预约演示
更新于:2025-08-29

Deutsches Herzzentrum Berlin
更新于:2025-08-29
概览
关联
173
项与 Deutsches Herzzentrum Berlin 相关的临床试验NCT06246188
Use of Stress-CMR Using Regadenoson and GE-267 in Adult Patients with Known or Suspected Coronary Artery Disease Using Mobile Cardiac MRI Units in a Single-arm Open-label Study
Stress cardiac MRI is crucial for diagnosing coronary artery disease in adults. Currently, it is mainly performed with vasodilators in specialized centers. Introducing mobile CMR units could increase accessibility, especially in rural areas, potentially reducing unnecessary invasive procedures. The objectives include demonstrating the feasibility of mobile stress perfusion CMR, detecting CAD using Regadenoson, and evaluating the image quality of GE-267 in real-world scenarios.
开始日期2025-06-01 |
申办/合作机构 |
DRKS00036011
Distress in Adults with Congenital Heart Disease: Screening, Protective and Risk Factors as well as Predictor for Outcome
开始日期2025-02-10 |
申办/合作机构 |
NCT06626672
Digital Lifestyle Intervention to Promote Physical Activity, Nutrition, and Health Literacy in Children With Congenital Heart Disease and Their Guardians
Congenital heart disease (CHD) affects approximately 1% of live births, and children with CHD often fail to meet WHO physical activity guidelines. Digital interventions to promote physical activity in CHD patients are limited. This study will develop and test a 12-week digital lifestyle intervention for children (ages 8-13) and their guardians, using a Garmin Vivofit Jr. 2 wearable to continuously monitor physical activity (PA). We will assess its impact on children's moderate to vigorous intensity physical activity (MVPA), daily activity (steps per day), quality of life, nutrition, and health literacy, as well as the quality of life and health literacy of their parents.
开始日期2024-10-01 |
申办/合作机构 |
100 项与 Deutsches Herzzentrum Berlin 相关的临床结果
登录后查看更多信息
0 项与 Deutsches Herzzentrum Berlin 相关的专利(医药)
登录后查看更多信息
612
项与 Deutsches Herzzentrum Berlin 相关的文献(医药)2025-07-31·European Heart Journal-Cardiovascular Imaging
Phenotypic clustering analysis of patients rejected for mitral valve interventions: implications for future transcatheter technologies
Article
作者: Garatti, Andrea ; Redwood, Simon ; Obadia, Jean-François ; Tchétché, Didier ; Adam, Matti ; Walther, Thomas ; Vincentelli, André ; Vogelhuber, Johanna ; Bleiziffer, Sabine ; Unbehaun, Axel ; Weber, Marcel ; Modine, Thomas ; Flagiello, Michele ; Ben Ali, Walid ; Schofer, Niklas ; Hamzi, Kenza ; Scotti, Andrea ; Maisano, Francesco ; Adamo, Marianna ; Longère, Benjamin ; Sudre, Arnaud ; Tanaka, Tetsu ; Muller, David W ; Makkar, Raj ; Granada, Juan F ; Pezel, Théo ; Schmidt, Tobias ; Metra, Marco ; Peterson, Mark ; Kaneko, Tsuyoshi ; Ludwig, Sebastian ; Shah, Pinak ; Rudolph, Tanja K ; Hausleiter, Jörg ; Petronio, Anna S ; Friedrichs, Kai ; Fam, Neil ; Da Rocha e Silva, Jaqueline ; Praz, Fabien ; Hungerford, Sara ; Leroux, Lionel ; Ochs, Laurin ; Sondergaard, Lars ; Lange, Rüdiger ; Regazzoli, Damiano ; Denti, Paolo ; Andreas, Martin ; von Bardeleben, Ralph Stephan ; Reardon, Michael J ; Conradi, Lenard ; Kleiman, Neil S ; Akodad, Mariama ; Rein, Kjell A ; Tang, Gilbert H L ; Hell, Michaela ; Blankenberg, Stefan ; Klein, Christoph ; Ruge, Hendrik ; Chehab, Omar ; Pozzoli, Alberto ; Blanke, Philipp ; Taramasso, Maurizio ; Koell, Benedikt ; Frerker, Christian ; Kalbacher, Daniel ; Kuhn, Elmar ; Dahle, Gry ; Goel, Sachin ; Dumonteil, Nicolas ; Coisne, Augustin ; Kempfert, Joerg ; Nickenig, Georg ; Kerbel, Tillmann ; Webb, John G ; Harloff, Morgan ; Latib, Azeem ; Duncan, Alison ; Wild, Mirjam ; Giannini, Cristina
Abstract:
Aims:
Although several treatment options are available for patients with severe mitral regurgitation (MR), a significant proportion of patients remain ineligible for any mitral valve (MV) intervention. We aimed to analyse the phenotypic characteristics of surgical high-risk patients ineligible for MV interventions using an unsupervised phenotypic clustering approach.
Methods and results:
Between 2014 and 2022, the CHOICE-MI registry included 984 patients with MR undergoing screening for transcatheter MV replacement at 33 international sites. For this study, only patients with screening failure receiving medical therapy alone were included. Patients receiving transcatheter or surgical treatment were excluded. A cluster analysis using K-means was performed on baseline clinical, demographic, and imaging variables to identify different patient phenotypes. Among 284 patients with MR (77.4 ± 8.82 years, 56.0% female, EuroSCORE II: 6.6 ± 5.8%) considered ineligible for any MV intervention, two clinically distinct phenogroups (PGs) were identified using unsupervised hierarchical clustering of principal components: PG1, elderly women with primary MR, preserved left ventricular function, and annular calcification; and PG2, patients with secondary MR, advanced heart failure, and high prevalence of comorbidities. One-year all-cause mortality did not differ between the PGs (PG1: 21.4%, PG2: 23.4%, P = 0.89). Predictors of mortality were albumin, renal function, and extracardiac arteriopathy for PG1 and albumin, coronary artery disease, and prior myocardial infarction for PG2.
Conclusion:
This study identified two major subgroups among patients ineligible for mitral interventions showing profound differences in clinical and anatomical profiles. Identifying these factors may drive technological evolution to address the unmet clinical need for therapeutic options in MR patients.
ClinicalTrials.gov identifier:
NCT04688190 (CHOICE-MI Registry)
2025-04-01·HEART RHYTHM
Association between surrogate insulin resistance markers and postablation atrial fibrillation recurrence: A systematic review and meta-analysis
Review
作者: Dagres, Nikolaos ; Mirjalili, Seyed Reza ; Soltani, Fatemeh ; Sepehri Shamloo, Alireza ; Ghoshouni, Hamed ; Hindricks, Gerhard ; Bakhshandeh, Hooman
Atrial fibrillation (AF) is the most common persistent arrhythmia and demonstrates a notable recurrence rate after ablation. Previous studies have suggested that surrogate markers of insulin resistance could predict postablation AF recurrence. This systematic review and meta-analysis aimed to assess studies examining the relationship between surrogate insulin resistance markers and the recurrence of AF after ablation. We searched PubMed, Web of Science, Embase, and Scopus for observational studies published from inception to August 2024. We incorporated studies that assessed the relationship between surrogate insulin resistance markers and the occurrence of postablation AF in patients with either paroxysmal or persistent AF. The random-effects model was used for meta-analysis. The Newcastle-Ottawa scale was used to evaluate risk of bias, and the leave-one-out method was applied for sensitivity analysis (PROSPERO: CRD42024584526). Nine studies involving 7729 participants met the inclusion criteria. Significant associations with AF recurrence were observed for the triglyceride-glucose index (hazard ratio [HR] 1.29; 95% confidence interval [CI] 1.15-1.44; I2 = 44%), homeostatic model assessment of insulin resistance (HR 1.27; 95% CI 1.14-1.42; I2 = 0%), and metabolic score for insulin resistance (HR 1.04; 95% CI 1.03-1.05; I2 = 0%). However, the triglyceride-to-high-density lipoprotein ratio did not demonstrate a statistically significant association with AF recurrence (HR 1.09; 95% CI 0.96-1.24; I2 = 86%). Surrogate markers of insulin resistance can be valuable predictors for assessing the risk of AF recurrence in patients who have undergone catheter ablation, potentially aiding in preventive strategies. Nevertheless, further prospective studies are required to validate our findings.
2025-03-28·EUROPACE
Epicardial ventricular arrhythmia ablation: a clinical consensus statement of the European Heart Rhythm Association of the European Society of Cardiology and the Heart Rhythm Society, the Asian Pacific Heart Rhythm Society, the Latin American Heart Rhythm Society, and the Canadian Heart Rhythm Society
Review
作者: Sepehri Shamloo, Alireza ; Zucchelli, Giulio ; Della Bella, Paolo ; Enriquez, Andres ; Hocini, Mélèze ; Sapp, John ; Deneke, Thomas ; Di Biase, Luigi ; Schmidt, Boris ; Wilde, Arthur ; Porta-Sanchez, Andreu ; Meyer, Christian ; Supple, Gregory E ; Arya, Arash ; de Chillou, Christian ; Pak, Hui-Nam ; Berruezo, Antonio ; Soejima, Kyoko ; Shivkumar, Kalyanam ; Bazán, Victor ; d'Avila, Andrea ; Zeppenfeld, Katja ; Kautzner, Josef ; Sommer, Philipp ; Stevenson, William G ; de Riva, Marta
Abstract:
Epicardial access during electrophysiology procedures offers valuable insights and therapeutic options for managing ventricular arrhythmias (VAs). The current clinical consensus statement on epicardial VA ablation aims to provide clinicians with a comprehensive understanding of this complex clinical scenario. It offers structured advice and a systematic approach to patient management. Specific sections are devoted to anatomical considerations, criteria for epicardial access and mapping evaluation, methods of epicardial access, management of complications, training, and institutional requirements for epicardial VA ablation. This consensus is a joint effort of collaborating cardiac electrophysiology societies, including the European Heart Rhythm Association, the Heart Rhythm Society, the Asia Pacific Heart Rhythm Society, the Latin American Heart Rhythm Society, and the Canadian Heart Rhythm Society.
100 项与 Deutsches Herzzentrum Berlin 相关的药物交易
登录后查看更多信息
100 项与 Deutsches Herzzentrum Berlin 相关的转化医学
登录后查看更多信息
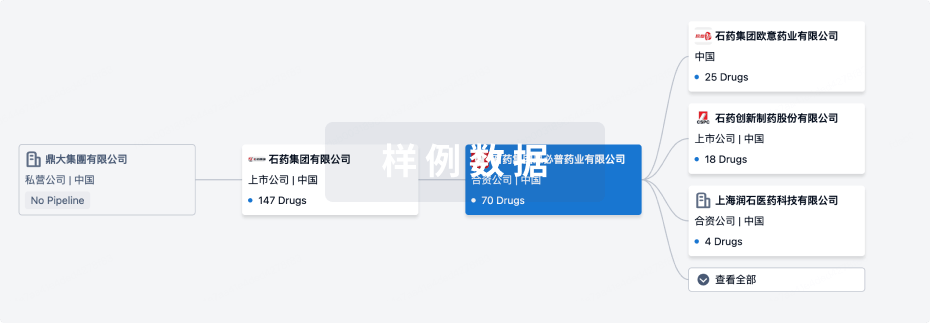
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年08月30日管线快照
无数据报导
登录后保持更新
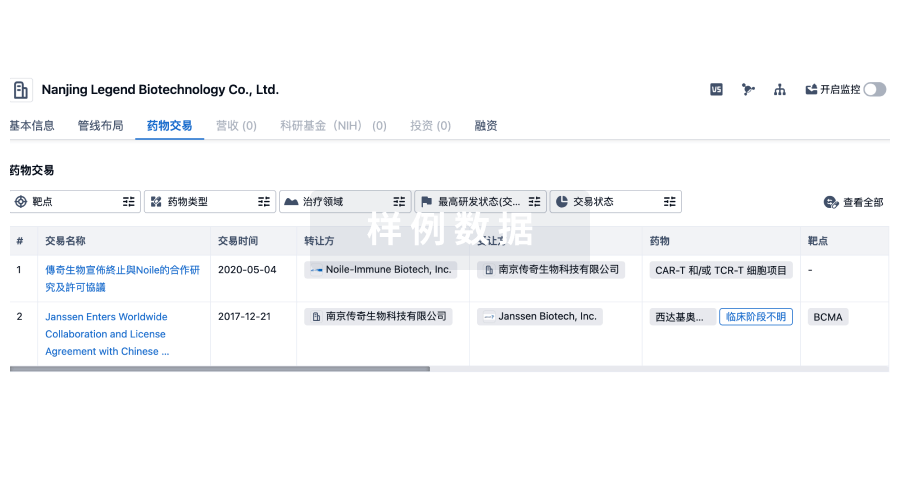
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
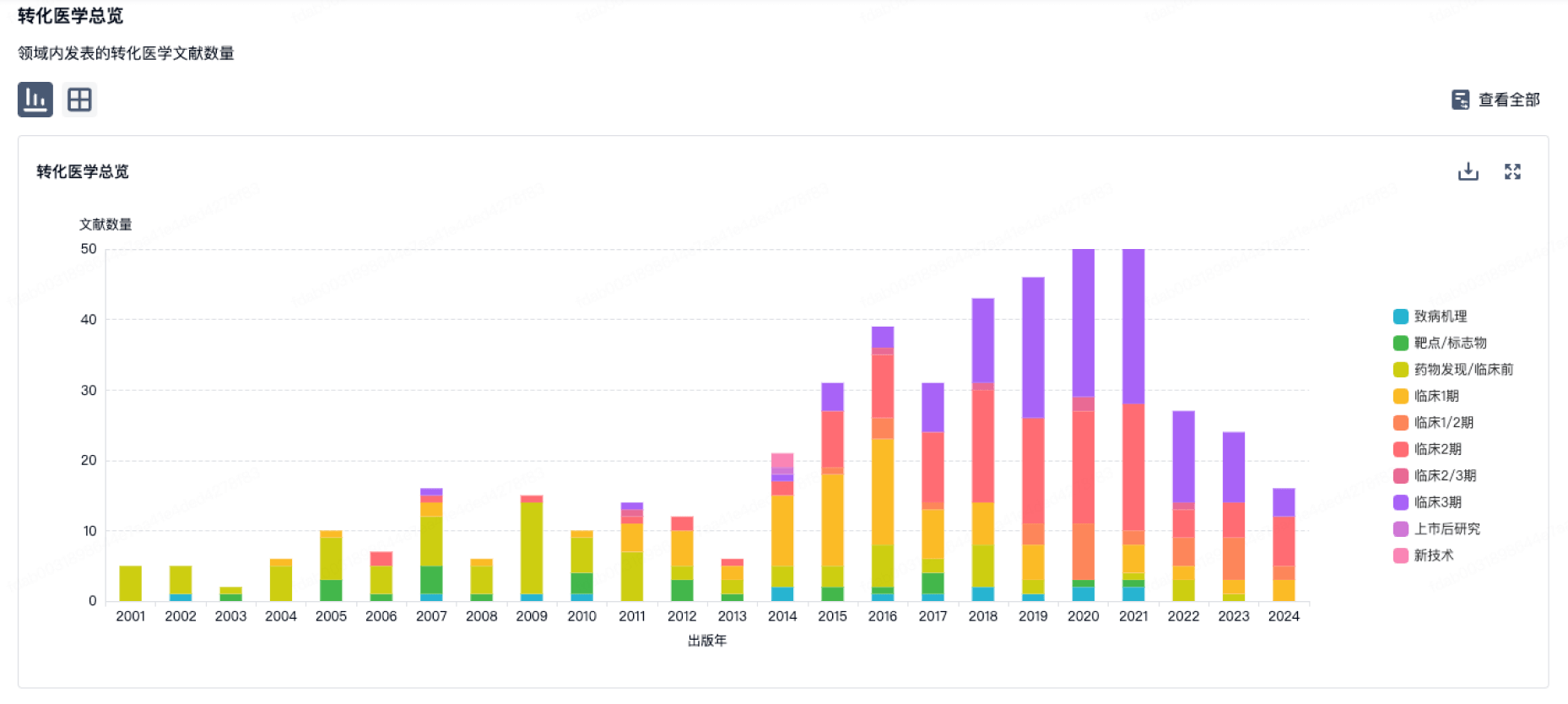
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
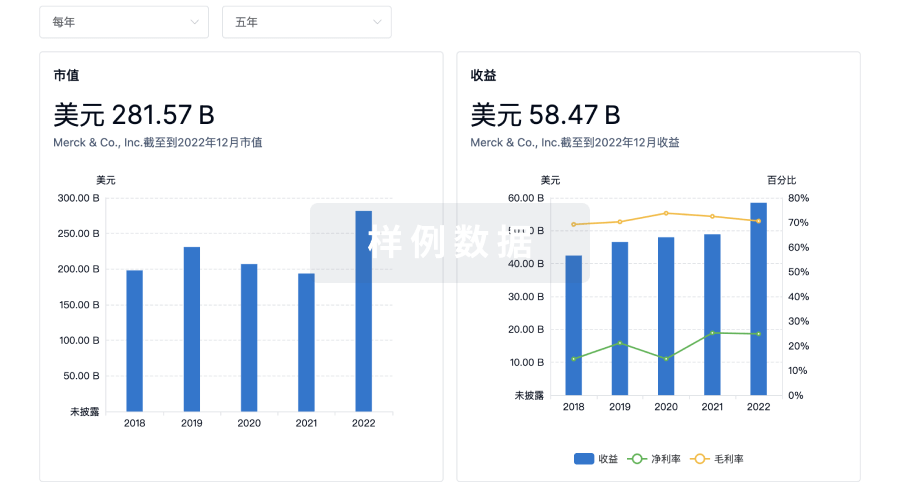
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

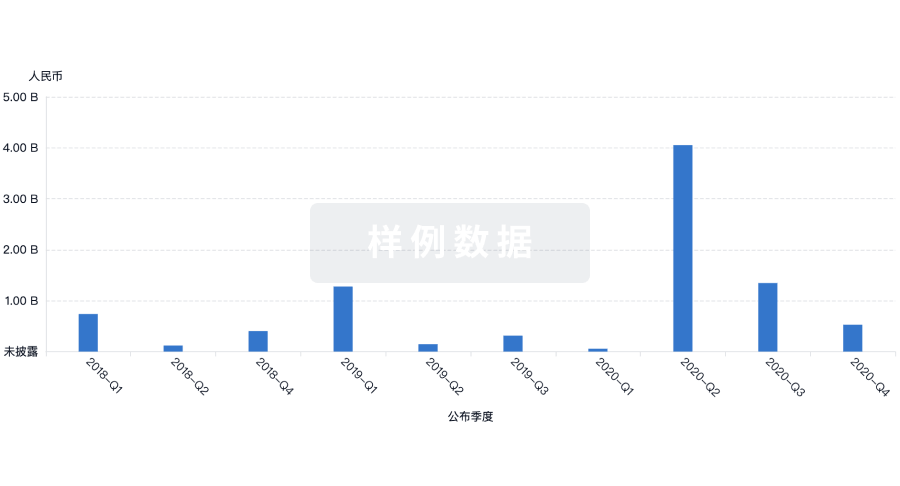
投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
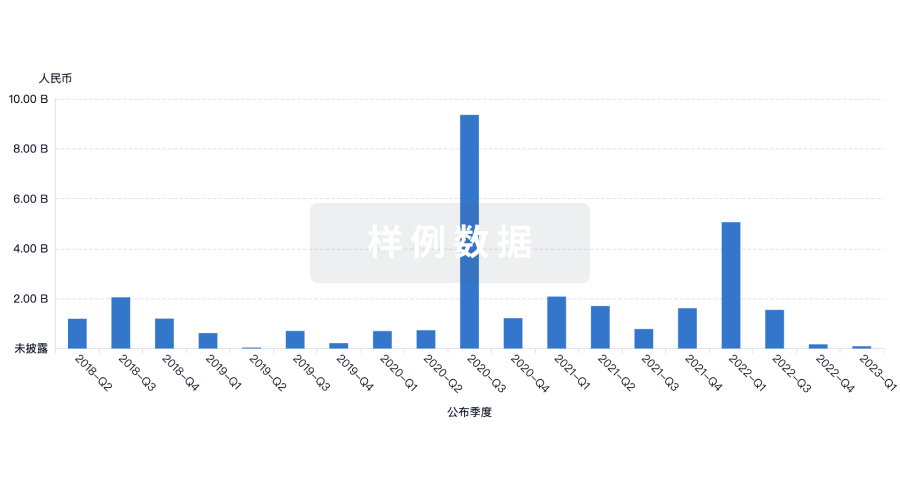
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用