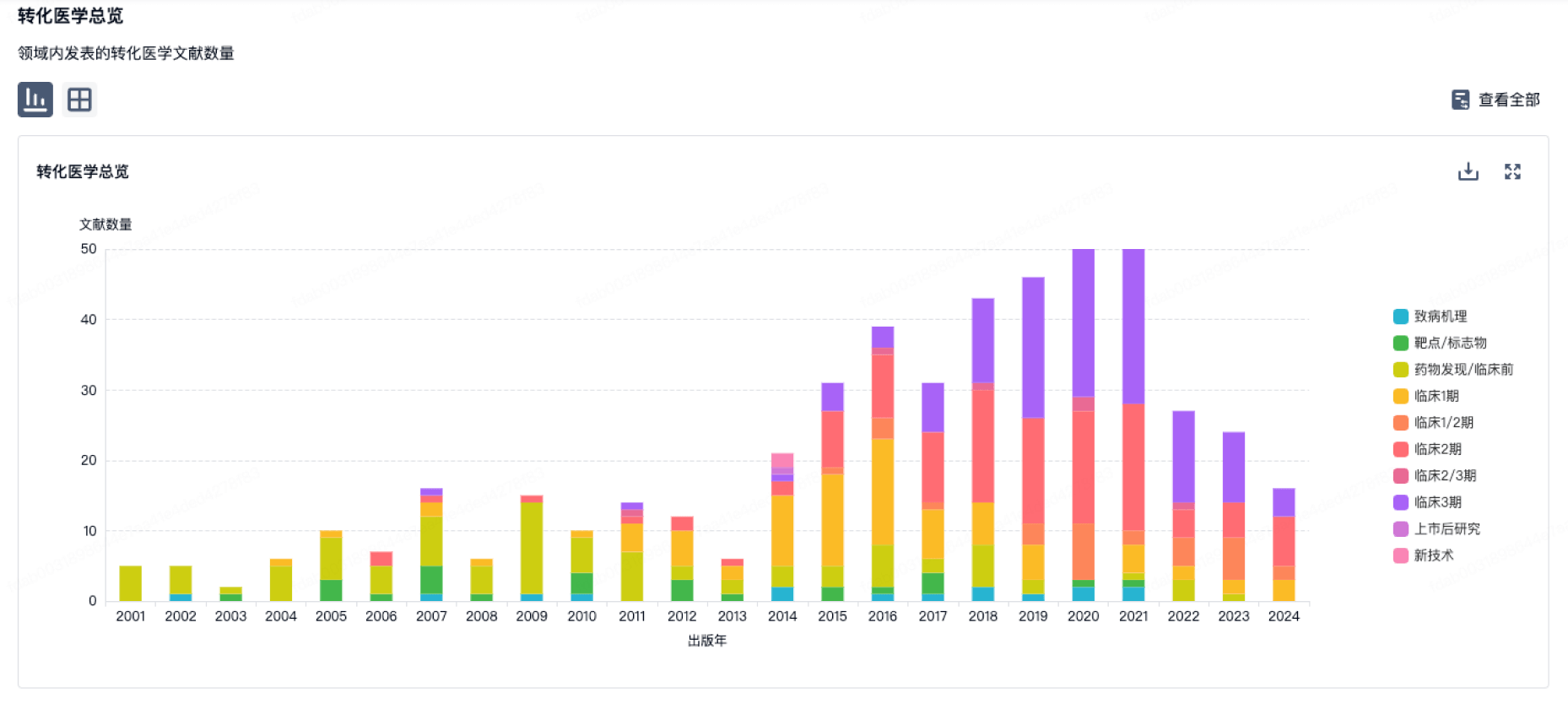
100 项与 Immune Response Biopharma, Inc. 相关的转化医学
登录后查看更多信息
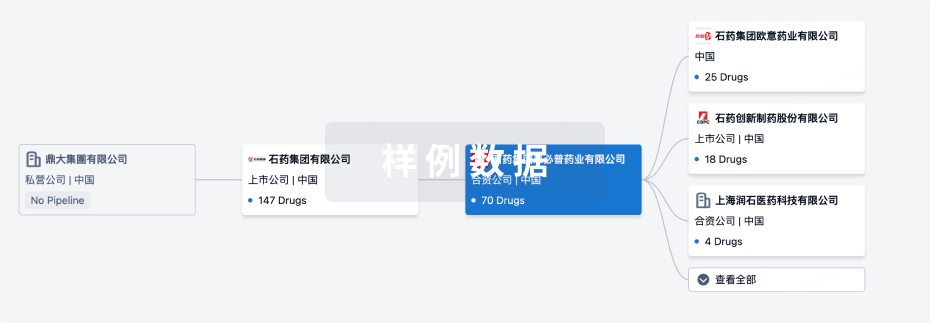
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年07月19日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
临床前
1
1
临床3期
其他
8
登录后查看更多信息
当前项目
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
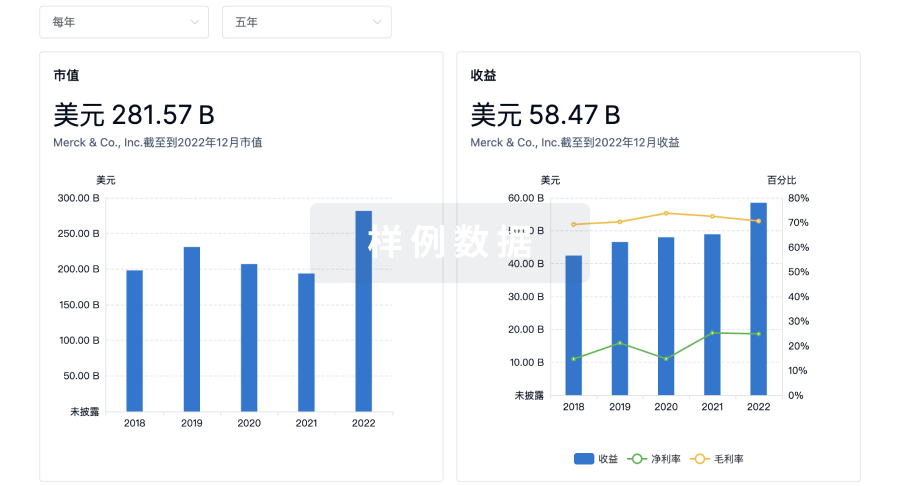
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
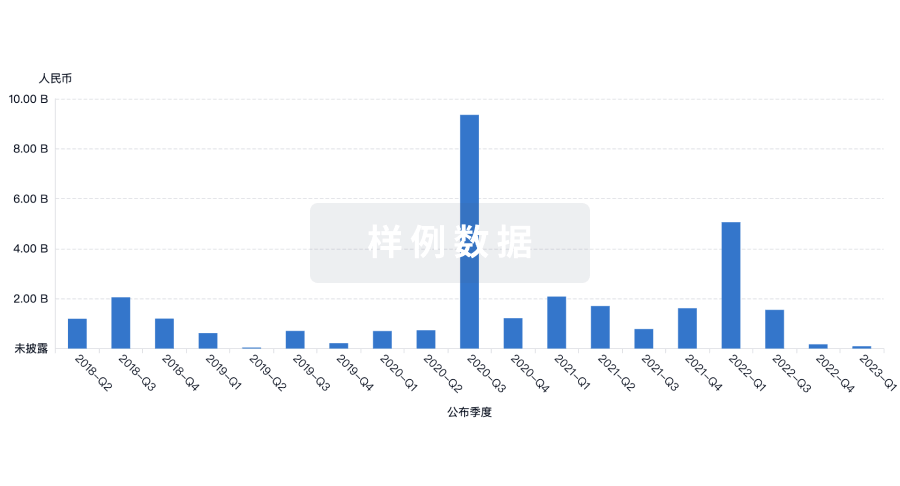
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用