更新于:2024-11-01

NeuroTrauma Sciences LLC
更新于:2024-11-01
概览
标签
心血管疾病
神经系统疾病
其他疾病
小分子化药
关联
7
项与 NeuroTrauma Sciences LLC 相关的药物靶点- |
作用机制- |
在研机构 |
非在研适应症- |
最高研发阶段临床1期 |
首次获批国家/地区- |
首次获批日期- |
靶点- |
作用机制- |
在研机构 |
原研机构 |
在研适应症 |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期- |
靶点- |
作用机制- |
在研机构 |
原研机构 |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期- |
1
项与 NeuroTrauma Sciences LLC 相关的临床试验A Single-Center, Randomized, Placebo-Controlled, Single Ascending Dose Trial to Evaluate the Safety, Tolerability, and Pharmacokinetics of Intravenous Nts-104 Tris in Healthy Adults
NTS-104 TRIS will be administered as a single intravenous dose to healthy subjects at doses of 0.8, 4, 8 and 16 mg/kg in 4 Cohorts. Each cohort of 8 subjects will begin with dosing 2 sentinel subjects with one being given the investigational product and one the placebo. If no safety issues arise, dosing the remaining subjects in the cohort will begin. A Safety Review Committee will review the safety and pharmacokinetic data before approving escalation to the next dose level.
开始日期2023-04-28 |
申办/合作机构  NeuroTrauma Sciences LLC初创企业 NeuroTrauma Sciences LLC初创企业 [+1] |
100 项与 NeuroTrauma Sciences LLC 相关的临床结果
登录后查看更多信息
0 项与 NeuroTrauma Sciences LLC 相关的专利(医药)
登录后查看更多信息
8
项与 NeuroTrauma Sciences LLC 相关的新闻(医药)2024-01-09
[09-January-2024]
David Lawrence Departs as CFO; Appointed to Board of Directors
ATLANTA, Jan. 9, 2024 /PRNewswire/ -- NeuroTrauma Sciences, LLC (NTS), a private biopharmaceutical company developing neuroprotective therapeutics for treating central nervous system (CNS) injuries including stroke and traumatic brain injury, today announced the appointment of William Fricker, CPA, MBA, to Chief Financial Officer, effective immediately. In this position, Mr. Fricker will assume responsibility for the oversight of NTS's financial strategy and operations.
NeuroTrauma Sciences Appoints William Fricker, CPA, MBA, as Chief Financial Officer
David Lawrence has stepped down from the full-time CFO position at NeuroTrauma Sciences. He will remain as a consultant and has been appointed to the Board of Directors.
Mr. Fricker brings to NTS more than 25 years of financial expertise across industries, including pharmaceutical and biotechnology companies, most recently as Chief Financial Officer for Eleison Pharmaceuticals and NeuroRx. In addition, he served as Vice President, Finance & Principal Accounting Officer for Immunomedics, where he supported the transition from a clinical-stage organization to a fully commercial biopharmaceutical company through its acquisition by Gilead in 2020. There he also managed over $600 million in equity raises. Earlier in his career, he held finance and accounting positions at Johnson & Johnson Corporation and Bristol-Myers Squibb Company, as well as Coopers & Lybrand. Mr. Fricker holds a Bachelor of Science in Accounting from Penn State University and a Master of Business Administration from Villanova University. He is a Certified Public Accountant.
"NTS is developing neuroprotective compounds in the critically underserved areas of stroke and traumatic brain injury, and I am honored to join the company and leverage my expertise to contribute to its success," said Mr. Fricker. "I look forward to partnering with the team to execute on its strategy and help realize the potential of investigational drug NTS-104."
"Throughout Bill's significant industry tenure, he has improved financial discipline and supported the finance and operational functions of companies at all stages," said Carl Long, Chief Executive Officer. "We are pleased to welcome him to our executive leadership team at an important time in the company's growth."
Mr. Long continued, "We also thank Dave Lawrence for his contributions to NTS, for his strategic leadership and integrity in the financial management of the company, and we look forward to continue working with him in another capacity."
About NeuroTrauma Sciences
NeuroTrauma Sciences is a biopharmaceutical company advancing its mission to develop neuroprotective therapies for treating CNS injuries, including ischemic stroke and traumatic brain injury (TBI). Acquired brain injuries remain areas of high unmet need with limited therapeutic options to alleviate the cognitive, functional, and neurobehavioral effects for millions of patients worldwide. By leveraging insights into the biology of acquired brain injury, NTS is advancing a pipeline of candidates targeting ischemic stroke and TBI. For additional information, please visit .
Contacts:
NeuroTrauma Sciences
William Fricker, CPA, MBA
Chief Financial Officer
M: 215-622-7875
w.fricker@neurotraumasciences.com
SMP Communications
Susan Pietropaolo
M: 201-923-2049
susan@smpcommunications.com
高管变更并购
2023-11-14
Monitoring brain injury biomarkers and glucose variation in patients who have suffered an acute cranial injury during the entire first week of hospitalization can provide a more accurate picture of the pathological process.
Monitoring brain injury biomarkers and glucose variation in patients who have suffered an acute cranial injury during the entire first week of hospitalisation can provide a more accurate picture of the pathological process. This is according to a paper by researchers at Karolinska Institutet in Sweden published in The Lancet Neurology. It is hoped that their findings can eventually lead to more personalised treatment.
After samples of brain injury markers and glucose have been taken over the entire first week of intensive care, patients with traumatic brain injury can be divided into different groups with different disease trajectories and prognoses.
“This could one day be used to identify different therapies for these different groups, who currently receive effectively the same treatment,” says the study’s first author Cecilia Åkerlund, anaesthetist and intensive care specialist at Karolinska University Hospital in Solna and researcher at the Department of Physiology and Pharmacology, Karolinska Institutet, Sweden.
She shows in her study that an advanced clustering method can be used to divide patients into six groups by sample data. In the group with the best prognosis, only four per cent died after six months, as opposed to a full 65 per cent in the group with the worst prognosis after the same time – 41 per cent during the first week.
Many hospitals now use a model based on different factors from the patients’ day of admission to assess their prognoses.
“Our study shows that more information gathered over a longer time might be needed to assess the patients,” she says.
The variation between the highest and lowest glucose variation during the day was one of the key metrics used to characterise the patients, something to which little attention is paid today. The same is true of the relevant biomarkers, which are also generally ignored during the first week of admission. Karolinska University Hospital, however, is an exception:
“We clinically monitor certain brain injury biomarkers daily,” says Dr Åkerlund. “But we are one of few hospitals in the world to do so, as far as I’m aware.”
“Our study supports the notion that serial brain injury biomarkers can play an important part in monitoring the disease trajectory in our brain injury patients,” says the study’s last author David Nelson, consultant at Karolinska University Hospital’s neurocritical care unit and researcher at Karolinska Institutet.
At the same time, Dr Åkerlund acknowledges that more research is needed on both the biomarkers and the patient groupings before the method can be recommended on a broad front.
“These results need to be corroborated by larger studies and with other patient groups to show that the method is stable,” she says. “If we can do this, it will be an important step towards being better able to personalise the treatment of patients with primarily moderate and severe traumatic brain injuries.”
The study was financed by grants from the EU’s Seventh Framework Programme, Hannelore Kohl Stiftung, OneMind, Integra LifeSciences Corporation and NeuroTrauma Sciences.
David K. Menon has reported financial relations with several pharmaceutical companies unrelated to this study; Shubhayu Bhattacharyay has reported research grants from the Gates Cambridge Foundation, Peter Smielewski software licence revenue, and Ewout Steyerberg royalties from Springer publishing house. All other researchers report no conflicts of interest.
Facts:
Acute cranial injury, or traumatic brain injury, affects men and women of all ages and for all types of reasons; however, patients are commonly in the younger age bracket following a traffic accident or the older following a fall. Seventy-five per cent are men. The study used data from the European multicentre study CENTER-TBI, the largest-ever observational study of traumatic brain injury. Frozen samples from over 1,700 patients were post-analysed. The researchers then used an advanced clustering method to create the different groups that best described the pathological process to optimise the groupings. Source: Cecilia Åkerlund.
Publication: “Clinical descriptors of disease trajectories in patients with traumatic brain injury in the intensive care unit (CENTER-TBI): a multicentre observational cohort study”, Cecilia A.I. Åkerlund, Anders Holst, Shubhayu Bhattacharyay, Nino Stocchetti, Ewout Steyerberg, Peter Smielewski, David K. Menon, Ari Ercole, David W. Nelson, The Lancet Neurology, online 14 November 2023, doi: 10.1016/S1474-4422(23)00358-7.
2023-07-31
Accomplished Business Development and Licensing Executive to Drive NTS's Business Development and Partnering Activities
ATLANTA, July 31, 2023 /PRNewswire/ -- NeuroTrauma Sciences, LLC (NTS), a private biopharmaceutical company developing neuroprotective therapeutics for treating central nervous system (CNS) injuries, including stroke and traumatic brain injury, today announced the appointment of Kevin Pong, PhD, MBA as Chief Business Officer. In this position, Dr. Pong is responsible for the strategic leadership of the company's global business development, licensing, and alliance management activities.
"We are delighted to welcome Kevin to our executive leadership team," said Carl Long, Chief Executive Officer. "His deep experience in business development and partnering strategy and ability to foster strong business relationships, combined with a background in neuroscience, will be valuable as we progress our lead program NTS-104 in stroke through the clinic and advance our vital work in traumatic brain injury."
Dr. Pong brings to NTS more than 20 years of industry experience with a successful track record of business development and licensing transactions in biotech and pharmaceutical companies. Most recently, he served as Chief Business Officer of Anima Biotech, where he drove multiple transformative transactions and helped evolve the company's partnering strategy. Prior to Anima, he served as vice president of business development, licensing, and alliance management at Summit Therapeutics and led the identification, evaluation, and negotiation of CNS business development opportunities at Sunovion Pharmaceuticals. He spent several years at Endo Pharmaceuticals in business development roles of increasing responsibility and held leadership roles in discovery neuroscience research at Wyeth. Dr. Pong holds a B.S. in Biological Sciences, a Ph.D. in Neuroscience from the University of Southern California, and an MBA from Rutgers University.
"I am excited by the potential I see in NTS and the opportunity to be a part of the team advancing compounds in the critically underserved areas of stroke and traumatic brain injury," said Dr. Pong. "I am delighted to be working in the neuroscience field again and look forward to leveraging my expertise and network."
About NeuroTrauma Sciences
NeuroTrauma Sciences is a biopharmaceutical company advancing its mission to develop neuroprotective therapies for treating CNS injuries, including ischemic stroke and traumatic brain injury (TBI). Acquired brain injuries remain areas of high unmet need with limited therapeutic options to alleviate the cognitive, functional, and neurobehavioral effects for millions of patients worldwide. By leveraging insights into the biology of acquired brain injury, NTS is advancing a pipeline of candidates targeting ischemic stroke and TBI. For additional information, please visit .
Contacts:
NeuroTrauma Sciences
David Lawrence
Chief Financial Officer
M: 845-548-6311
[email protected]
SMP Communications
Susan Pietropaolo
M: 201-923-2049
[email protected]
SOURCE NeuroTrauma Sciences, LLC
高管变更
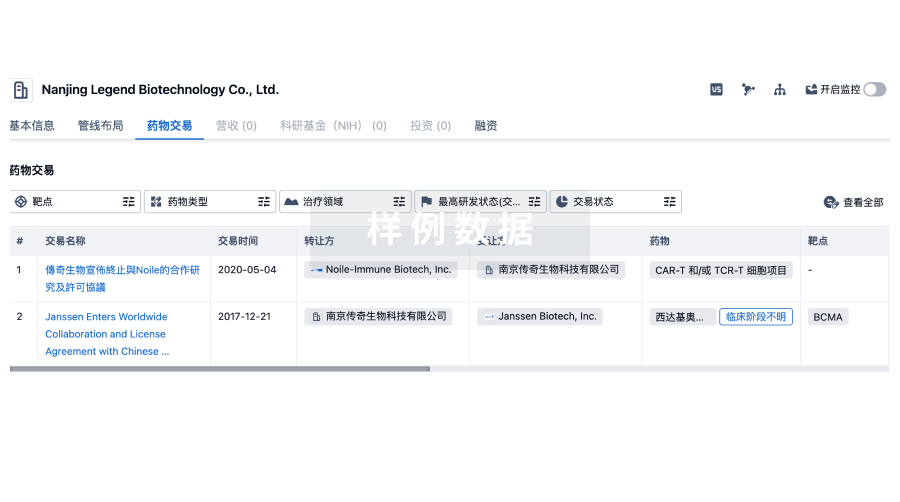
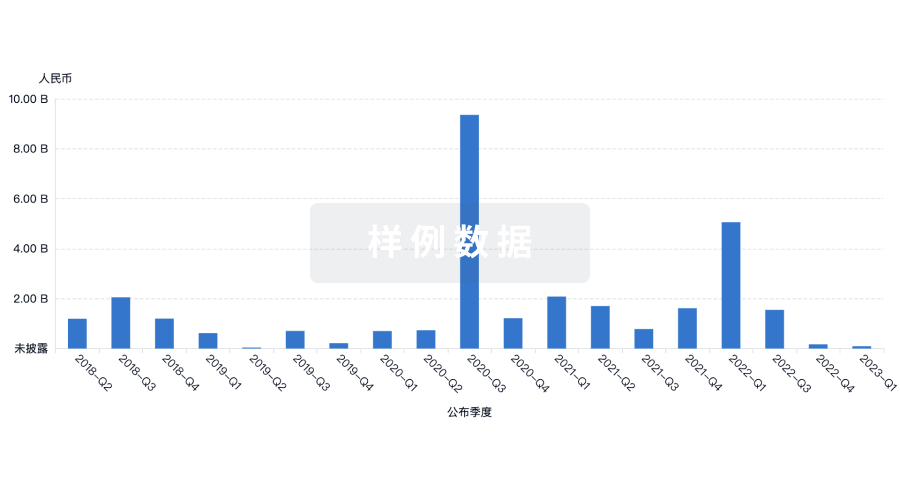
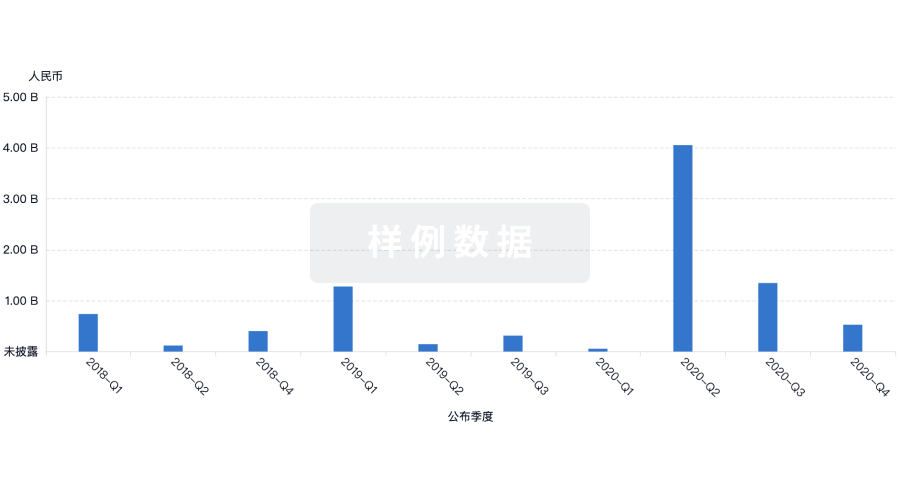
100 项与 NeuroTrauma Sciences LLC 相关的药物交易
登录后查看更多信息
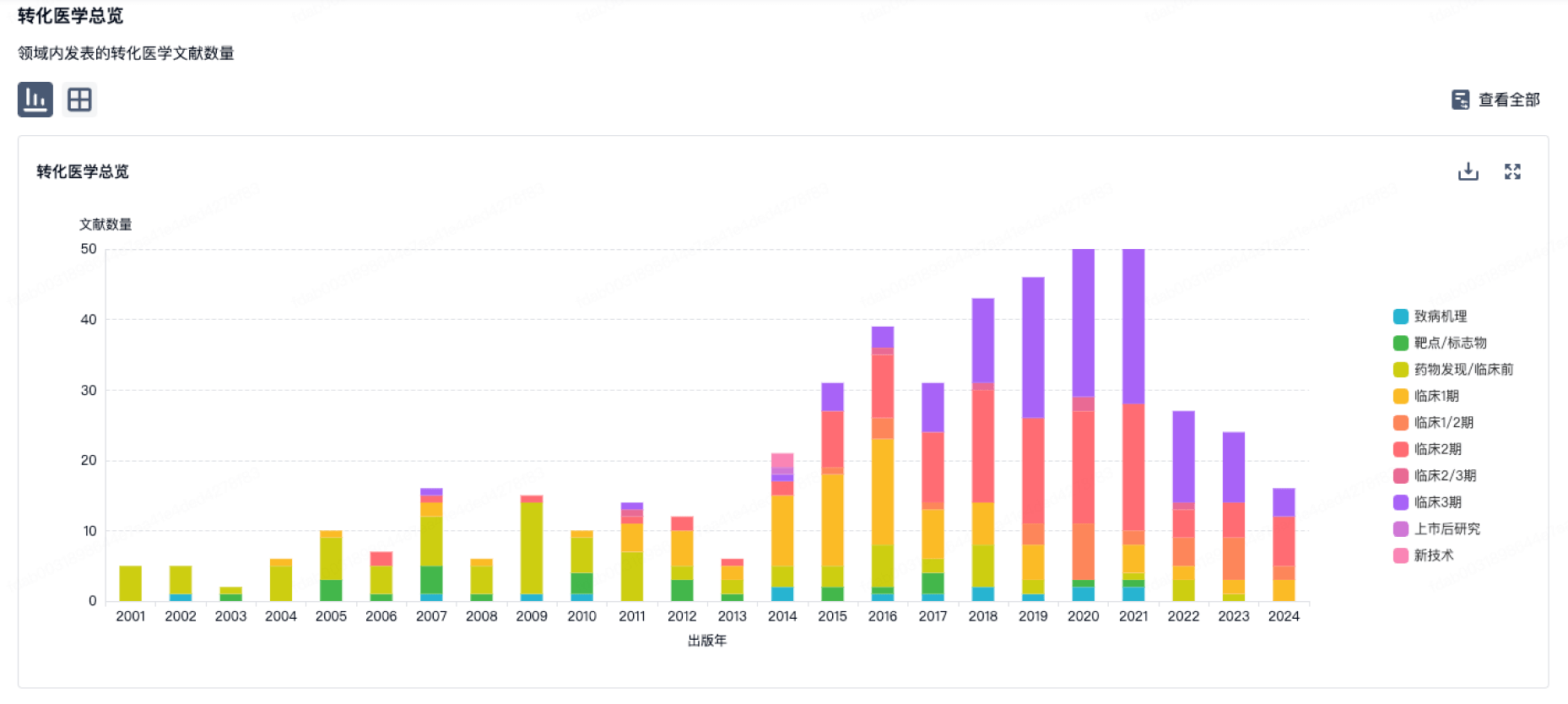
100 项与 NeuroTrauma Sciences LLC 相关的转化医学
登录后查看更多信息
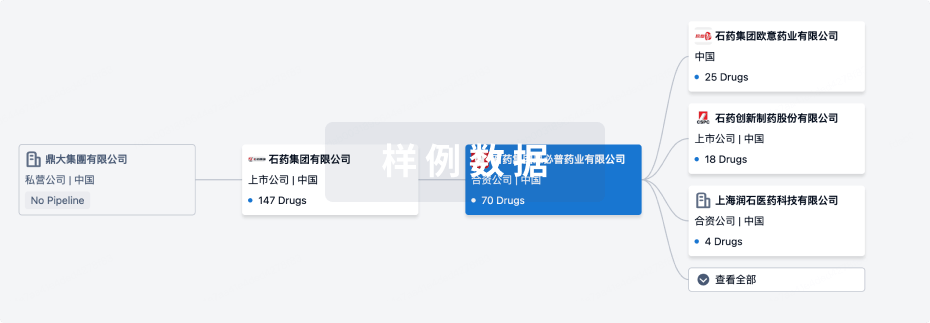
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2024年12月12日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
临床前
1
1
临床1期
其他
5
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
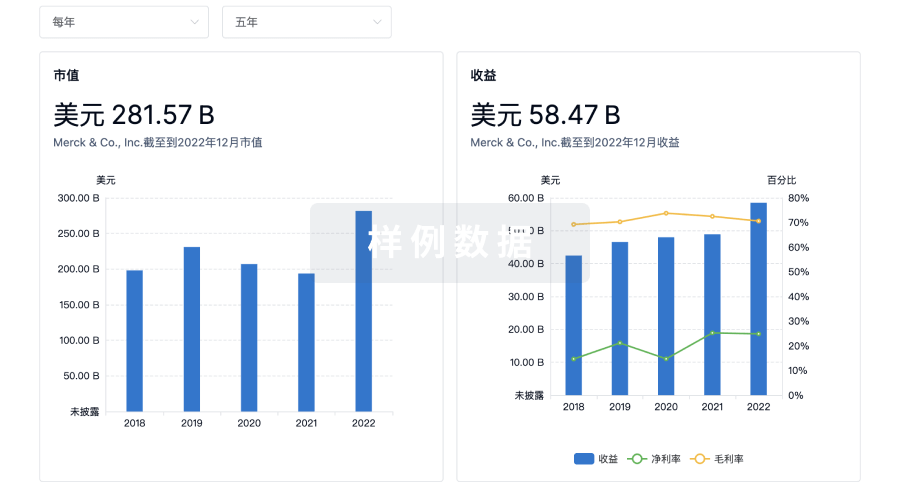
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
标准版
¥16800
元/账号/年
新药情报库 | 省钱又好用!
立即使用
来和芽仔聊天吧
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用

