预约演示
更新于:2025-05-07
Centro Nacional de Investigaciones Oncologicas
更新于:2025-05-07
概览
标签
其他疾病
免疫系统疾病
呼吸系统疾病
腺相关病毒基因治疗
小分子化药
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 小分子化药 | 1 |
| 腺相关病毒基因治疗 | 1 |
| 排名前五的靶点 | 数量 |
|---|---|
| PIM1(Pim-1 激酶) | 1 |
关联
5
项与 Centro Nacional de Investigaciones Oncologicas 相关的药物靶点- |
作用机制 基因转移 |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期- |
靶点 |
作用机制 PIM1抑制剂 |
非在研适应症- |
最高研发阶段药物发现 |
首次获批国家/地区- |
首次获批日期- |
作用机制 SIRT1抑制剂 [+1] |
在研机构- |
在研适应症- |
非在研适应症 |
最高研发阶段无进展 |
首次获批国家/地区- |
首次获批日期- |
100 项与 Centro Nacional de Investigaciones Oncologicas 相关的临床结果
登录后查看更多信息
0 项与 Centro Nacional de Investigaciones Oncologicas 相关的专利(医药)
登录后查看更多信息
3,042
项与 Centro Nacional de Investigaciones Oncologicas 相关的文献(医药)2025-12-31·OncoImmunology
Dual-targeted STAb-T cells secreting BCMA and CD19 T cell engagers for improved control of haematological cancers
Article
作者: Díez-Alonso, Laura ; Álvarez-Vallina, Luis ; Arroyo-Ródenas, Javier ; Velasco-Sidro, Miriam ; Ramírez-Fernández, Ángel
2025-07-01·Physiological Reviews
The influence of extracellular vesicles on tumor evolution and resistance to therapy
Review
作者: Bastón, Enrique ; García-Agulló, Juan ; Peinado, Héctor
2025-05-01·Clinical Cancer Research
Treatment Efficacy and Molecular Dynamics of Neoadjuvant Durvalumab and Olaparib in Resectable Urothelial Bladder Cancer: The NEODURVARIB Trial
作者: Gajate, Pablo ; Rodríguez-Moreno, Juan F. ; Ruiz-Llorente, Sergio ; Fernández, Ricardo ; Rodríguez-Antona, Cristina ; Virizuela, Juan A. ; Graña-Castro, Osvaldo ; Berraondo, Pedro ; Sevillano-Fernández, Elena ; Vázquez, Sergio ; Font, Albert ; García-Donas, Jesús ; de Velasco, Guillermo ; Álvarez-Fernández, Carlos ; Beltrán, Luis ; Lainez, Nuria ; Collado, Ricardo ; Madurga, Rodrigo
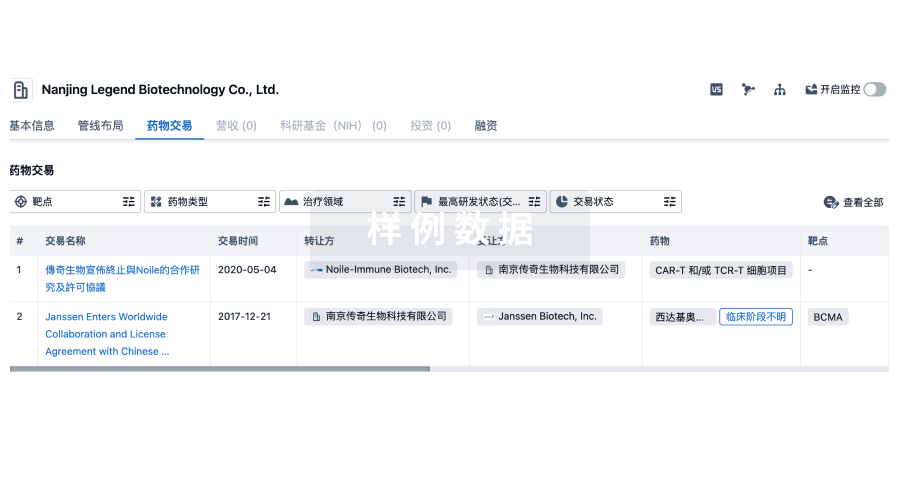
100 项与 Centro Nacional de Investigaciones Oncologicas 相关的药物交易
登录后查看更多信息
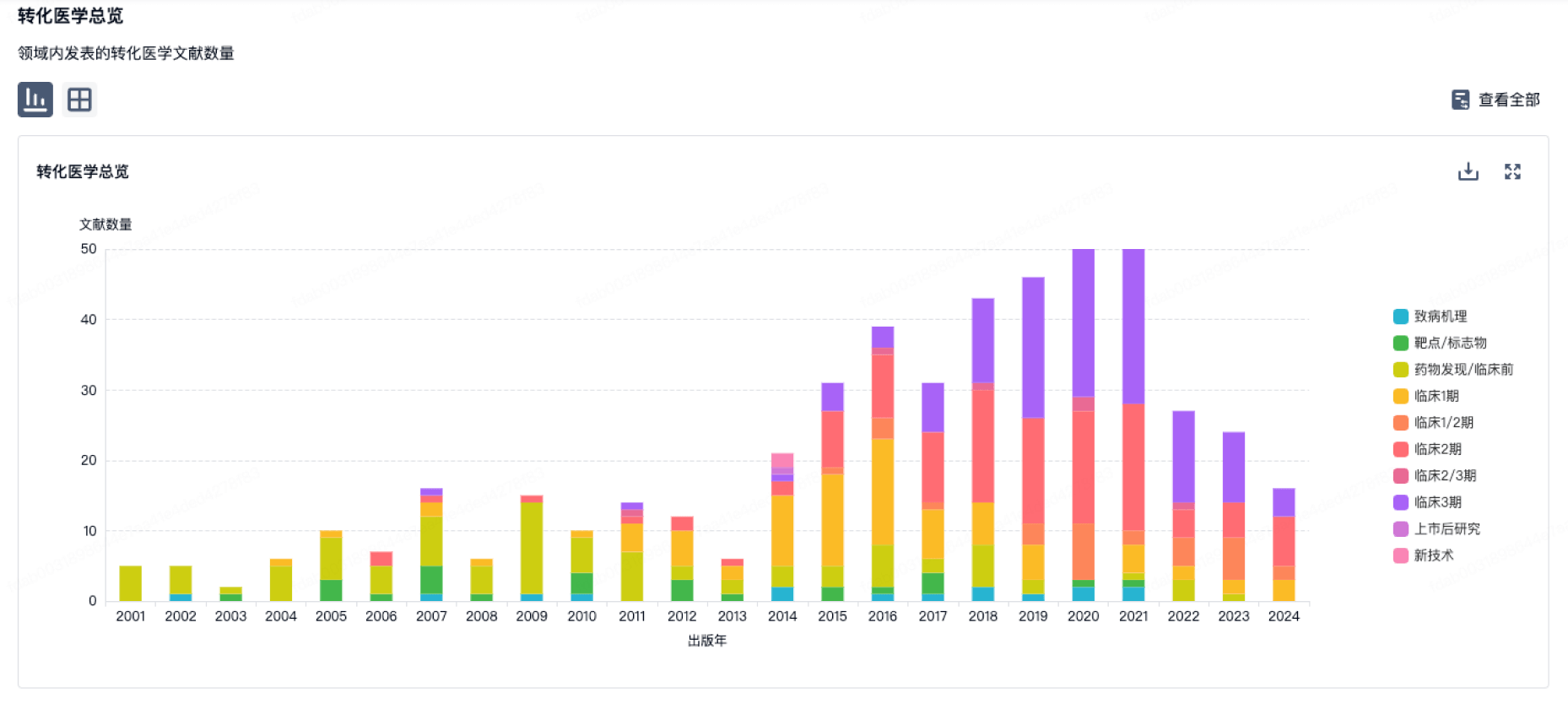
100 项与 Centro Nacional de Investigaciones Oncologicas 相关的转化医学
登录后查看更多信息
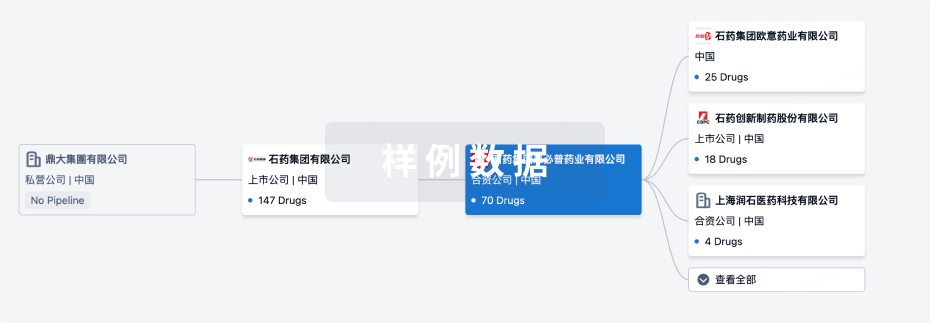
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年08月10日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
药物发现
1
1
临床前
其他
3
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
AAV9-tert gene therapy (CNIO/Universitat Autonoma de Barcelona/F Hoffmann-La Roche) | 心脏衰竭 更多 | 临床前 |
IBL-100 ( PIM1 ) | 炎症 更多 | 药物发现 |
ETP-46321 ( PI3Kα x PI3Kδ ) | 肿瘤 更多 | 无进展 |
Salermide ( SIRT1 x SIRT2 ) | 肿瘤 更多 | 无进展 |
ETP-46992 ( Class I PI3K ) | 肿瘤 更多 | 无进展 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
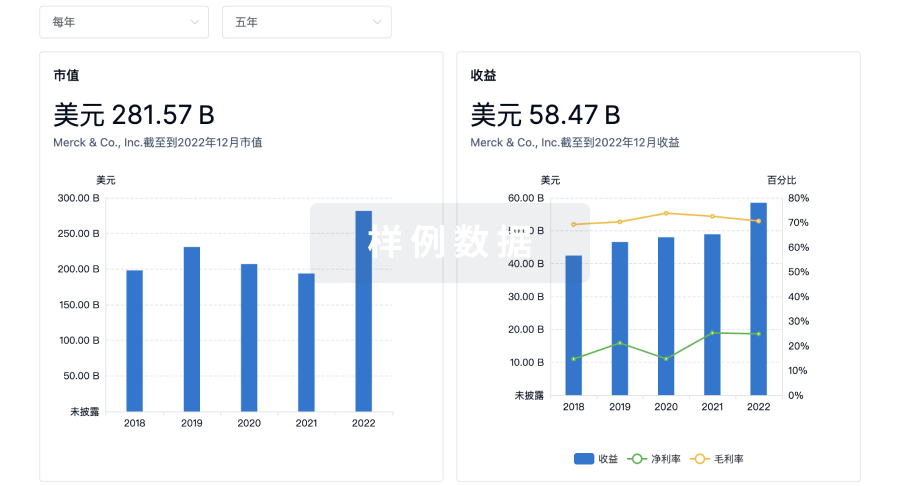
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用