预约演示
更新于:2025-05-07

Northeast Ohio Medical University
更新于:2025-05-07
概览
关联
1
项与 Northeast Ohio Medical University 相关的药物靶点 |
作用机制 TRPV1拮抗剂 |
在研机构- |
原研机构 |
在研适应症- |
最高研发阶段无进展 |
首次获批国家/地区- |
首次获批日期- |
4
项与 Northeast Ohio Medical University 相关的临床试验NCT05702762
Single Dose Aminoglycosides for Acute Uncomplicated Cystitis in the Emergency Department Setting
The purpose of this research study is to determine if gentamicin is as effective treatment of acute uncomplicated cystitis (urinary tract infection) using aminoglycosides versus the current standards of care. The current standards of care in our region are often to prescribe a multi-day antibiotic prescription that is taken multiple times per day whereas gentamicin will be a one-time dose in the emergency department. Gentamicin is the medicine being studied.
开始日期2022-10-01 |
申办/合作机构  Mercy Health Mercy Health [+1] |
NCT00979784
The Better Weight-Better Sleep Study: A Pilot Intervention in Primary Care
The hypothesis of this study is that overweight and obese patients exposed to sleep focused counseling and standard dietary and exercise counseling will have better outcomes than similar patients exposed to standard dietary and exercise counseling only.
开始日期2009-04-01 |
申办/合作机构 |
NCT00258492
The Prevalence and Outcomes of Restless Legs Syndrome Among Veterans - Exercise Intervention
A pilot study of an aerobic exercise intervention to moderate symptoms and improve sleep quality among patients with Restless Legs Syndrome (RLS). We, the researchers at Northeastern Ohio Universities College of Medicine, hypothesize that, relative to a control group, RLS sufferers who participate in an aerobic exercise intervention will demonstrate:
reduced RLS symptoms;
improved sleep quality;
reduced daytime sleepiness.
reduced RLS symptoms;
improved sleep quality;
reduced daytime sleepiness.
开始日期2005-12-01 |
申办/合作机构 |
100 项与 Northeast Ohio Medical University 相关的临床结果
登录后查看更多信息
0 项与 Northeast Ohio Medical University 相关的专利(医药)
登录后查看更多信息
5,758
项与 Northeast Ohio Medical University 相关的文献(医药)2025-12-01·Immunologic Research
Hepatitis C associated mixed cryoglobulinemia glomerulonephritis in the setting of undetectable viral load: successful treatment with hydroxychloroquine and review of the literature
Review
作者: Khan, Khadeja ; Shweikeh, Faris ; Mouchli, Mohamad ; Singh, Inderprit ; Torres, Yaritza
2025-11-01·Journal of Orthopaedics
Postoperative complications rates and outcomes following total hip arthroplasty in patients with ankylosing spondylitis: A systematic review
Review
作者: Anaspure, Omkar ; Sheth, Neil P ; Eachempati, Krishna K ; Patel, Shiv ; Newsom, Andrew ; Smith, Weston ; Baumann, Anthony N
2025-06-01·Currents in Pharmacy Teaching and Learning
Pharmacy faculty and students perceptions of artificial intelligence: A National Survey
Article
作者: Singh, Divita ; Hintze, Trager D ; Rowe, Casey ; Bernknopf, Allison ; Showman, Leanne ; Abdel Aziz, May H ; Gustafson, Kyle A ; Chu, Angela ; Mohamed, Islam ; Dave, Vivek ; Ogunsanya, Motolani E ; Jones, Ellen ; Berman, Sarah ; Devraj, Radhika ; Nogid, Anna ; Munir, Faria ; Hoffman, Alexander ; Brand-Eubanks, Damianne ; Gavaza, Paul ; Prudencio, Jarred ; Southwood, Robin ; Miller, Victoria
30
项与 Northeast Ohio Medical University 相关的新闻(医药)2025-03-10
MONDAY, March 10, 2025 -- For patients with type 2 diabetes (T2D), glucagon-like peptide-1 receptor agonist (GLP-1 RA) use is associated with a reduced risk for developing hematologic cancers compared with insulin and metformin use, according to a research letter published online March 6 in
JAMA Network Open
.
Omer S. Ashruf, from Northeast Ohio Medical University in Rootstown, and colleagues conducted a retrospective cohort study to compare the risks for hematologic cancers in patients with T2D treated with a GLP-1 RA versus metformin and insulin. The study included patients with T2D prescribed a GLP-1 RA, insulin, or metformin between April 30, 2005, and Oct. 31, 2023 (51,617; 611,115; and 938,602 patients, respectively). Groups were independently matched using a nearest neighbor greedy matching algorithm; 47,716 patients were included in the GLP-1 RA-insulin analysis and 50,590 were included in the GLP-1 RA-metformin analysis.
The researchers found that GLP-1 RA use was associated with significantly lower risks for of myelodysplastic syndromes (MDS) and myeloproliferative neoplasms (MPN) compared with metformin (hazard ratios, 0.61 and 0.67, respectively). No significant difference was seen in the risk for any other hematologic cancer. GLP-1 RA use was associated with significantly lower risks for myeloid leukemia, lymphoid leukemia, non-Hodgkin lymphoma, MDS, MPN, monoclonal gammopathy, multiple myeloma, and amyloidosis compared with insulin (hazard ratios, 0.39, 0.45, 0.42, 0.19, 0.50, 0.68, 0.49, and 0.52, respectively). GLP-1 RA use was associated with a 54 percent lower risk than that seen with insulin across all hematologic cancers.
"The findings of this cohort study suggest that GLP-1 RAs are associated with reduced risk of developing several hematologic cancers, particularly MDS and MPN, in patients with T2D," the authors write.
One author disclosed ties to Celegene, BMS, and Carobou.
Abstract/Full Text
Whatever your topic of interest,
subscribe to our newsletters
to get the best of Drugs.com in your inbox.
临床结果临床研究
2025-01-27
SECAUCUS, N.J. and CLEVELAND, Jan. 27, 2025 /PRNewswire/ -- Quest Diagnostics (NYSE: DGX), a leading provider of diagnostic information services, today announced it has completed its previously announced acquisition of select assets of University Hospitals, one of the nation's leading nonprofit health systems and academic medical centers. Financial terms were not disclosed.
With the acquisition, Quest broadens access to its industry-leading and innovative test menu, network of convenient patient access sites and broad health plan coverage in Ohio.
For University Hospitals' providers and patients using Quest for lab services, Quest's laboratories in Twinsburg, Ohio and Pittsburgh, Pennsylvania will perform the testing. University Hospitals will continue to provide all inpatient and select outpatient testing from its hospital-based labs.
About Quest Diagnostics
Quest Diagnostics works across the healthcare ecosystem to create a healthier world, one life at a time. We provide diagnostic insights from the results of our laboratory testing to empower people, physicians and organizations to take action to improve health outcomes. Derived from one of the world's largest databases of de-identifiable clinical lab results, Quest's diagnostic insights reveal new avenues to identify and treat disease, inspire healthy behaviors and improve healthcare management. Quest Diagnostics annually serves one in three adult Americans and half the physicians and hospitals in the United States, and our more than 50,000 employees understand that, in the right hands and with the right context, our diagnostic insights can inspire actions that transform lives and create a healthier world. www.QuestDiagnostics.com.
About University Hospitals / Cleveland, Ohio
Founded in 1866, University Hospitals serves the needs of patients through an integrated network of more than 20 hospitals (including five joint ventures), more than 50 health centers and outpatient facilities, and over 200 physician offices in 16 counties throughout northern Ohio. The system's flagship quaternary care, academic medical center, University Hospitals Cleveland Medical Center, is affiliated with Case Western Reserve University School of Medicine, Northeast Ohio Medical University, Oxford University, Taiwain University and the Technion Israel Institute of Technology. The main campus also includes the UH Rainbow Babies & Children's Hospital, ranked among the top children's hospitals in the nation; UH MacDonald Women's Hospital, Ohio's only hospital for women; and UH Seidman Cancer Center, part of the NCI-designated Case Comprehensive Cancer Center. UH is home to some of the most prestigious clinical and research programs in the nation, with more than 3,000 active clinical trials and research studies underway. UH Cleveland Medical Center is perennially among the highest performers in national ranking surveys, including "America's Best Hospitals" from U.S. News & World Report. UH is also home to 19 Clinical Care Delivery and Research Institutes. UH is one of the largest employers in Northeast Ohio with more than 30,000 employees. Follow UH on LinkedIn, Facebook and Twitter. For more information, visit UHhospitals.org.
并购诊断试剂临床研究
2025-01-02
Regeneron, maker of the blockbuster ophthalmology medicine Eylea, has acquired an ocular biotech, the large biopharma confirmed to
Endpoints News
on Thursday.
The London-area biotech, named Oxular, was bought last month, according to board member and recently departed CEO Mark Gaffney. He
posted
about the deal on LinkedIn on Thursday afternoon. Gaffney is now CEO of inflammation and fibrosis biotech Calluna Pharma.
Regeneron had not previously announced the deal, a company spokesperson confirmed in an email. The New York-based drugmaker plans to disclose more details in its next quarterly filing, the spokesperson added.
“This was a targeted acquisition that provides us with a potential best-in-class delivery device for our future ocular gene therapies, with the goal of accelerating the time it will take to reach clinical readiness,” the Regeneron spokesperson wrote. Terms of the deal were not disclosed.
Regeneron’s clinical-stage gene therapy pipeline currently revolves around a hearing loss program. Oxular could help with its expansion. Regeneron also inked a retinal gene therapy pact with
German biotech ViGeneron
in April 2022. Ophthalmology has long been a cornerstone of Regeneron’s business. The pharmaceutical company reported
$1.53 billion
in sales of
Eylea
and its high-dose counterpart (marketed as
Eylea HD
) in the most recent quarter.
Oxular was developing a biodegradable polymer system and a semi-automated ocular administration device to help extend the duration of eye disease treatments to about 12 months. It had been in Phase 2 development and was
exploring treatments
for diabetic macular edema, retinoblastoma, uveal melanoma, age-related macular degeneration and diabetic retinopathy. Regeneron declined to comment on whether it would continue advancing any of Oxular’s pipeline programs, including OXU-001, OXU-003, OXU-004 and OXU-005.
The startup last disclosed a
$37 million
funding round in March 2021. It was backed by Dutch investor Forbion, IP Group, NeoMed and V-Bio Ventures.
Regeneron hasn’t been as acquisitive, or doled out the same price tags, as some of its pharma peers in recent years. In early 2024, it bought
the R&D unit from 2seventy bio
. In 2023, it
acquired
hearing loss gene therapy maker Decibel Therapeutics, and in 2022, it
snagged Checkmate Pharmaceuticals
.
并购基因疗法临床2期高管变更
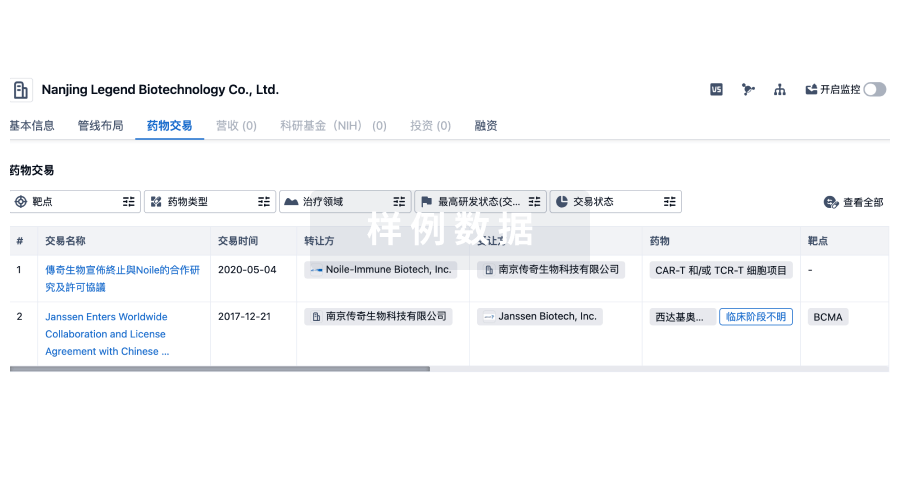
100 项与 Northeast Ohio Medical University 相关的药物交易
登录后查看更多信息
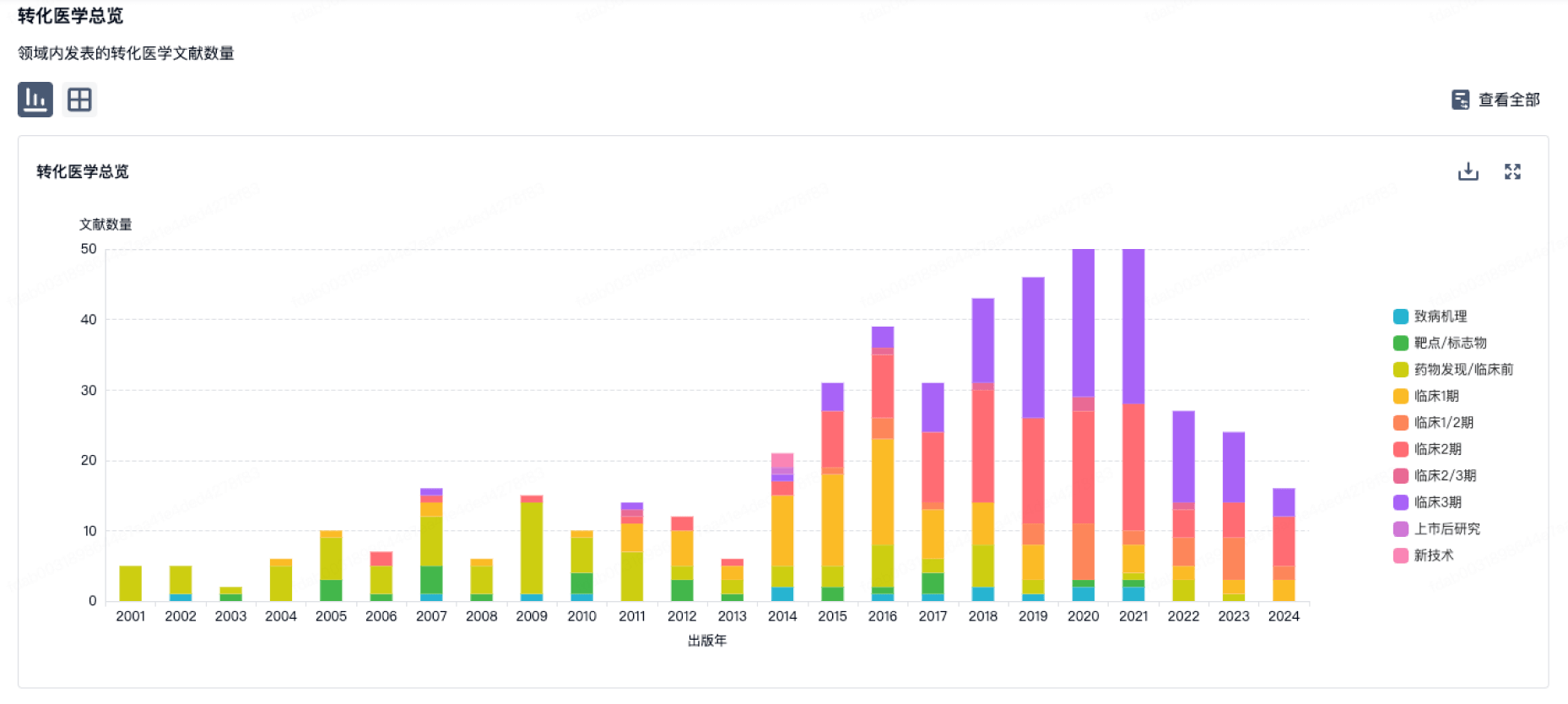
100 项与 Northeast Ohio Medical University 相关的转化医学
登录后查看更多信息
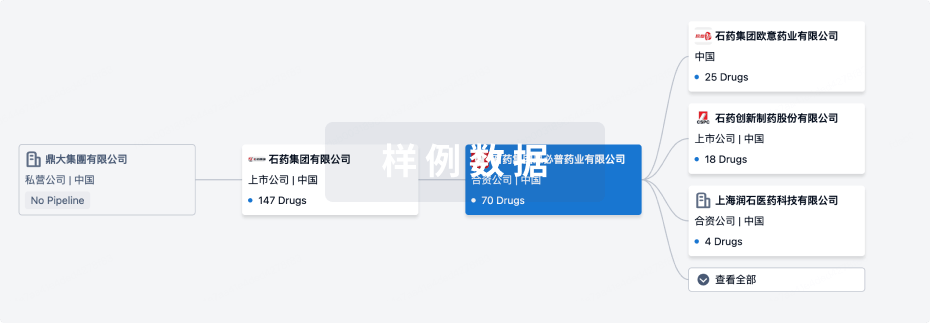
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年08月29日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
其他
1
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
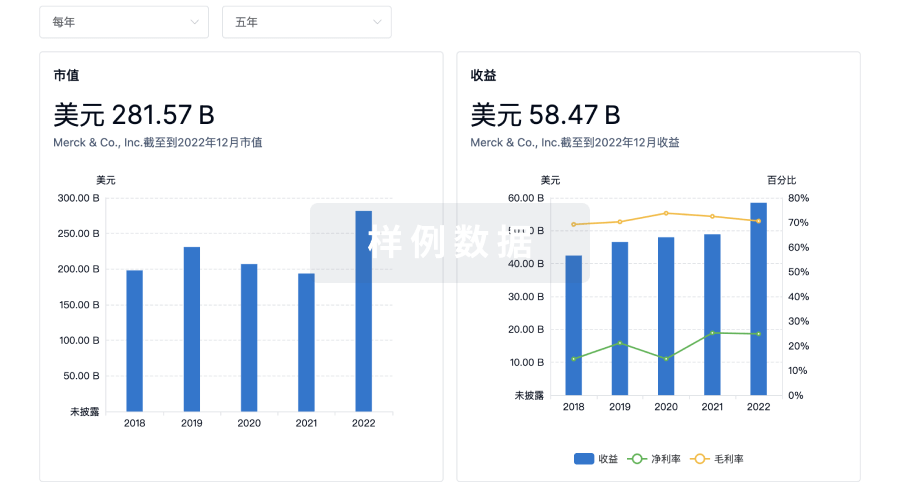
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
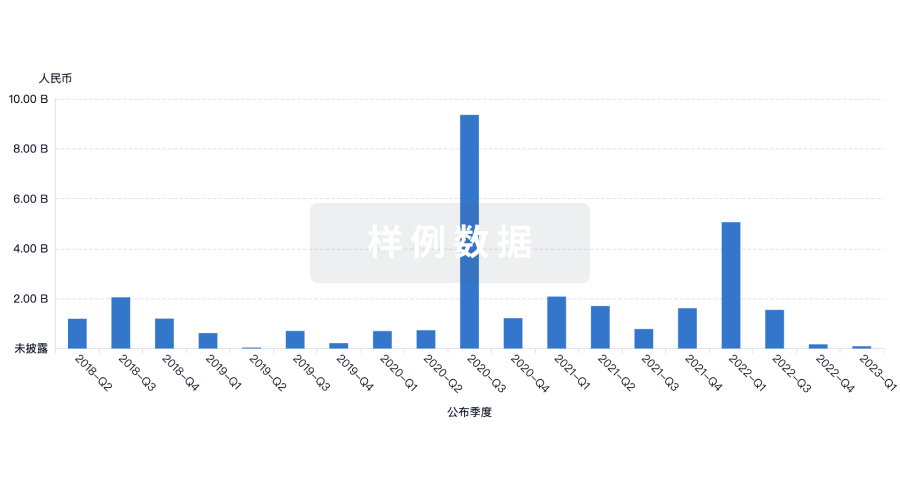
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

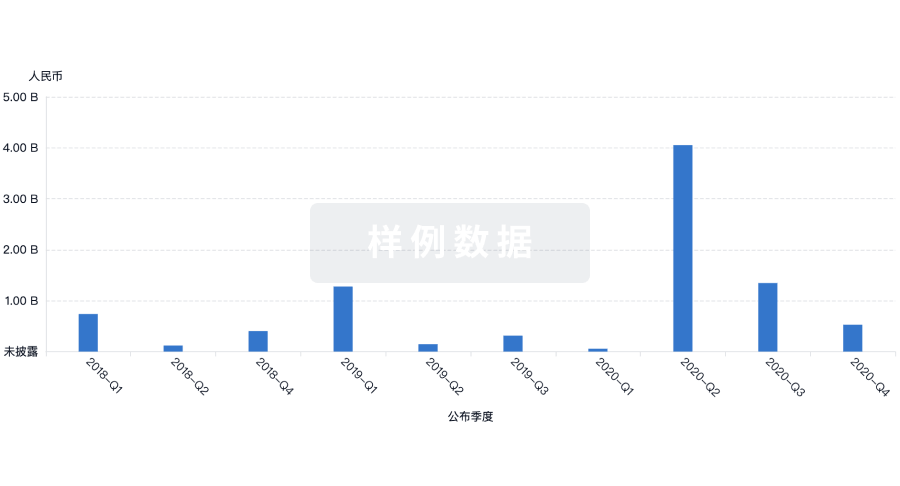
投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用

