Preventing Liver Recurrence After Partial Hepatectomy for Intrahepatic Cholangiocarcinoma Using Adjuvant Hepatic Arterial Infusion Pump Chemotherapy - PUMP IV Trial
The goal of this clinical trial is to learn if additional chemotherapy by means of a chemo pump can prevent return of disease in adult patients with bile duct cancer in the liver that can be treated with surgery. The main questions it aims to answer are:
* Does addition of chemotherapy by means of a chemo pump lead to less return of disease within the liver two years after surgery?
* Does addition of chemotherapy by means of a chemo pump lead to longer survival of patients?
* Does addition of chemotherapy by means of a chemo pump lead to an increase in quality of life?
Participants will receive an implanted chemo pump, through which additional chemotherapy will be given to the liver in addition to surgery.
DIRECT-2: Fasting Mimicking Diet Program to ImpRovE ChemoTherapy in HR+, HER2- Breast Cancer
In preclinical research, short-term fasting (STF) protects tumor-bearing mice against the toxic effects of chemotherapy, improves the CD8+ effector T-cell intratumor infiltration, while enhancing the chemotherapy efficacy. Short-term use of a "fasting-mimicking diet" (FMD) caused a major increase in the efficacy of cancer treatment in mice comparable to STF. In humans, the investigators recently performed a multicenter randomized phase II trial showing that patients with Human Epidermal growth factor Receptor 2 (HER2) negative breast cancer treated with neoadjuvant chemotherapy and FMD displayed a better radiological response and a better pathological response (90-100% vs <90% tumor cell reduction) than patients treated with chemotherapy without FMD (de Groot, Nat Commun 2020; NCT02126449). Therefore these findings will be validated in a phase 3 trial with the underlying hypothesis that FMD during neoadjuvant chemotherapy for breast cancer improves clinical outcomes, potentially due to improved local immunity.
/ Active, not recruitingN/AIIT DRAGON 1- Training, Accreditation, Implementation and Safety Evaluation of Portal and Hepatic Vein Embolization to Accelerate Future Liver Remnant (FLR) Hypertrophy
Brief Summary: Some colorectal liver metastases can only be resected after inducing liver regeneration by portal vein embolization (PVE) to increase size function of the future liver remnant (FLR). While PVE is standard, embolization of portal vein and hepatic veins (PVE/HVE) on one side of the liver may faster and more extensive liver size and function growth. PVE/HVE is a novel procedure and requires a safety and feasibility evaluation in a pretrial (DRAGON1) to then be compared in a randomized controlled trial (RCT) to PVE (DRAGON 2).
100 项与 Stichting Koningin Wilhelmina Fonds Voor de Nederlandse 相关的临床结果
0 项与 Stichting Koningin Wilhelmina Fonds Voor de Nederlandse 相关的专利(医药)
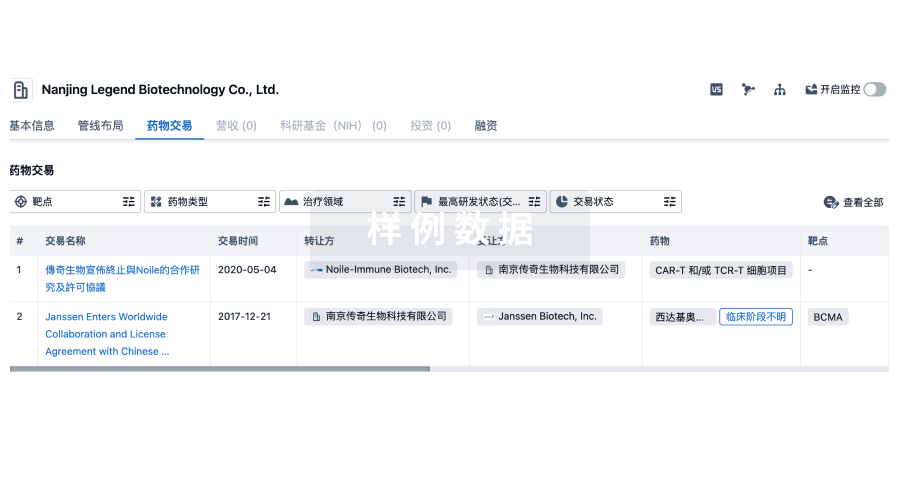
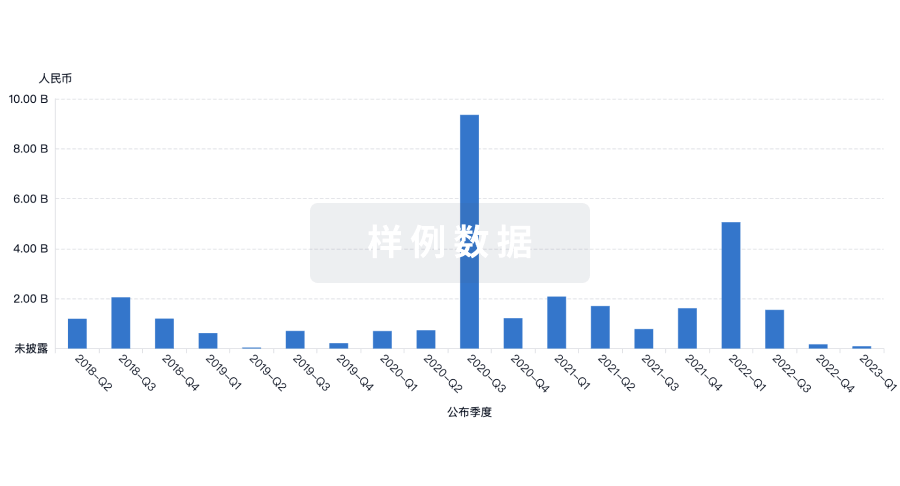
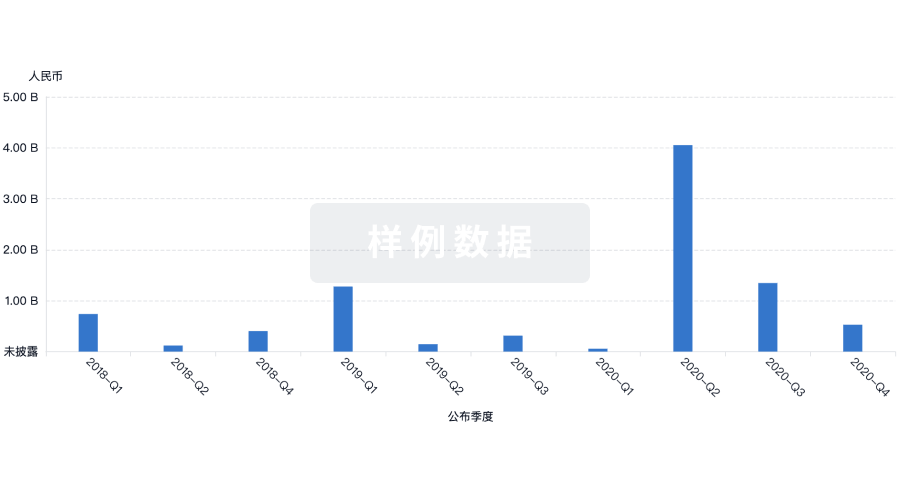
100 项与 Stichting Koningin Wilhelmina Fonds Voor de Nederlandse 相关的药物交易
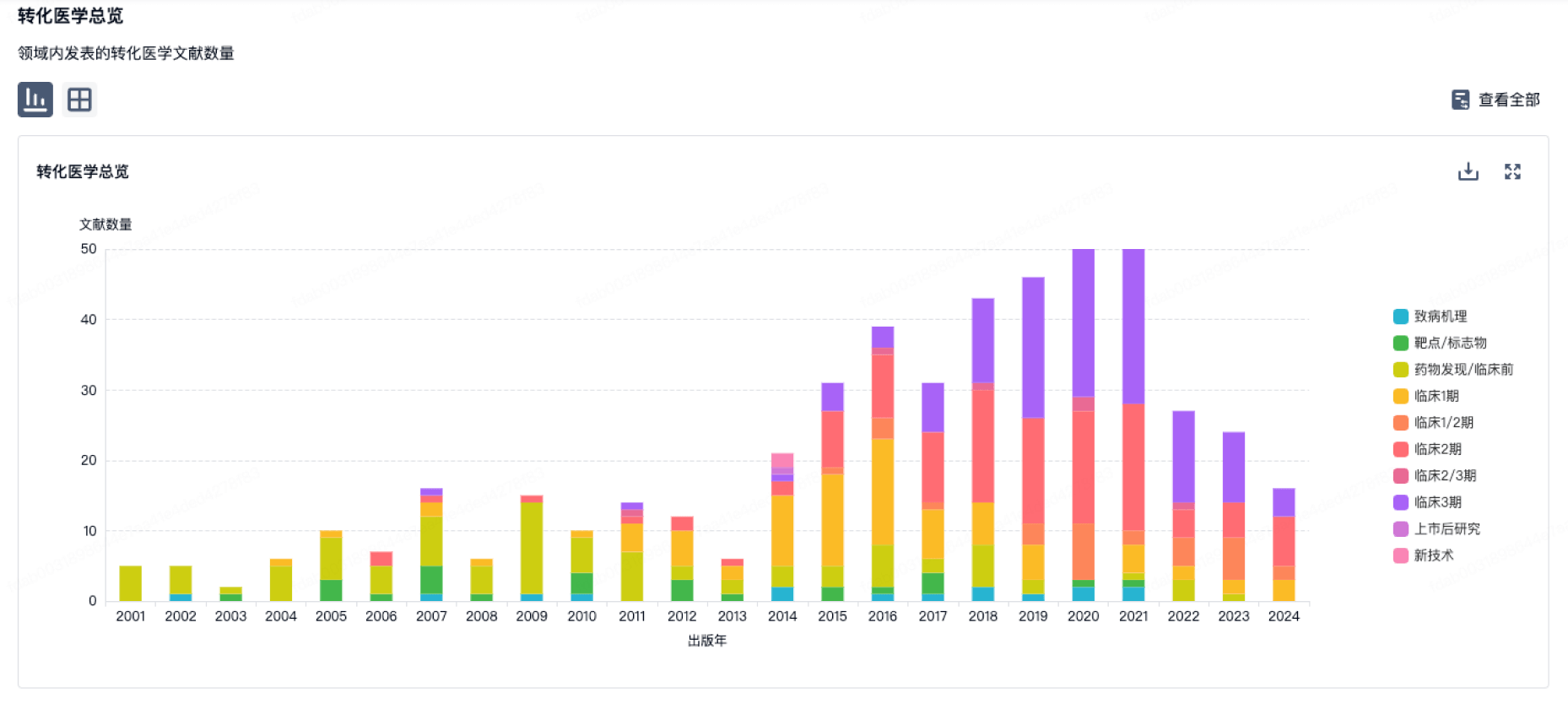
100 项与 Stichting Koningin Wilhelmina Fonds Voor de Nederlandse 相关的转化医学