预约演示
更新于:2025-05-07

Henan Provincial Cancer Hospital
更新于:2025-05-07
概览
关联
5
项与 Henan Provincial Cancer Hospital 相关的临床试验ChiCTR2500099667
Efficacy and Safety of All-Trans Retinoic Acid Combined with Decitabine for the Treatment of Refractory cancer treatment-induced Thrombocytopenia:a clinical study.
开始日期2025-03-31 |
ChiCTR2500099941
A single-arm, exploratory clinical study of tricacilli in preventing myelosuppression induced by platinum-containing chemotherapy in advanced non-small cell lung cancer - A single-arm, exploratory clinical study of tricacilli in preventing myelosuppression induced by platinum-containing chemotherapy in advanced non-small cell lung cancer
开始日期2024-04-02 |
ChiCTR1800014953
Clinical Study on the Safety and Efficacy of CD19CART Cell Therapy for Refractory B-Cell Leukemia
开始日期2018-02-24 |
100 项与 Henan Provincial Cancer Hospital 相关的临床结果
登录后查看更多信息
0 项与 Henan Provincial Cancer Hospital 相关的专利(医药)
登录后查看更多信息
24
项与 Henan Provincial Cancer Hospital 相关的文献(医药)2025-02-01·Journal of Clinical Oncology
Current status of physicians’ perception of HCC conversion/downstaging therapy: A nationwide survey in China.
作者: Bi, Xinyu ; Sun, Hui-Chuan ; Xue, Jianfeng ; Tan, Guang ; Zhao, Hai-Tao ; Huang, Tao ; Zhao, Ming ; Chen, Jinzhang ; Cai, Jianqiang ; Liang, Xiao ; Zhu, Xiao-Dong
2025-01-01·International Journal of Medical Sciences
A novel nomogram on predicting extrahepatic metastasis in colorectal cancer with liver metastasis for selective application of 18F-FDG PET/CT
Article
作者: Zhang, Bin ; Wang, Libo ; Zhu, Rongtao ; Wei, Sidong ; Zhao, Yipu ; Zhao, Jie
2024-11-05·Blood
Post Hoc Analysis of Phase III Gecacitinib Clinical Trial Outcomes: Enhanced Understanding and Implications
作者: Zhu, Huanling ; Zhang, Yi ; Suo, Shanshan ; Jiang, Zhongxing ; Zhang, Jin ; Li, Xin ; Du, Xin ; Xu, Na ; Li, Yarong ; Zhou, Hu ; Hong, Mei ; Yang, Linhua ; Wang, Jishi ; Jing, Hongmei ; Zhou, ZePing ; Zhang, Feng ; He, Aili ; Xiao, Zhijian ; Jin, Chenghao ; Liu, Lin ; Xu, Yajing ; Gao, Sujun ; Chen, Yuqing ; Liu, Qingchi ; He, Guangsheng ; Jiang, Qian ; Li, Yan ; Jin, Jie ; Wu, Wen ; Zheng, Cuiping ; Zhuang, Junling ; Yue, Lingling ; Wu, Dengshu
100 项与 Henan Provincial Cancer Hospital 相关的药物交易
登录后查看更多信息
100 项与 Henan Provincial Cancer Hospital 相关的转化医学
登录后查看更多信息
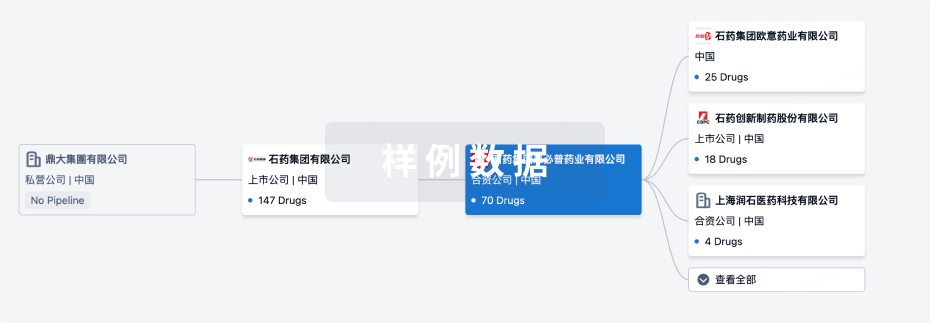
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年07月21日管线快照
无数据报导
登录后保持更新
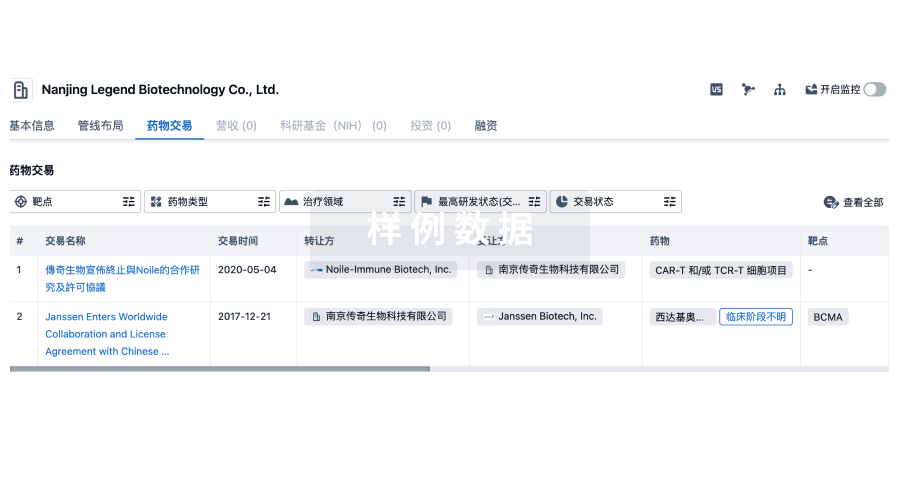
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
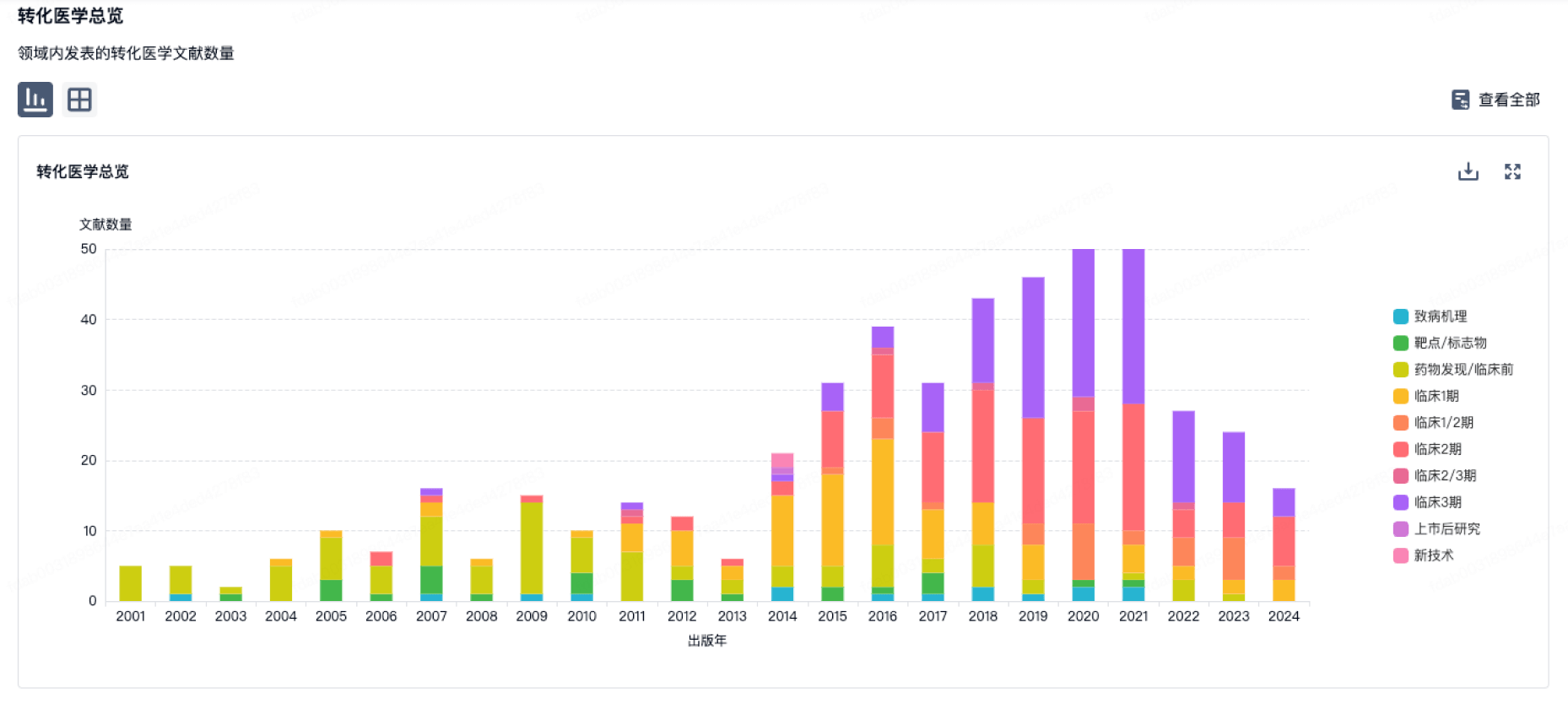
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
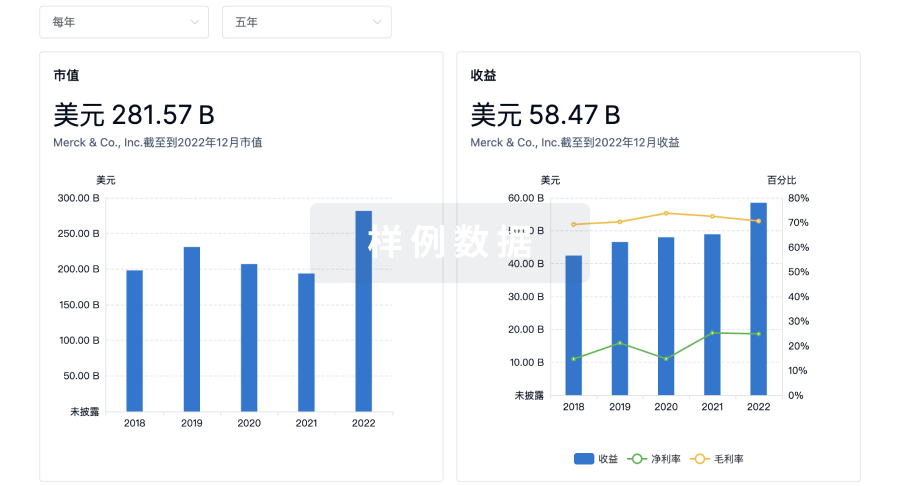
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用