预约演示
更新于:2025-08-09
Korea University Anam Hospital
更新于:2025-08-09
概览
标签
其他疾病
间充质干细胞疗法
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 间充质干细胞疗法 | 1 |
关联
1
项与 Korea University Anam Hospital 相关的药物靶点- |
作用机制- |
在研适应症 |
非在研适应症- |
最高研发阶段临床阶段不明 |
首次获批国家/地区- |
首次获批日期- |
301
项与 Korea University Anam Hospital 相关的临床试验NCT07091773
A Clinical Trial to Evaluate the Safety and Effectiveness of "OLIZ," a Combined Wavelength Photobiomodulation Medical Device, for Surgical Site Pain Relief in Patients Who Have Undergone Total Knee Arthroplasty (TKA) : A Multicenter, Controlled, and Randomized Clinical Trial
A Clinical Trial to Evaluate the Safety and Effectiveness of OLIZ, a Photobiomodulation Medical Device for Surgical Site Pain Relief in Patients After Total Knee Arthroplasty
开始日期2025-08-20 |
申办/合作机构 Ltbio Co. Ltd. [+5] |
NCT07017361
A Multicenter Randomized Prospective Study on Establishing an ERAS Program and Optimized Clinical Protocol for Patients Undergoing Minimally Invasive Pancreatoduodenectomy (MIPD)
To evaluate the impact of an Enhanced Recovery After Surgery (ERAS) program on postoperative recovery in patients undergoing minimally invasive pancreatoduodenectomy (MIPD)
开始日期2025-07-15 |
申办/合作机构 |
NCT06767345
Comparing the Moderate Intensity STatin With Ezetimibe COmbination TheraPy With High Intensity Statin Monotherapy on Coronary PLAQUE Stabilization
This study is a prospective, multicenter, randomized clinical trial aimed at comparing the effects of moderate-intensity statin plus ezetimibe combination therapy versus high-intensity statin monotherapy on coronary plaque stabilization. Using advanced imaging techniques such as near-infrared spectroscopy-intravascular ultrasound (NIRS-IVUS), the trial evaluates whether the combination therapy is non-inferior to monotherapy in stabilizing coronary plaques over 52 weeks. The primary endpoint is the percentage change in coronary atheroma volume (PAV), with secondary outcomes including changes in lipid core burden, inflammatory markers, and clinical events like myocardial infarction and ischemic stroke. The study plans to enroll 330 patients undergoing coronary intervention across 9 domestic institutions, with rigorous follow-up protocols and adherence to international research guidelines.
开始日期2025-05-12 |
申办/合作机构 |
100 项与 Korea University Anam Hospital 相关的临床结果
登录后查看更多信息
0 项与 Korea University Anam Hospital 相关的专利(医药)
登录后查看更多信息
1,776
项与 Korea University Anam Hospital 相关的文献(医药)2025-12-01·MEDICAL IMAGE ANALYSIS
Attend-and-Refine: Interactive keypoint estimation and quantitative cervical vertebrae analysis for bone age assessment
Article
作者: Kim, Taesung ; Kim, Yoon-Ji ; Song, In-Seok ; Kim, Jinhee ; Kim, Dong-Wook ; Choo, Jaegul ; Kim, Taewoo ; Ahn, Byungduk
In pediatric orthodontics, accurate estimation of growth potential is essential for developing effective treatment strategies. Our research aims to predict this potential by identifying the growth peak and analyzing cervical vertebra morphology solely through lateral cephalometric radiographs. We accomplish this by comprehensively analyzing cervical vertebral maturation (CVM) features from these radiographs. This methodology provides clinicians with a reliable and efficient tool to determine the optimal timings for orthodontic interventions, ultimately enhancing patient outcomes. A crucial aspect of this approach is the meticulous annotation of keypoints on the cervical vertebrae, a task often challenged by its labor-intensive nature. To mitigate this, we introduce Attend-and-Refine Network (ARNet), a user-interactive, deep learning-based model designed to streamline the annotation process. ARNet features Interaction-guided recalibration network, which adaptively recalibrates image features in response to user feedback, coupled with a morphology-aware loss function that preserves the structural consistency of keypoints. This novel approach substantially reduces manual effort in keypoint identification, thereby enhancing the efficiency and accuracy of the process. Extensively validated across various datasets, ARNet demonstrates remarkable performance and exhibits wide-ranging applicability in medical imaging. In conclusion, our research offers an effective AI-assisted diagnostic tool for assessing growth potential in pediatric orthodontics, marking a significant advancement in the field.
2025-09-01·COMPUTER METHODS AND PROGRAMS IN BIOMEDICINE
Temporal convolutional neural network-based feature extraction and asynchronous channel information fusion method for heart abnormality detection in phonocardiograms
Article
作者: Shin, Won-Jung ; Cha, Seul-Gi ; Seo, Woo-Young ; Kim, Dong-Kyu ; Shin, Keewon ; Kim, Sung-Hoon ; Park, Seongyong ; Moon, Baehun ; Shin, Jae-Man ; Kim, Hyun-Seok
BACKGROUND AND OBJECTIVE:
Auscultation-based cardiac abnormality detection is valuable screening approach in pediatric populations, particularly in resource-limited settings. However, its clinical utility is often limited by phonocardiogram (PCG) signal variability and a difficulty in distinguishing between pathological and innocent murmurs.
METHODS:
We proposed a framework that leverages temporal convolutional network (TCN)-based feature extraction and information fusion to integrate asynchronously acquired PCG recordings at the patient level. A probabilistic representation of the pathological state was first extracted from segmented PCG signals using a TCN-based model. These segment-level representations were subsequently averaged to generate record- or patient-level features. The framework was designed to accommodate recordings of varying durations and different auscultation locations. Furthermore, we addressed domain adaptation challenges in cardiac abnormality detection by incorporating transfer learning techniques.
RESULTS:
The proposed method was evaluated using two large, independent public PCG datasets, demonstrating robust performance at both record and patient levels. While its initial performance on an unseen external dataset was modest, likely due to demographic characteristics and signal acquisition, transfer learning significantly improved the model's performance, yielding an area under the receiver operating characteristic curve of 0.931±0.027 and an area under the precision-recall curve of 0.867±0.064 in external validation. Combining internal and external datasets further enhanced model generalizability.
CONCLUSION:
This proposed framework accommodates multi-channel, variable-length PCG recordings, making it a flexible and accurate solution for detecting pediatric cardiac abnormalities, particularly in low-resource settings. The source code is publicly available on Github (https://github.com/baporlab/pcg_pathological_murmur_detection).
2025-08-01·PEDIATRIC INFECTIOUS DISEASE JOURNAL
Disease Burden of Respiratory Syncytial Virus in Korean Children: A Nationwide Cohort Study
Article
作者: Choe, Young June ; Bertizzolo, Lorenzo ; Lee, Jue Seong ; Yoo, Young ; Choi, Sujin ; Kim, Hyun Jung ; Lee, Young Hwa
Background::
Respiratory syncytial virus (RSV) is a leading cause of lower respiratory tract infections in young children globally. This study aimed to characterize the epidemiology, clinical burden, and risk factors associated with RSV infection in South Korean children under 5 years of age.
Methods::
This nationwide, population-based retrospective cohort study utilized national health insurance claims data from 2007 to 2019. RSV cases were identified using relevant International Classification of Diseases, 10th Revision codes, and incidence, hospitalization, and outpatient visit rates were calculated. Logistic regression analysis identified risk factors for hospitalization.
Results::
A total of 185,823 RSV cases were identified, with an annual incidence of 286.0 to 822.9 per 100,000 children under 5. Hospitalization was required for 44.7% of cases. Infants under 6 months had the highest risk of hospitalization, longer hospital stays and higher medical costs. Logistic regression identified younger age, comorbidities and metropolitan residence as independent risk factors for hospitalization. Infants 6–11 months of age constituted the largest proportions of inpatient (48.2%) and outpatient (33.6%) cases, and highest number of intensive care unit admission.
Conclusion::
RSV infection places a substantial burden on young children in South Korea, particularly infants. High hospitalization rates underscore the need for targeted public health preventive interventions, enhanced surveillance and improved access to timely medical care, to mitigate RSV’s impact and improve child health outcomes.
24
项与 Korea University Anam Hospital 相关的新闻(医药)2025-07-28
Hazard Ratios and Improvements in Median PFS are Unprecedented in HR+/HER2- Advanced Breast Cancer (“ABC”)
MINNEAPOLIS, MN, USA I July 28, 2025 I
Celcuity Inc. (Nasdaq: CELC), a clinical-stage biotechnology company pursuing development of targeted therapies for oncology, today announced positive topline results from the
PIK3CA
wild-type cohort of the Phase 3 VIKTORIA-1 clinical trial evaluating gedatolisib plus fulvestrant with and without palbociclib versus fulvestrant in adults with hormone receptor (HR)-positive, human epidermal growth factor receptor 2 (HER2)-negative,
PIK3CA
wild-type, locally advanced or metastatic breast cancer, following progression on, or after, treatment with a CDK4/6 inhibitor and an aromatase inhibitor.
In the trial, the gedatolisib triplet demonstrated a statistically significant and clinically meaningful improvement in PFS among patients, reducing the risk of disease progression or death by 76% compared to fulvestrant (based on a hazard ratio [HR] of 0.24, 95% confidence interval [CI] 0.17-0.35; p<0.0001). The mPFS, as assessed by blinded independent central review (“BICR”), was 9.3 months with the gedatolisib triplet versus 2.0 months with fulvestrant, an incremental improvement of 7.3 months.
The gedatolisib doublet also demonstrated a statistically significant and clinically meaningful improvement in PFS among patients, reducing the risk of disease progression or death by 67% compared to fulvestrant (HR of 0.33, 95% CI 0.24-0.48; p<0.0001). The mPFS, as assessed by BICR, was 7.4 months with the gedatolisib doublet versus 2.0 months with fulvestrant, an incremental improvement of 5.4 months.
The topline efficacy data from the VIKTORIA-1
PIK3CA
wild-type cohort established several new milestones in the history of drug development for HR+/HER2- advanced breast cancer:
Sara Hurvitz, MD, Senior Vice President, Clinical Research Division, Fred Hutchinson Cancer Center, Professor and Head, Division of Hematology and Oncology, University of Washington, Department of Medicine and co-principal investigator for the trial said: “Patients with HR-positive, HER2-negative,
PIK3CA
wild-type advanced breast cancer whose disease has progressed while on, or after, treatment with a CDK4/6 inhibitor typically derive limited benefit from subsequent endocrine-based therapy. The topline data for both gedatolisib regimens from VIKTORIA-1 are potentially practice-changing. To my knowledge, we have not seen Phase 3 results in patients with HR-positive, HER2-negative advanced breast cancer before where there was a quadrupling of the likelihood of survival without disease progression relative to the study control.”
Treatment discontinuation due to a treatment-related adverse event for the gedatolisib triplet and gedatolisib doublet was lower than was observed in Arm D of the Phase 1b trial in patients with ABC, and lower than observed in any Phase 3 trials for currently approved drug combinations in HR+/HER2- ABC. Additionally, the gedatolisib triplet and gedatolisib doublet were better tolerated than was observed in the Phase 1b trial in patients with ABC, including lower rates of hyperglycemia and stomatitis.
Igor Gorbatchevsky, MD, Chief Medical Officer of Celcuity said: “The topline data from VIKTORIA-1 demonstrate the potential for gedatolisib to become a transformative new medicine for the treatment of patients with HR-positive, HER2-negative,
PIK3CA
wild-type advanced breast cancer whose disease progressed on or after treatment with CDK4/6 inhibitors. The 7.3 and 5.4-months incremental improvement in median PFS relative to fulvestrant for the gedatolisib regimens are potentially paradigm shifting results. We are also very excited that treatment with gedatolisib combined with fulvestrant with or without palbociclib was well-tolerated by the VIKTORIA-1 patients and that only a few patients discontinued treatment due to an adverse event.”
Brian Sullivan, Chairman, Chief Executive Officer and co-founder of Celcuity said, “The efficacy improvement relative to the control that each of the gedatolisib regimens demonstrated was historic for this patient population. We are excited about the potential opportunity to provide a breakthrough therapeutic option for patients with HR-positive, HER2-negative,
PIK3CA
wild-type advanced breast cancer.”
Full data from the
PIK3CA
wild-type cohort of the VIKTORIA-1 clinical trial will be presented at an upcoming medical conference later this year. Celcuity expects to submit a New Drug Application for gedatolisib to the U.S. Food and Drug Administration in the fourth quarter of 2025. Topline data for the VIKTORIA-1
PIK3CA
mutation cohort is expected by the end of 2025.
Webcast and Conference Call Information
The Celcuity management team will host a webcast/conference call on Monday, July 28, 2025, at 8:00 a.m. ET to discuss the topline results from the Phase 3 VIKTORIA-1 trial. Those who would like to participate may access the live webcast
here
, or register in advance for the teleconference
here
. A replay of the webcast will be available on the Celcuity website following the live event.
Notes
HR+/HER2- Breast cancer
Breast cancer is the second most common cancer and one of the leading causes of cancer-related deaths worldwide.
1
More than two million breast cancer cases were diagnosed globally in 2022.
1
While survival rates are high for those diagnosed with early breast cancer, only approximately 30% of patients who are diagnosed with or who progress to metastatic disease are expected to live five years after their diagnosis.
2
HR+/HER2- breast cancer is the most common subtype of breast cancer, accounting for approximately 70% of all breast cancers.
2
Three interconnected signaling pathways, estrogen, cyclin D1-CDK4/6, and PI3K/AKT/mTOR (PAM), are primary oncogenic drivers of HR+, HER2- breast cancer.
3
Therapies inhibiting these pathways are approved and used in various combinations for advanced breast cancer. Currently approved inhibitors of the PAM pathway for breast cancer target a single PAM pathway component, such as PI3Kα, AKT, or mTORC1.
4,5,6,7
However, resistance to CDK4/6 inhibitors and current endocrine therapies develops in many patients with advanced disease.
8
Survival rates are low with 30% of patients anticipated to live beyond five years after diagnosis.
2
Optimizing the inhibition of the PAM pathway is an active area of focus for breast cancer research.
VIKTORIA-1
VIKTORIA-1 is a Phase 3 open-label, randomized clinical trial to evaluate the efficacy and safety of gedatolisib in combination with fulvestrant with or without palbociclib in adults with HR+/HER2- ABC whose disease progressed on or after prior CDK4/6 therapy in combination with an aromatase inhibitor. The clinical trial is enrolling subjects regardless of
PIK3CA
status while enabling separate evaluation of subjects according to their
PIK3CA
status. Subjects who meet eligibility criteria and do not have confirmed
PI3KCA
mutations (WT) were randomly assigned (1:1:1) to receive a regimen of either gedatolisib, palbociclib, and fulvestrant, gedatolisib and fulvestrant, or fulvestrant. Subjects who meet eligibility criteria and have confirmed
PI3KCA
mutations (MT) are randomly assigned (3:3:1) to receive a regimen of either the gedatolisib triplet, alpelisib and fulvestrant, or the gedatolisib doublet.
Gedatolisib
Gedatolisib is an investigational, multi-target PAM inhibitor that potently targets all four class I PI3K isoforms, mTORC1, and mTORC2 to induce comprehensive blockade of the PAM pathway.
9,10,11
As a multi-target PAM inhibitor, gedatolisib’s mechanism of action is highly differentiated from currently approved single-target inhibitors of the PAM pathway.
11
Inhibition of only a single PAM component gives tumors an escape mechanism through cross-activation of the uninhibited targets. Gedatolisib’s comprehensive PAM pathway inhibition ensures full suppression of PAM activity by eliminating adaptive resistance cross-activation that occurs with single-target inhibitors. Unlike single-target inhibitors of the PAM pathway, gedatolisib has demonstrated equal potency and comparable cytotoxicity in
PIK3CA
-mutant and -wild-type breast tumor cells in nonclinical studies and early clinical data.
11,12
About Celcuity
Celcuity is a clinical-stage biotechnology company pursuing development of targeted therapies for treatment of multiple solid tumor indications. The company’s lead therapeutic candidate is gedatolisib, a potent, pan-PI3K and mTORC1/2 inhibitor that comprehensively blockades the PAM pathway. Its mechanism of action and pharmacokinetic properties are differentiated from other currently approved and investigational therapies that target PI3Kα, AKT, or mTORC1 alone or together. A Phase 3 clinical trial, VIKTORIA-1, evaluating gedatolisib in combination with fulvestrant with or without palbociclib in patients with HR+/HER2- advanced breast cancer is currently enrolling patients. A Phase 1/2 clinical trial, CELC-G-201, evaluating gedatolisib in combination with darolutamide in patients with metastatic castration resistant prostate cancer, is ongoing. A Phase 3 clinical trial, VIKTORIA-2, evaluating gedatolisib plus a CDK4/6 inhibitor and fulvestrant as first-line treatment for patients with HR+/HER2- advanced breast cancer is currently enrolling patients. More detailed information about Celcuity’s active clinical trials can be found at
ClinicalTrials.gov
. Celcuity is headquartered in Minneapolis. Further information about Celcuity can be found at
www.celcuity.com
. Follow us on
LinkedIn
and
X
.
SOURCE:
Celcuity
临床3期临床结果临床1期临床2期
2025-07-02
·药事纵横
自安进公司斥资近20亿美元收购Five Prime公司及其针对FGFR2b的单克隆抗体(mAb)以来,已过去四年多。如今,贝马妥珠单抗(bemarituzumab)的新数据证明了安进公司这一决策的正确性。6月30日,安进公司公布了一项胃癌III期临床试验的主要结果,显示该单克隆抗体达到了主要生存终点。尽管这家制药公司未透露此次临床试验成功的具体细节,但承诺会在未来的医学会议上提供详细数据。这项名为FORTITUDE-101的III期临床试验共招募了547名患有不可切除、局部晚期或转移性非HER2阳性、FGFR2b过表达的胃癌或胃食管交界处(GEJ)癌的患者。参与者被随机分组,一组接受一线贝马妥珠单抗联合化疗(mFOLFOX6方案)治疗,另一组仅接受化疗。根据预先设定的中期分析结果,联合治疗组在总生存期(OS)方面相比单纯化疗组,取得了具有统计学意义和临床意义的显著改善,达到了试验的主要终点。安进公司负责研发的执行副总裁杰伊·布拉德纳(Jay Bradner)表示:“大多数胃癌患者在确诊时已处于晚期,预后较差,生存率低,且治疗选择有限。”他补充道,此次研究结果“标志着在开发有效胃癌靶向治疗药物方面取得了具有重大意义的进展”。此次结果也印证了II期临床试验的发现。在II期试验中,贝马妥珠单抗联合化疗相较于单纯化疗,显著延长了患者的无进展生存期和总生存期。II期试验也显示,接受贝马妥珠单抗治疗的患者角膜和口腔炎等不良事件(AEs)的发生率更高。实验药物组中至少出现3级不良事件的患者比例达82.9%,而安慰剂组为74%。此外,34.2%接受贝马妥珠单抗治疗的患者因不良事件而中断治疗,而安慰剂组仅为5.2%。在III期试验中,贝马妥珠单抗组眼部不良事件的发生“频率更高,严重程度也更高”。超过四分之一接受该单克隆抗体治疗的患者出现了视力下降、点状角膜炎、贫血、中性粒细胞减少、恶心、角膜上皮缺损或干眼等症状。FORTITUDE-101试验得到了再鼎医药的支持。2017年,再鼎医药从Five Prime公司独家获得了贝马妥珠单抗在中国大陆、香港、澳门和台湾地区的共同开发与商业化权利。此外,双方合作伙伴还在开展一项贝马妥珠单抗联合化疗及百时美施贵宝公司的纳武利尤单抗(Opdivo,商品名)作为胃癌一线治疗的III期试验,预计今年下半年公布数据。药事纵横投稿须知:稿费已上调,欢迎投稿
临床3期临床2期并购临床成功临床结果
2025-06-15
编者按:三阴性乳腺癌(TNBC)是当前预后最差的乳腺癌亚型之一。随着近年来诊疗技术的发展,免疫治疗、抗体偶联药物(ADC)为TNBC带来了新的选择,其中靶向Trop-2 的ADC戈沙妥珠单抗(SG)已成为TNBC二线治疗的标准方案[1]。2025年美国临床肿瘤学会(ASCO)年会上,戈沙妥珠单抗联合帕博利珠单抗一线治疗PD-L1阳性TNBC的III期ASCENT-04/KEYNOTE-D19研究作为LBA,重磅披露了阳性结果,显示较标准的化疗联合免疫方案降低了35%的疾病进展或死亡风险,安全可控,奠定了ADC+免疫治疗一线应用于TNBC的基础[2]。因此,《肿瘤瞭望》于ASCO会议现场邀请江苏省人民医院殷咏梅教授与广东省人民医院王坤教授展开对话,分享对ASCENT-04研究结果的评价,展望未来TNBC一线治疗格局的发展前景。01肿瘤瞭望:此次ASCO大会公布了ASCENT-04研究的初步结果,显示了Trop-2 ADC戈沙妥珠单抗联合帕博利珠单抗一线治疗晚期TNBC的优势。首先,请您分享一下该研究的设计及主要结果。殷咏梅教授江苏省人民医院ASCENT-04研究[2]是一项全球性、多中心、开放标签、随机Ⅲ期临床研究,主要针对既往未经晚期系统治疗、无法手术的PD-L1阳性(CPS≥10)局部晚期或转移性三阴性乳腺癌 (TNBC)患者,评估戈沙妥珠单抗联合帕博利珠单抗vs化疗联合帕博利珠单抗一线应用的疗效和安全性。该研究的主要终点是经盲法独立中央审查(BICR)使用RECIST v1.1确定的无进展生存期(PFS)。次要终点包括总生存期(OS)、客观缓解率(ORR)、缓解持续时间(DOR)、缓解开始时间(TTR)、患者报告结局(PROs)和安全性(图1)。图1. 研究设计该研究共纳入了443名PD-L1阳性TNBC患者,按1:1随机分组后予以戈沙妥珠单抗联合帕博利珠单抗和化疗联合帕博利珠单抗方案。该研究达到了PFS的主要研究终点,与化疗联合帕博利珠单抗相比,戈沙妥珠单抗联合帕博利珠单抗降低了疾病进展或死亡风险达35%,具有统计学显著性和临床意义(11.2个月 vs 7.8个月; HR 0.65, 95%CI 0.51-0.84; P = 0.0009)(图2上)。OS尚不成熟,但也展现了早期获益的趋势。戈沙妥珠单抗联合帕博利珠单抗方案具有更高的ORR(60% vs 53%),并显示出深度且持久的缓解(完全缓解:13% vs 8%;DOR 16.5个月 vs 9.2个月)(图2,下)。安全性方面,与既往戈沙妥珠单抗及帕博利珠单抗研究一致,未见新的不良事件信号。患者耐受性较好,戈沙妥珠单抗联合帕博利珠单抗组与化疗联合帕博利珠单抗组的不良事件相关停药率为12% vs 31%,为更多患者可以完整接受治疗带来了保障。图2. ASCENT-04研究BICR评估的PFS(上)、缓解状况(下)该研究是首次证实了ADC联合免疫治疗方案可一线应用于TNBC的Ⅲ期临床研究,为TNBC一线治疗带来了新的选择。02肿瘤瞭望:ASCENT-04研究是首次确立ADC联合免疫治疗一线应用地位的Ⅲ期研究。您如何评价该研究结果?将为晚期TNBC治疗格局带来怎样的变化?王坤教授广东省人民医院随着近年来免疫治疗的发展,国内外指南愈加强调免疫治疗联合化疗在TNBC应用的重要性,特别是对于PD-L1阳性患者,免疫治疗联合化疗已成为标准治疗方案[3,4]。此次ASCENT-04研究数据的披露,证实了对于PD-L1阳性(CPS≥10)的患者,一线戈沙妥珠单抗联合免疫治疗优于化疗联合免疫治疗。该结果既确证了Trop-2 ADC联合免疫治疗一线应用的可行性,又标志着Trop-2 ADC从此正式从TNBC二线及其后线治疗迈入一线。在免疫联合化疗作为目前TNBC一线标准治疗方案的背景下,ASCENT-04研究的阳性结果必将改写指南,改变临床实践。随着ASCENT-04研究的成功,我也期待在中国人群中开展相应的桥接研究或类似的临床研究,来验证戈沙妥珠单抗联合免疫治疗的疗效。目前江泽飞教授牵头的多中心、随机、对照的ASCENT-C04研究(图3)正在进行中,旨在探索戈沙妥珠单抗联合特瑞普利单抗对比特瑞普利单抗联合化疗一线治疗TNBC的表现,期待其结果能早日披露,为临床提供更多可能。图3. ASCENT-C04研究设计此外,近日ASCENT-03研究(NCT 05382299)披露信息显示已达到主要终点,取得了高度显著且具有临床意义的PFS改善[5]。该研究旨在验证戈沙妥珠单抗对比化疗在不适合接受PD-1/PD-L1单抗治疗的TNBC患者一线治疗的地位。戈沙妥珠单抗在TNBC一线治疗的全面突破,必将改变一线治疗的临床格局,期待戈沙妥珠单抗能够早日获批该适应症,为患者带来更多的临床治疗选择。03肿瘤瞭望:在ASCENT-04研究的基础上,您对戈沙妥珠单抗联合免疫治疗应用于中国临床实践有哪些期待?殷咏梅教授江苏省人民医院ASCENT-04研究在全球人群中确立了戈沙妥珠单抗联合帕博利珠单抗一线治疗PD-L1阳性乳腺癌的地位。该研究主要针对PD-L1阳性的TNBC患者,我相信对于该人群而言,ASCENT-04研究提供的戈沙妥珠单抗联合帕博利珠单抗方案将替代当前的化疗联合免疫治疗方案。我非常期待未来Trop-2 ADC联合免疫治疗不仅能够为患者带来ORR改善,还能为患者带来更好的总体生存获益。04肿瘤瞭望:在临床实践中,安全性管理直接影响患者生活质量及生存时间。ADC联合免疫治疗存在哪些常见的不良事件?应如何管理?王坤教授广东省人民医院ASCENT-04研究中,戈沙妥珠单抗联合帕博利珠单抗最常见不良事件为中性粒细胞减少和腹泻,未见其他新的安全信号,与既往文献报告一致,也未见间质性肺病(ILD)、眼毒性、口腔炎等不良事件,临床应用安全可控(图4)。图4. ASCENT-04研究的常见不良事件对于中性粒细胞减少,可使用粒细胞刺激因子(G-CSF)等二级预防;对于存在中性粒细胞减少高风险患者,可以使用G-CSF一级预防;若出现了严重的中性粒细胞减少伴发热,则须开始抗感染治疗。对于腹泻,可通过及时监测并对症补液、补充电解质、使用洛哌丁胺等止泻治疗有效控制[6]。此外,还需要通过患教活动等提高患者对不良事件的认知,做到早发现、早处理。参考文献:(滑动查看)[1] Bardia A, Hurvitz SA, Tolaney SM, et al. Sacituzumab Govitecan in Metastatic Triple-Negative Breast Cancer. N Engl J Med. 2021;384(16):1529-1541. doi:10.1056/NEJMoa2028485[2] Sara M. Tolaney, et al. Sacituzumab govitecan (SG) + pembrolizumab (pembro) vs chemotherapy (chemo) + pembro in previously untreated PD-L1–positive advanced triple-negative breast cancer (TNBC): Primary results from the randomized phase 3 ASCENT-04/KEYNOTE-D19 study. 2025 ASCO LBA 109.[3] 中国临床肿瘤学会指南工作委员会. 中国临床肿瘤学会(CSCO)乳腺癌诊疗指南2025. 人民卫生出版社-北京. 2025.04.[4] ESMO Living Guideline Metastatic Breast Cancer 2025v1.2. Available at:https://www.esmo.org/guidelines/living-guidelines/esmo-living-guideline-metastatic-breast-cancer/triple-negative-breast-cancer/de-novo-mbc-or-recurrence-6-12-months-after-the-end-of-neo-adjuvant-ici[5] Gilead Sciences, Inc. ASCENT-03: Trodelvy® Demonstrates Highly Statistically Significant & Clinically Meaningful Improvement in Progression Free Survival in Patients With First-line Metastatic Triple-Negative Breast Cancer Who Are Not Candidates for Checkpoint Inhibitors. Available at:https://www.gilead.com/news/news-details/2025/ascent-03-trodelvy-demonstrates-highly-statistically-significant--clinically-meaningful-improvement-in-progression-free-survival-in-patients-with-first-line-metastatic-triple-negative-breast[6] 中国医师协会肿瘤医师分会乳腺癌学组,中国抗癌协会国际医疗交流分会. 中国乳腺癌抗体药物偶联物安全性管理专家共识[J]. 中华肿瘤杂志,2022,44(09):913-927.殷咏梅 教授教授,主任医师,博士生导师江苏省人民医院(南京医科大学第一附属医院、江苏省妇幼保健院)副院长中国临床肿瘤学会(CSCO)副理事长北京市希思科临床肿瘤学研究基金会副理事长第19届St.Gallen国际乳腺癌大会专家团成员CSCO乳腺癌专家委员会秘书长中国抗癌协会乳腺癌专业委员会常委CSCO患者教育专家委员会主任委员CSCO BC指南执笔专家荣获2021年度,2023年度中国生物医药产业链创新风云榜“Leading Pl桂冠奖”王坤 教授广东省人民医院肿瘤医院副院长博士研究生导师CSCO和CBCS乳腺癌专委会常委2019年国之名医获得者2021年NeoCART研究入选美国NCCN乳腺癌指南2023年人民好医生-乳腺癌领域杰出贡献奖获得者(来源:《肿瘤瞭望》编辑部)声 明凡署名原创的文章版权属《肿瘤瞭望》所有,欢迎分享、转载。本文仅供医疗卫生专业人士了解最新医药资讯参考使用,不代表本平台观点。该等信息不能以任何方式取代专业的医疗指导,也不应被视为诊疗建议,如果该信息被用于资讯以外的目的,本站及作者不承担相关责任。
ASCO会议临床结果抗体药物偶联物临床3期
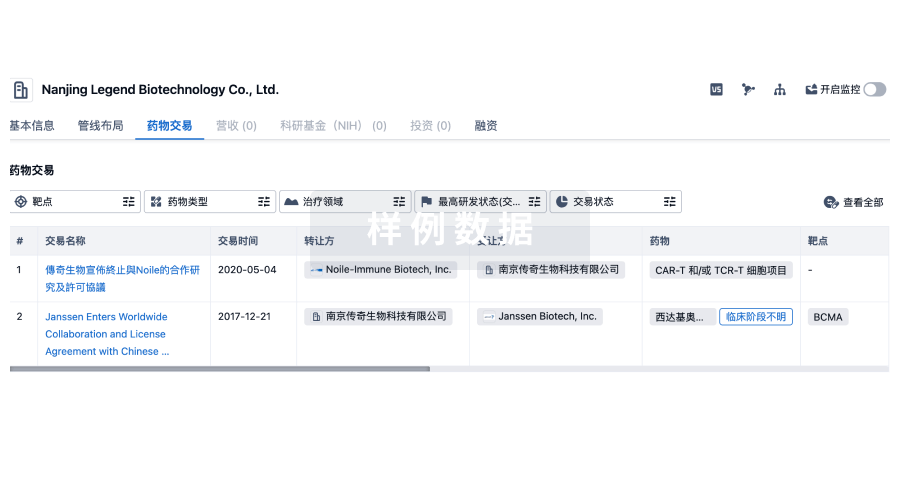
100 项与 Korea University Anam Hospital 相关的药物交易
登录后查看更多信息
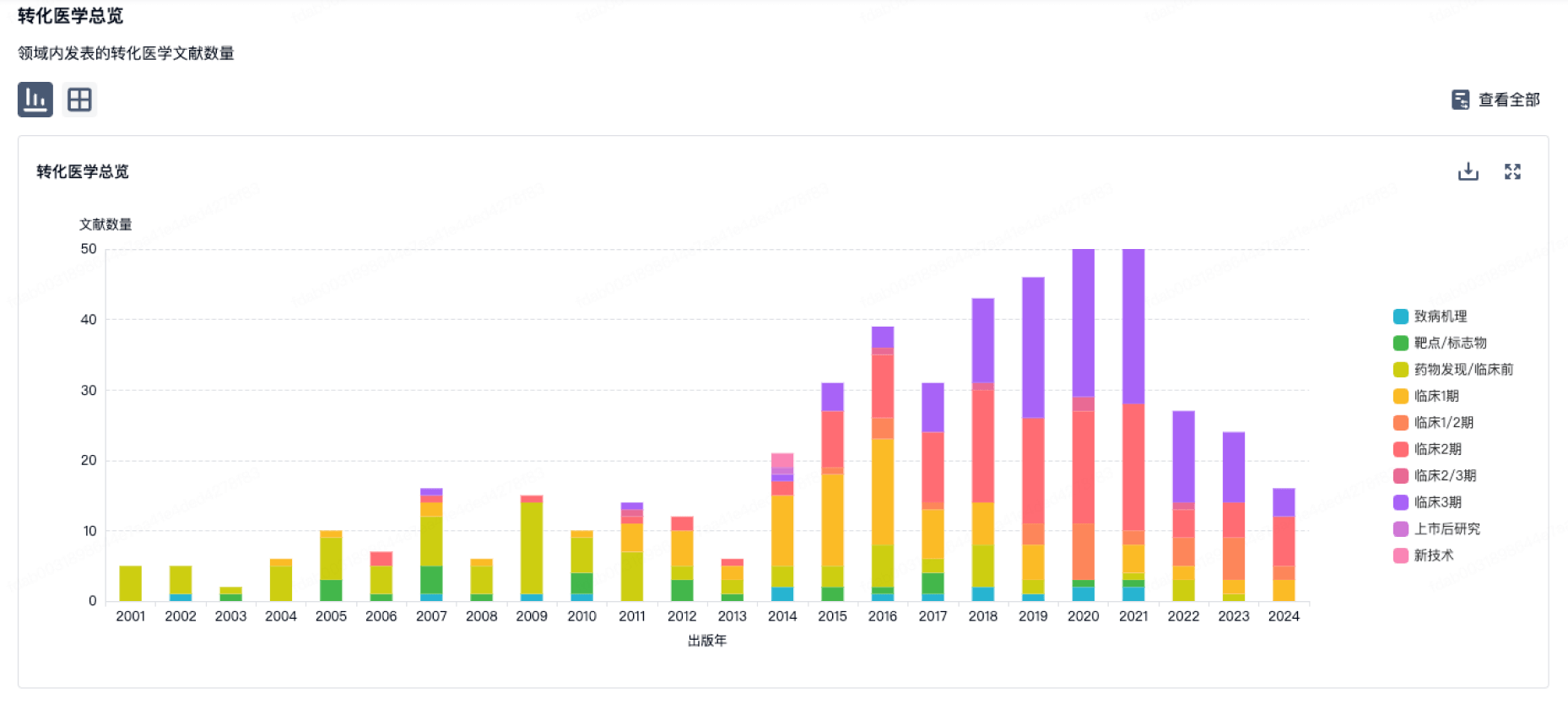
100 项与 Korea University Anam Hospital 相关的转化医学
登录后查看更多信息
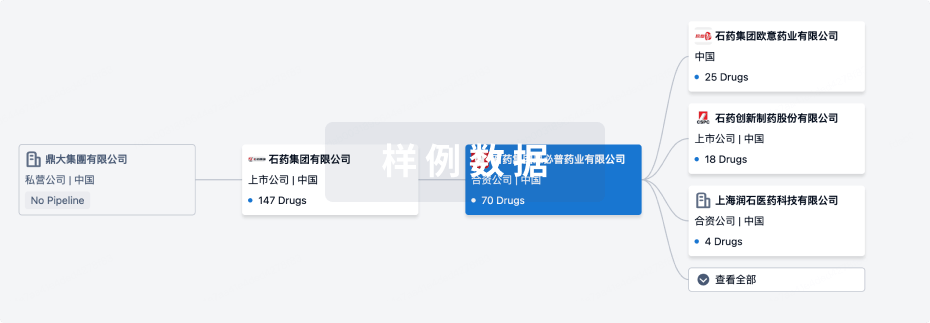
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年11月03日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
其他
2
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
Umbilical Cord-derived Mesenchymal Stem Cells(Korea University Anam Hospital) | 肩袖肌腱炎 更多 | 临床阶段不明 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
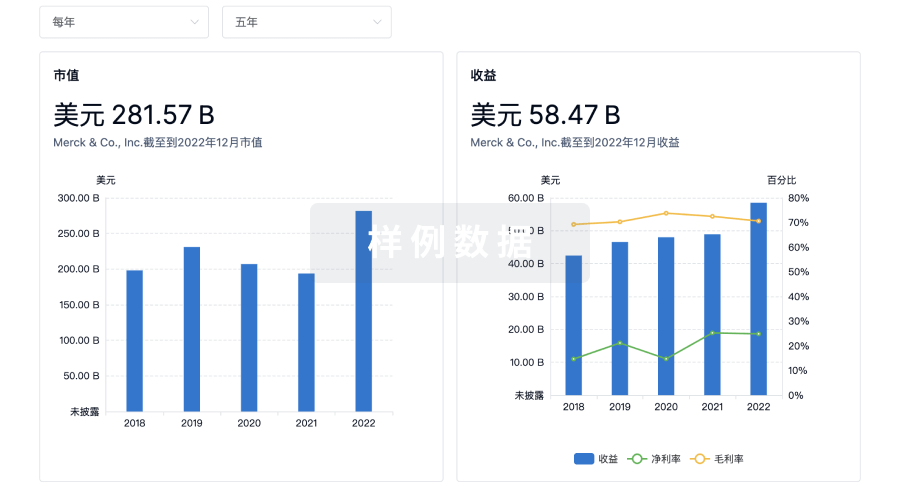
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
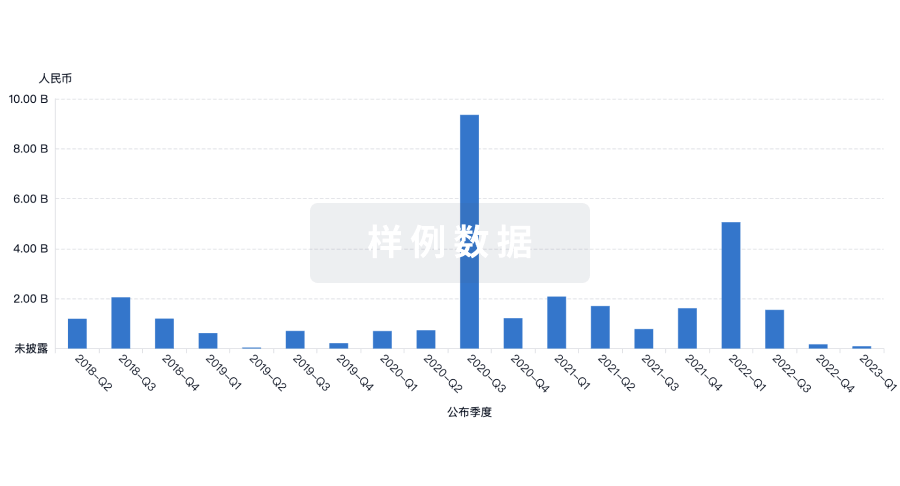
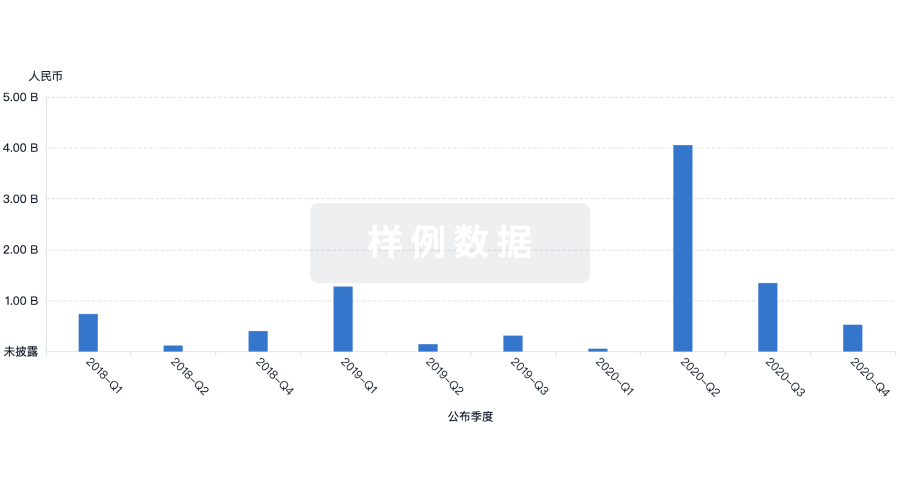
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
