更新于:2024-11-01
Institute of Regenerative and Cellular Medicine
更新于:2024-11-01
概览
关联
2
项与 Institute of Regenerative and Cellular Medicine 相关的临床试验Characterizing plasma metabolites/ lipids and gut microbiome profile as biomarkers of susceptibility to sarcopenia in the elderly
开始日期2022-12-12 |
Safety and Clinical Effectiveness of A3 SVF in Osteoarthritis
To purpose of this study is to determine if treatment with SVF (Stromal Vascular Fraction) has an effect on pain and inflammation associated with Osteoarthritis.
开始日期2012-09-01 |
100 项与 Institute of Regenerative and Cellular Medicine 相关的临床结果
登录后查看更多信息
0 项与 Institute of Regenerative and Cellular Medicine 相关的专利(医药)
登录后查看更多信息
5
项与 Institute of Regenerative and Cellular Medicine 相关的新闻(医药)2023-10-24
Eggs of the mosquito that carries Zika virus can tolerate extended desiccation by altering their metabolism, according to a new study. The finding offers potential new ways to control the spread of this mosquito.
Eggs of the mosquito that carries Zika virus can tolerate extended desiccation by altering their metabolism, according to a new study publishing October 24 in the open access journal PLOS Biology by Anjana Prasad, Sunil Laxman, and colleagues at the Institute for Stem Cell Science and Regenerative Medicine in Bengaluru, India and the Indian Institute of Technology in Mandi, India. The finding offers potential new ways to control the spread of this mosquito.
Cells are made mostly of water, and desiccation is a potentially fatal event for any organism, since the structures of many proteins and other cellular molecules are dependent on adequate hydration. While many types of microbes have evolved mechanisms to survive drying out, only a few animals have. Among them is the mosquito Aedes aegypti, the carrier of a variety of viral diseases, including, Zika, dengue, yellow fever, and Chikungunya. Originally found in North Africa, Ae. aegypti has expanded globally, and is now a threat in warm, moist regions throughout the world.
Aedes eggs require from 48 to 72 hours to hatch into larvae, and the authors first showed that eggs must be at least 15 hours old to survive desiccation; eggs that were dried out before this stage failed to hatch when rehydrated. They then compared the proteomes of viable eggs that had and had not been desiccated, and found multiple major changes in metabolic pathways within the desiccated eggs. These included increases in the levels of those enzymes in the tricarboxylic acid (Krebs) cycle that promote lipid metabolism, and a decrease in enzymes of glycolysis and ATP-producing parts of the TCA cycle, which together shunted cellular metabolism toward the production and use of fatty acids. Overall, the level of metabolism was reduced, while the levels of the amino acids arginine and glutamine were increased. In addition, enzymes that reduce the damaging effects of oxidative stress, a known consequence of dehydration, were also increased.
When linked together, arginine molecules form polyamines, which are known to help protect nucleic acids, proteins, and membranes from a variety of insults. Here, the authors showed that the eggs accumulate polyamines, suggesting that they may be a key aspect of desiccation tolerance. To test this, they fed egg-laying female mosquitoes an inhibitor of polyamine synthesis. The eggs that they laid were significantly less able to survive desiccation than eggs from untreated females. A second inhibitor, this one of fatty acid metabolism, also reduced egg viability after desiccation. Finally, they showed that this fatty acid inhibitor reduced polyamine synthesis, indicating that one role of the increase in fatty acid breakdown is to supply the energy needed for production of protective polyamines.
"Given the importance of Ae. aegypti as a primary vector for numerous viral diseases that affect nearly half the world's population," Laxman said, "as well as the rapid geographical expansion of this mosquito vector, these results provide a foundation for reducing Aedes egg survival and global spread. Additionally, some of the specific inhibitors described here that reduce desiccation resistance in Ae. aegypti eggs, as well as new ones affecting other steps in the egg desiccation tolerance pathway, may prove useful as vector-control agents."
Laxman adds, "Aedes mosquito eggs can indefinitely survive after drying up completely, and hatch into viable larvae. The embryos rewire their metabolism upon drying, to protect themselves through desiccation, and revive after water becomes available again."
临床结果
2023-08-14
Organoids have now been created from stem cells to secrete the proteins that form dental enamel, the substance that protects teeth from damage and decay. A multi-disciplinary team of scientists led this effort. This is a critical first step to the long-term goal to develop stem cell-based treatments to repair damaged teeth and regenerate those that are lost. Enamel is made during tooth formation by specialized cells called amelobasts. These cells die off after tooth formation is complete. Consequently, the body has no way to repair or regenerate damaged enamel.
Organoids have now been created from stem cells to secrete the proteins that form dental enamel, the substance that protects teeth from damage and decay. A multi-disciplinary team of scientists from the University of Washington in Seattle led this effort.
"This is a critical first step to our long-term goal to develop stem cell-based treatments to repair damaged teeth and regenerate those that are lost," said Hai Zhang, professor of restorative dentistry at the UW School of Dentistry and one of the co-authors of the paper describing the research.
The findings are published today in the journal Developmental Cell. Ammar Alghadeer, a graduate student in Hannele Ruohola-Baker's laboratory in the Department of Biochemistry at the UW School of Medicine was the lead author on the paper. The lab is affiliated with the UW Medicine Institute for Stem Cell and Regenerative Medicine.
The researchers explained that tooth enamel protects teeth from the mechanical stresses incurred by chewing and helps them resist decay. It is the hardest tissue in the human body.
Enamel is made during tooth formation by specialized cells called amelobasts. When tooth formation is complete, these cells die off. Consequently, the body has no way to repair or regenerate damaged enamel, and teeth can become prone to fractures or subject to loss.
To create ameloblasts in the laboratory, the researchers first had to understand the genetic program that drives fetal stem cells to develop into these highly specialized enamel-producing cells.
To do this they used a technique called single-cell combinatorial indexing RNA sequencing (sci-RNA-seq), which reveals which genes are active at different stages of a cell's development.
This is possible because RNA molecules, called messenger RNA (mRNA), carry the instructions for proteins encoded in the DNA of activated genes to the molecular machines that assemble proteins. That is why changes in the levels of mRNA at different stages of a cell's development reveal which genes are turned on and off at each stage.
By performing sci-RNA-seq on cells at different stages of human tooth development, the researchers were able to obtain a series of snapshots of gene activation at each stage. They then used a sophisticated computer program, called Monocle, to construct the likely trajectory of gene activities that occur as undifferentiated stem cells develop into fully differentiated ameloblast.
"The computer program predicts how you get from here to there, the roadmap, the blueprint needed to build ameloblasts," said Ruohola-Baker, who headed the project. She is a professor of biochemistry and associate director of the UW Medicine Institute for Stem Cell and Regenerative Medicine.
With this trajectory mapped out, the researchers, after much trial and error, were able to coax undifferentiated human stem cells into becoming ameloblasts. They did this by exposing the stem cells to chemical signals that were known to activate different genes in a sequence that mimicked the path revealed by the sci-RNA-seq data. In some cases, they used known chemical signals. In other cases, collaborators from the UW Medicine Institute for Protein Design created computer-designed proteins that had enhanced effects.
While conducting this project, the scientists also identified for the first time another cell type, called a subodontoblast, which they believe is a progenitor of odontoblasts, a cell type crucial for tooth formation.
The researchers found that together these cell types could be induced to form small, three-dimensional, multicellular mini-organs, called organoids. These organized themselves into structures similar to those seen in developing human teeth and secreted three essential enamel proteins: ameloblastin, amelogenin and enamelin. These proteins would then form a matrix. A mineralization process that is essential for forming enamel with the requisite hardness would follow.
Zhang said the research team now hopes to refine the process to make an enamel comparable in durability to that found in natural teeth and develop ways to use this enamel to restore damaged teeth. One approach would be to create enamel in the laboratory that could then be used to fill cavities and other defects.
Ruohola-Baker points out that another more ambitious approach would be to create "living fillings" that could grow into and repair cavities and other defects. Ultimately, the goal would be to create stem cell-derived teeth that could replace lost teeth entirely.
Ruohola-Baker said teeth are an ideal model to work on the development of other stem cell therapies.
"Many of the organs we would like to be able to replace, like human pancreas, kidney, and brain, are large and complex. Regenerating them safely from stem cells will take time," she said. "Teeth on the other hand are much smaller and less complex. They're perhaps the low-hanging fruit. It may take a while before we can regenerate them, but we can now see the steps we need to get there."
She predicts, "This may finally be the 'Century of Living Fillings' and human regenerative dentistry in general."
In addition to researchers from the Department of Oral Health Sciences in the UW School of Dentistry, other scientists from the UW Brotman Baty Institute, the UW Allen School of Computer Science and Engineering, Seattle Children's Research Institute, Institute for Stem Cell and Regenerative Medicine, Institute for Protein Design, the Department of Engineering in the UW College of Engineering Bioengineering (a joint department in UW's College of Engineering and School of Medicine), Biochemistry, Comparative Medicine and Pediatrics, Genome Sciences, all at the UW medical school, and the SRM Institute of Science and Technology, Chennai, India, all contributed to the study.
This work was supported by funding from the U.S. National Institutes of Health (1P01GM081619, R01GM097372, R01GM97372-03S1, R01GM083867, 5R24HD000836, T90DE021984, R01DE033016, U01DK127553, R01DK117914), the National Heart, Lung and Blood Institute Progenitor Cell Biology Consortium (U01HL099997; UO1HL099993), the Eunice Kennedy Shriver National Institute of Child Health and Human Development, UW Medicine Institute of Stem Cell and Regenerative Medicine Fellowships and the Dr. Douglass L. Morell Research Fund. Work conducted in the Institute for Stem Cell and Regenerative Medicine's Genomics Core was supported by a gift from the John H. Tietze Foundation
2023-05-31
MAUI, Hawaii--(
BUSINESS WIRE
)--Extended Longevity, a leading provider of innovative anti-aging solutions, is thrilled to announce the successful completion of the groundbreaking Longevinaut Study #1. The study, conducted under the guidance of Dr. Juergen Winkler at Quantum Functional Medicine, Carlsbad, CA, under the supervision of the Institute of Regenerative and Cellular Medicine, of Santa Monica, California, Executive Director Dr. Barbara Krutchkoff, PhD has demonstrated the safety and effectiveness of the Extended Longevity Protocol in reversing the epigenetic aging rate in a cohort of healthy individuals aged 55-75.
The results of this year-long clinical trial have exceeded expectations, providing hope for individuals seeking to improve their quality of life and reduce the risk of age-related diseases. The Extended Longevity Protocol, a set of 10 phytotherapeutic extract formulations targeting the 10 determinant factors of aging, has shown significant success in decelerating the biomarkers of aging across the cohort.
The study involved a rigorous methodology, with participants undergoing epigenome tests, telomere tests, and C-Reactive Protein (CRP) tests at baseline, 6 months, and 12 months. The study conducted by Dr. Winkler revealed astonishing outcomes. The epigenome aging biomarker was decelerated by an average of 13.16 years, or 22.5%, from baseline age, with some participants achieving age deceleration of up to 36.31%. Telomere length, a critical marker of cellular aging, exhibited an average reduction of 8.2% from chronological age, equivalent to a staggering 40-year age deceleration. Additionally, inflammation levels, as measured by the Hs C-RP test, decreased by an average of 55.4% in participants testing positive.
"The results of the Longevinaut Study #1 provide significant evidence of the effectiveness of the Extended Longevity Protocol in reversing the aging process," said Dr. Winkler. "These findings offer hope for individuals looking to enhance their overall health, well-being, and longevity."
Extended Longevity's commitment to providing evidence-based interventions using natural phytotherapeutic extract formulations has paved the way for a potential breakthrough in healthy aging. While further research is required to fully comprehend the benefits and potential risks, these findings indicate a promising approach for promoting longevity and improving the quality of life for aging individuals.
As the aging population continues to grow, the implications of slowing down the aging process and reducing the burden of age-related diseases are immense. Extended Longevity remains dedicated to advancing the field of anti-aging medicine and improving the overall health of individuals through continued research and development.
For more information on the Longevinaut Study #1 and the Extended Longevity Protocol, please visit
https://www.extendedlongevity.com/general-8
or contact our media relations team.
About Extended Longevity:
Extended Longevity is a leading provider of phytotherapeutic extract formulations designed to address the determinant factors of aging. Backed by proven clinical studies, our products offer a natural and evidence-based approach to promote healthy aging safely. With a commitment to research and innovation, Extended Longevity is dedicated to improving the quality of life for individuals seeking to reverse the aging process.
临床结果临床研究
100 项与 Institute of Regenerative and Cellular Medicine 相关的药物交易
登录后查看更多信息
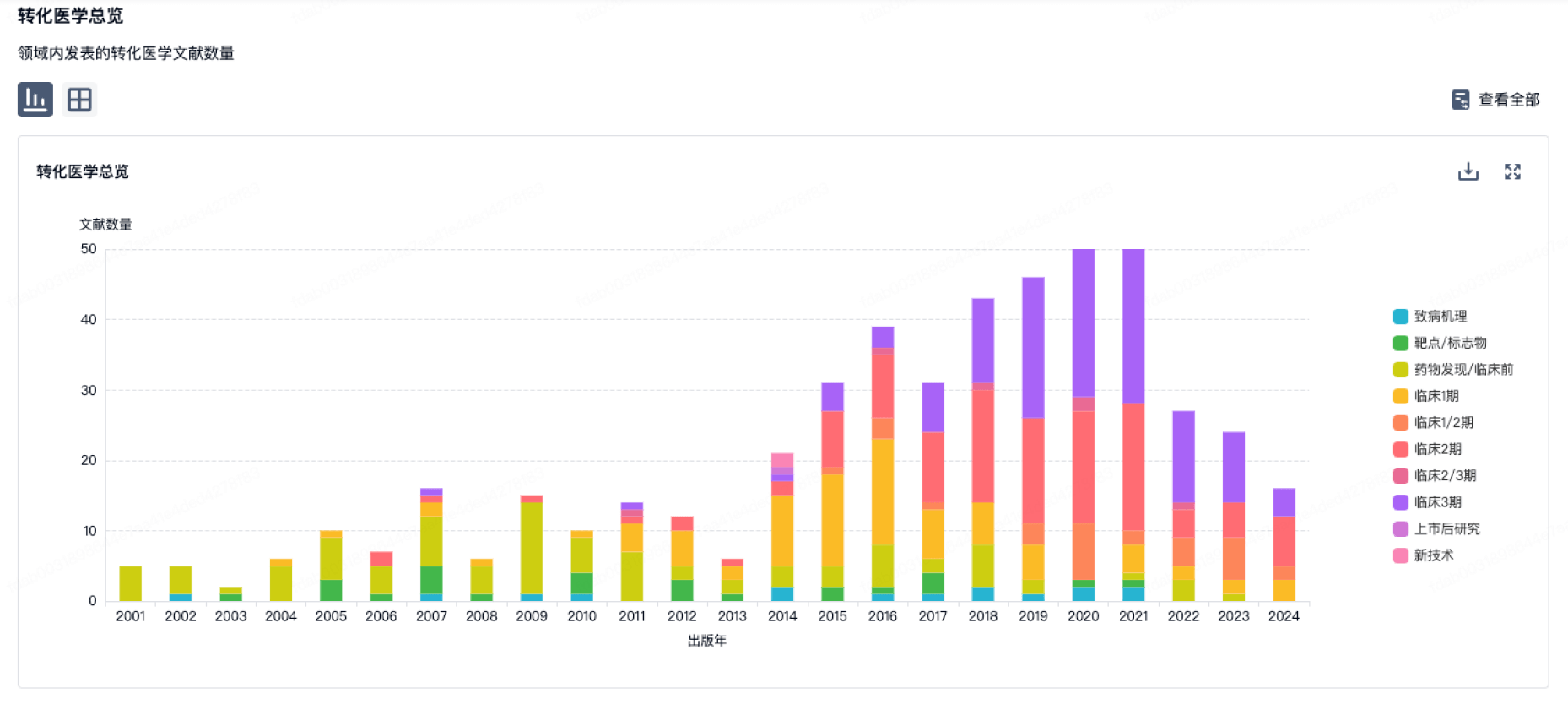
100 项与 Institute of Regenerative and Cellular Medicine 相关的转化医学
登录后查看更多信息
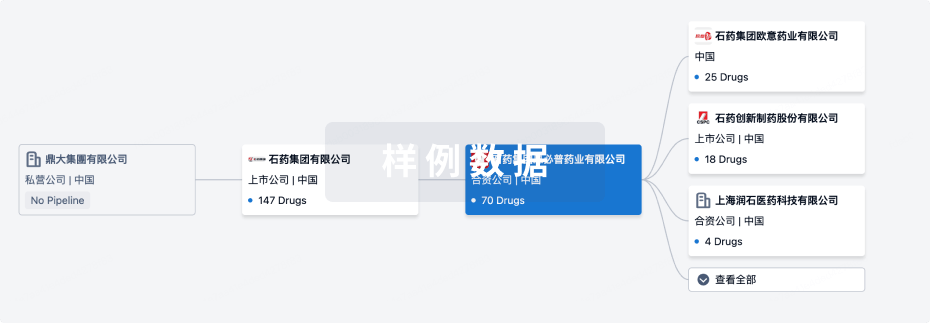
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2024年11月10日管线快照
无数据报导
登录后保持更新
药物交易
使用我们的药物交易数据加速您的研究。
登录
或

转化医学
使用我们的转化医学数据加速您的研究。
登录
或
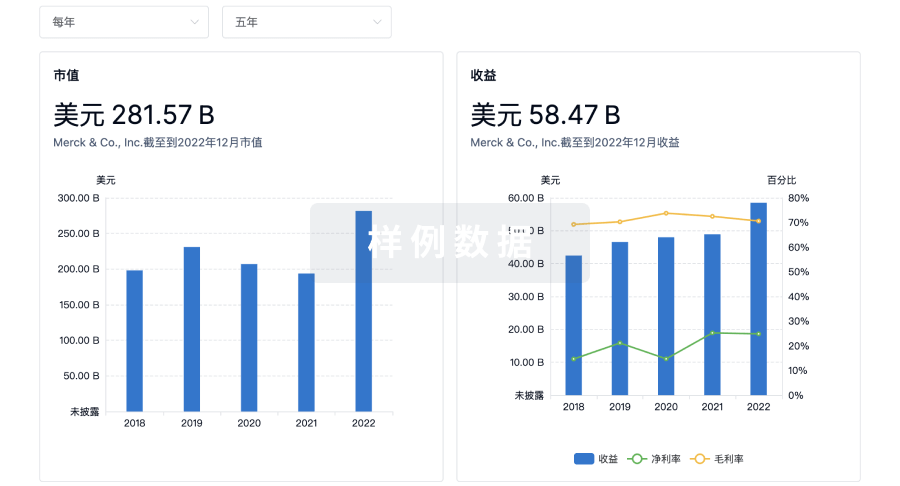
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或

融资
发掘融资趋势以验证和推进您的投资机会。
登录
或

标准版
¥16800
元/账号/年
新药情报库 | 省钱又好用!
立即使用
来和芽仔聊天吧
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用