预约演示
更新于:2025-05-07
Corporacion Sanitaria Parc Tauli
私营公司|Spain
私营公司|Spain
更新于:2025-05-07
概览
关联
174
项与 Corporacion Sanitaria Parc Tauli 相关的临床试验NCT06597929
The Effectiveness of Moderate-vigorous Intermittent Lifestyle Physical Activity and Health Education to Increase Intense Physical Activity in Stroke Survivors: a Pragmatic Randomised Controlled Trial (MV-ILPA-stroke)
Stroke is the leading cause of disability in Spain. Additionally, it is the second leading cause of death in women and the third in both sexes. Regular physical activity (PA) helps prevent and manage stroke. It also helps with hypertension, maintains a healthy body weight, and improves mental health, quality of life, and well-being. PA plays a prominent role in inpatient care after stroke. However, stroke survivors become more sedentary when discharged from the hospital. They have muscle weakness, reduced balance, and fatigue. Consequently, PA levels of community-dwelling post-stroke individuals remain lower than their age-matched counterparts. Continued PA can help this population maintain and improve physical function, and reduce long-term functional limitations, and mortality risk.
开始日期2025-04-01 |
申办/合作机构 |
NCT06900335
Characterization of the Functional Connectome in Prader-Willi Syndrome: Integrating Neuroimaging and Artificial Intelligence to Assess the Impact of Physiological and Therapeutic Interventions
The goal of this observational study is to explore brain network changes and identify patterns related to hyperphagia, hormonal treatment effects, and cognitive deficits in adults with Prader-Willi Syndrome (PWS). The main questions it aims to answer are:
* How are brain connectivity patterns altered in PWS patients compared to healthy and obese controls?
* How do brain network changes relate to hyperphagia and the response to growth hormone therapy?
Researchers will compare PWS patients to healthy and obese controls to see if there are significant differences in brain network connectivity before and after meals and growth hormone therapy. Ultimately, researchers will try to develop predictive models of treatment outcomes using AI and machine learning.
* How are brain connectivity patterns altered in PWS patients compared to healthy and obese controls?
* How do brain network changes relate to hyperphagia and the response to growth hormone therapy?
Researchers will compare PWS patients to healthy and obese controls to see if there are significant differences in brain network connectivity before and after meals and growth hormone therapy. Ultimately, researchers will try to develop predictive models of treatment outcomes using AI and machine learning.
开始日期2025-03-01 |
NCT06873360
Design of a Medical Device for Oxaliplatin-Induced Peripheral Neuropathy Considering the Patient's Voice in Gastrointestinal Cancer
This is an observational study related to a medical device designed for the prevention of oxaliplatin-induced peripheral neuropathy (OIPN) in patients with gastrointestinal cancer. The primary objective is to collect data through interviews with patients experiencing OIPN symptoms to co-design the medical device prototype, incorporating the patient's perspective. Additionally, the study aims to identify clinical and usability patterns that will help optimize the design of a future clinical investigation assessing the safety and efficacy of the final device.
开始日期2025-03-01 |
100 项与 Corporacion Sanitaria Parc Tauli 相关的临床结果
登录后查看更多信息
0 项与 Corporacion Sanitaria Parc Tauli 相关的专利(医药)
登录后查看更多信息
115
项与 Corporacion Sanitaria Parc Tauli 相关的文献(医药)2025-06-01·The Lancet Regional Health - Europe
Safety and efficacy of combined portal and hepatic vein embolisation in patients with colorectal liver metastases (DRAGON1): a multicentre, single-arm clinical trial
Article
作者: Grünhagen, Dirk J ; Imani, Farshad ; Andorrà, Esteban Cugat ; Seeger, Nico ; Moragues, Jaume Sampere ; Herrero, Eric ; Dewulf, Maxime J L ; Serenari, Matteo ; Billingsley, Kevin G ; Arntz, Pieter J W ; van Baardewijk, Laurens J ; Leclercq, Wouter K G ; Fretland, Åsmund A ; Lindsay, Richard ; Vogl, Thomas J ; Bemelmans, Marc H A ; Hoffmann, Martin H ; Ryan, Stephen ; Xudong, Qu ; Navinés-López, Jordi ; Erdmann, Joris I ; van Dam, Ronald M ; Korenblik, Remon ; Baclija, Ivan ; Wang, Xiaoying ; Zijlstra, IJsbrand A J ; Schnitzbauer, Andreas ; Wohlgemuth, Walter A ; Udupa, Venkatesha ; Delle, Martin ; Fouraschen, Suomi M G ; De Cobelli, Francesco ; Carling, Ulrik ; Criado, Eva ; Björnsson, Bergthor ; Macdonald, Andrew ; Suarez, Yiliam Fundora ; Vass, David G ; Díaz-Nieto, Rafael ; Detry, Olivier ; Madoff, David C ; Pieterman, Kay J ; Davis, Rob ; Heil, Jan ; Binkert, Christoph A ; Metrakos, Peter ; Serrablo, Alejandro ; Primrose, John N ; Aldrighetti, Luca A ; Ridouani, Fourat ; Kleeff, Jörg ; Borel Rinkes, Inne H M ; Stavrou, Gregor A ; Kalil, Jennifer ; Moelker, Adriaan ; Smits, Jens ; de Boer, Marieke T ; Olde Damink, Steven W L ; Sparrelid, Ernesto ; Gelabert, Arantxa ; Sarriá, Luis ; Kollmar, Otto ; Modi, Sachin ; Chan, Benjamin K Y ; Bokkers, Reinoud P H ; Gruenberger, Thomas ; Schadde, Erik ; De Boo, Diederick W ; Muños, Fernando Gómez ; Valenti, David ; van der Leij, Christiaan ; Spuentrup, Elmar ; Winkens, Bjorn ; Martel, Guillaume ; Cappelli, Alberto ; Sandström, Per A ; Kingham, T Peter ; Gerard, Laurent ; Borobia, Francisco G ; Gobardhan, Paul D ; Croagh, Daniel ; Breitenstein, Stefan ; Smits, Maarten L J ; James, Sinéad ; Tasse, Jordan C
2023-10-01·Pediatric Pulmonology
Characteristics and management of patients with SARS‐CoV2 infection admitted to pediatric intensive care units: Data analysis of the Spanish national multicenter registry
Article
作者: Belda Hofheinz, Sylvia ; Slöcker Barrio, María ; Jiménez Olmos, Ainhoa ; Holanda Peña, Maria Soledad ; García-Salido, Alberto ; Rey Galan, Corsino ; Huidobro Labarga, Beatriz ; González Navarro, Pablo ; Martínez Padilla, Carmen ; Oulego-Erroz, Ignacio ; Roca Pascual, David ; Hernández Yuste, Alexandra ; Cuervas-Mons Tejedor, Maite ; Rodríguez Rubio, Miguel ; Sanchíz Cárdenas, Sonia ; Morteruel Arizcuren, Elvira ; García-Besteiro, Maria ; Bermúdez Barrezueta, Lorena ; Guitart Pardellans, Carmina ; Cortés, Rafael González ; Calvo Monge, Cristina ; de Carlos Vicente, Juan Carlos
2023-06-01·Journal of Clinical Oncology
Impact of WNT/B-catenin alterations and metastasis location among patients with metastatic colorectal cancer (mCRC) treated with immune checkpoint inhibitors (ICI) combinations.
作者: Vega, Sharela ; Baraibar, Iosune ; Alonso, Guzman ; Tabernero, Josep ; Salva, Francesc ; Garcia, Ariadna ; Navarro Garces, Victor ; Ros Montañá, Javier ; Garralda, Elena ; Saoudi Gonzalez, Nadia ; Bueno, Sergio ; Saavedra, Omar ; Elez, Elena ; Rodríguez Castells, Marta ; Vivancos, Ana ; Comas, Raquel
100 项与 Corporacion Sanitaria Parc Tauli 相关的药物交易
登录后查看更多信息
100 项与 Corporacion Sanitaria Parc Tauli 相关的转化医学
登录后查看更多信息
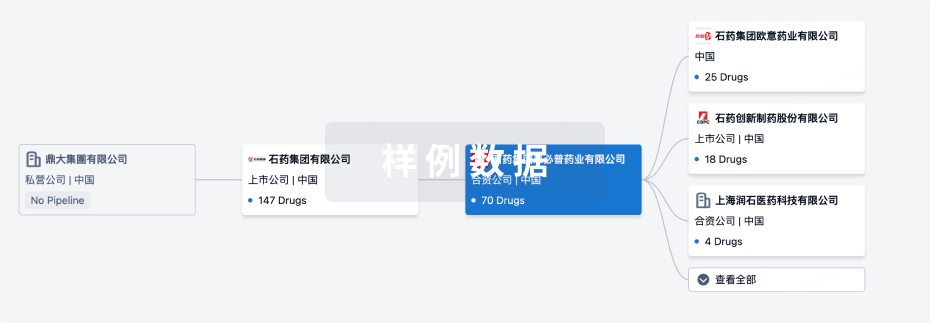
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年07月27日管线快照
无数据报导
登录后保持更新
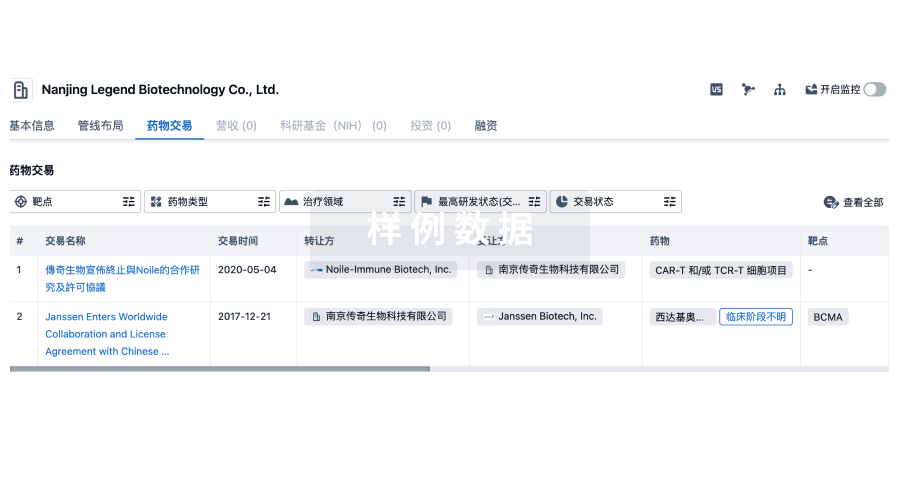
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
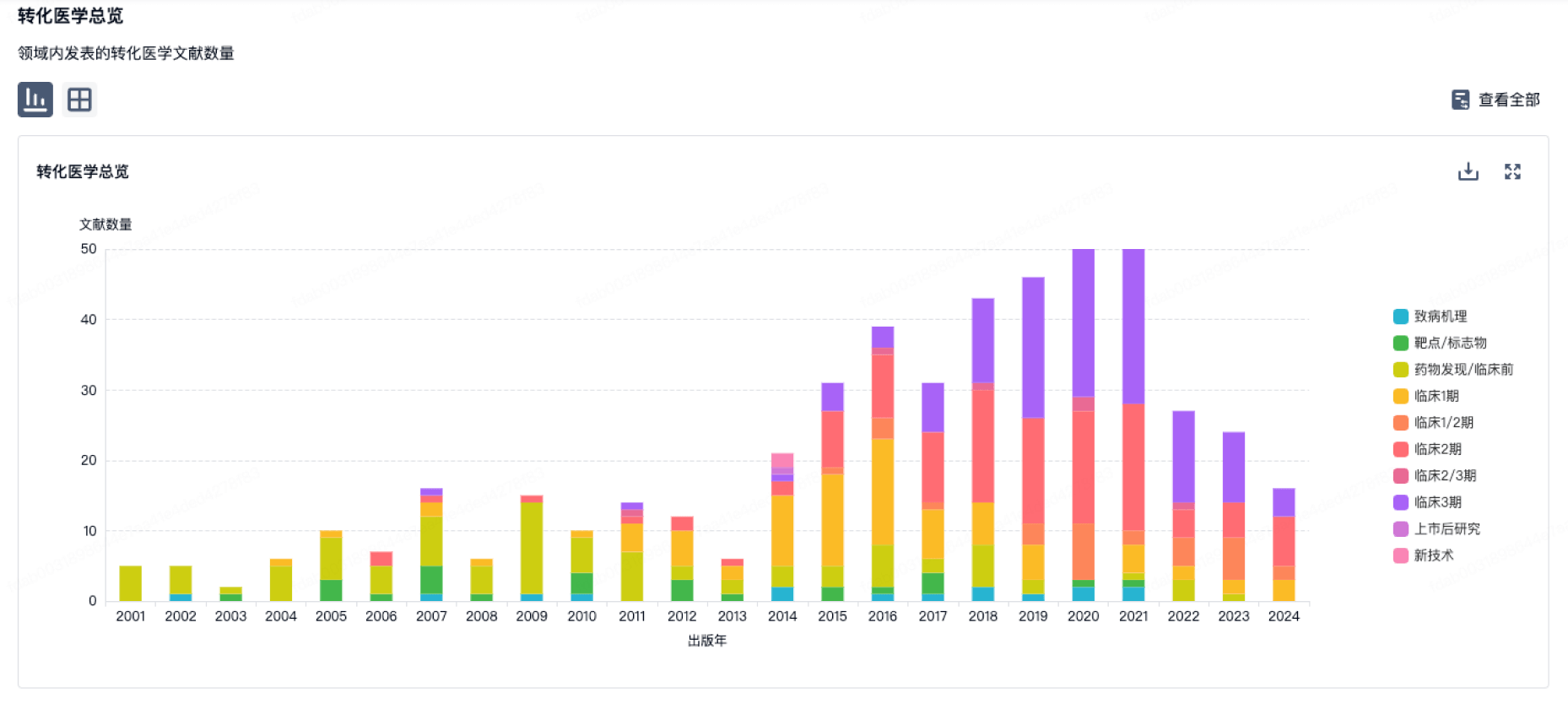
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
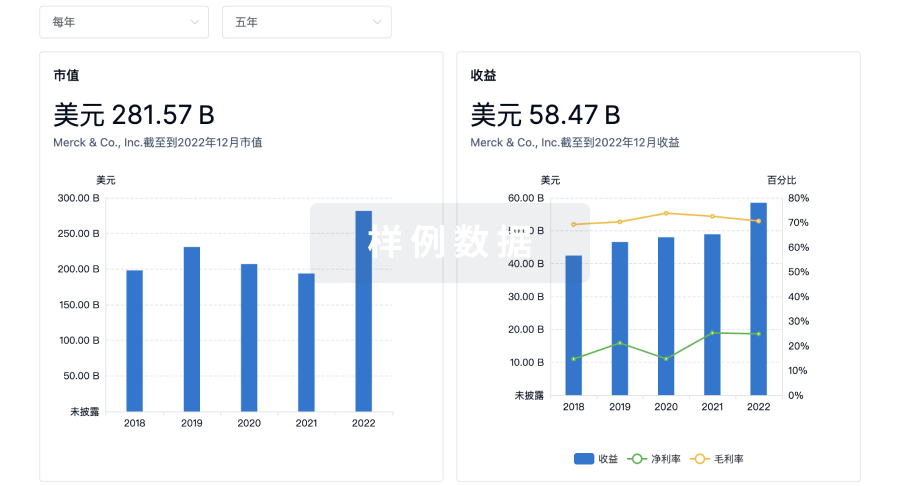
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
