预约演示
更新于:2025-08-27

Polaris Inc.
更新于:2025-08-27
概览
标签
血液及淋巴系统疾病
免疫系统疾病
酶
关联
1
项与 Polaris Inc. 相关的药物作用机制 尿酸刺激剂 |
在研机构 |
原研机构 |
非在研适应症- |
最高研发阶段临床2期 |
首次获批国家/地区- |
首次获批日期- |
100 项与 Polaris Inc. 相关的临床结果
登录后查看更多信息
0 项与 Polaris Inc. 相关的专利(医药)
登录后查看更多信息
180
项与 Polaris Inc. 相关的文献(医药)2022-01-01·LWT-FOOD SCIENCE AND TECHNOLOGY
Functional annotation unravels probiotic properties of a poultry isolate, Bacillus velezensis CGS1.1
作者: Ninad Pandit ; Christopher Dunlap ; Hareshkumar Keharia ; Jayraj Doshi ; Riteshri Soni
Probiotics are an eco-friendly and prospective substitute for antibiotic growth promoters.The present investigation aimed to dissect the probiotic attributes of a poultry isolate CGS1.1 by integrating genomics and phenotypic traits.The strain exhibited bile salt hydrolase activity and ∼73% survival in simulated gastrointestinal juices.It displayed notable aggregation, cell surface hydrophobicity, biofilm formation, and antimicrobial activity against gram-pos. and gram-neg. bacterial pathogens.Interestingly, the strain CGS1.1 completely inhibited the growth of E. coli and S. enterica after 24 h in liquid co-culture assay.The strain CGS1.1 effectively hydrolyzes starch, cellulose, pectin, tributyrin, casein, and phytate.The in silico genome anal. revealed its identity as Bacillus velezensis.Genome annotation revealed the presence of genes encoding the aforementioned probiotic properties.Furthermore, CGS1.1 was found to be non-hemolytic and sensitive to major classes of antibiotics.No potent virulent factor or toxin encoding genes could be predicted in CGS1.1 genome signifying its safety.The demonstrate the potential of CGS1.1 as a probiotic to promote chicken growth and control pathogens.
2021-12-15·Cancer1区 · 医学
Assessment of pegylated arginine deiminase and modified FOLFOX6 in patients with advanced hepatocellular carcinoma: Results of an international, single‐arm, phase 2 study
1区 · 医学
Article
作者: Lee, Dae‐Won ; El Dika, Imane ; Huang, Wen‐Tsung ; Yang, Tsai‐Sheng ; Ryoo, Baek‐Yeol ; Ho, Ching‐Liang ; Qin, Shukui ; Chen, Yen‐Yang ; Sarker, Debashis ; Harding, James J. ; Meyer, Timothy ; O’Reilly, Eileen M. ; Cohen, Stacey A. ; Akce, Mehmet ; Tan, Benjamin ; Feng, Yin‐Hsun ; Johnston, Amanda ; Bomalaski, John S. ; Abou‐Alfa, Ghassan K. ; Lim, Ho Yeong ; Yen, Chia‐Jui
Background:
Arginine starvation depletes the micronutrients required for DNA synthesis and interferes with both thymidylate synthetase activity and DNA repair pathways in preclinical models of hepatocellular carcinoma (HCC). Pegylated arginine deiminase (ADI‐PEG 20), an arginine degrader, potentiates the cytotoxic activity of platinum and pyrimidine antimetabolites in HCC cellular and murine models.
Methods:
This was a global, multicenter, open‐label, single‐arm, phase 2 trial of ADI‐PEG 20 and modified 5‐fluorouracil, leucovorin, and oxaliplatin (mFOLFOX6) in patients who had HCC with Child‐Pugh A cirrhosis and disease progression on ≥2 prior lines of treatment. The primary objective was the objective response rate assessed according to Response Evaluation Criteria in Solid Tumors, version 1.1. Secondary objectives were to estimate progression‐free survival, overall survival, safety, and tolerability. Eligible patients were treated with mFOLFOX6 intravenously biweekly at standard doses and ADI‐PEG‐20 intramuscularly weekly at 36 mg/m2.
Results:
In total, 140 patients with advanced HCC were enrolled. The median patient age was 62 years (range, 30‐85 years), 83% of patients were male, 76% were of Asian race, 56% had hepatitis B viremia, 10% had hepatitis C viremia, 100% had received ≥2 prior lines of systemic therapy, and 39% had received ≥3 prior lines of systemic therapy. The objective response rate was 9.3% (95% confidence interval [CI], 5.0%‐15.4%), with a median response duration of 10.2 months (95% CI, 5.8 months to not reached). The median progression‐free survival was 3.8 months (95% CI, 1.8‐6.3 months), and the median overall survival was 14.5 months (95% CI, 13.6‐20.9 months). The most common grade ≥3 treatment‐related events were neutropenia (32.9%), white blood cell count decrease (20%), platelet count decrease (19.3%), and anemia (9.3%).
Conclusions:
Concurrent mFOLFOX6 plus ADI‐PEG 20 exhibited limited antitumor activity in patients with treatment‐refractory HCC. The study was terminated early, and no further evaluation of the combination will be pursued.
Lay Summary:
Arginine is an important nutrient for hepatocellular carcinoma (HCC).The depletion of arginine with pegylated arginine deiminase (ADI‐PEG 20), an arginine degrader, appeared to make chemotherapy (FOLFOX) work better in animal models of HCC and in patients with HCC on an early phase clinical trial.To formally test this hypothesis in the clinical setting, a large, global, phase 2 clinical trial was conducted of ADI‐PEG 20 and FOLFOX in the treatment of patients with refractory HCC.The study showed limited activity of ADI‐PEG 20 and FOLFOX in advanced HCC and was stopped early.
2021-10-01·Journal of plastic, reconstructive & aesthetic surgery : JPRAS3区 · 医学
The chimeric medial sural artery perforator flap as the ideal for partial tongue reconstruction: A case series and technical refinements
3区 · 医学
Article
作者: Siti Radhziah Binte Sudirman ; Marcus J.M. Ng ; David Chang ; Adrian S.H. Ooi
BACKGROUND:
The medial sural artery perforator free flap (MSAP) has gained increasing popularity in head and neck reconstruction. Its slightly bulkier nature than the radial forearm flap, combined with negligible donor site morbidity, makes it an ideal candidate for the reconstruction of partial glossectomy defects. The ability to harvest the MSAP as a chimeric flap with a portion of the medial gastrocnemius muscle gives it greater flexibility in soft tissue reconstruction.
METHODS:
A retrospective study of patients with partial glossectomy defects reconstructed using the MSAP by a single surgeon was performed. Perioperative data, donor and recipient site characteristics, complications, and outcomes were analyzed. A video is included to show technical points for the harvest of the flap.
RESULTS:
A total of 10 patients were included. The average age was 59.1 years, with a mean of 43.5% of the tongue resected. All flaps survived, with no major complications. At follow-up, the patients had regained an average of 86.5% of original speech, with none requiring NG feeding. The average MSAP skin flap thickness was 7.8 mm, with 6 flaps being harvested as chimeric fasciocutaneous muscle flaps. Five flaps incorporated 2 perforators. Two case examples are presented.
CONCLUSION:
The chimeric MSAP perforator allows for more robust partial glossectomy reconstruction with improved postoperative functional outcomes. It should be considered as the workhorse flap for partial tongue reconstruction.
92
项与 Polaris Inc. 相关的新闻(医药)2025-04-27
买科研服务(代计算、代测试、超算机时),送老李校长“科研理工男士情感课”第一性原理计算解决50年悬而未决难题:半导体中铜为何扩散更快?Ab initio及第一性原理入门参考书介绍《海贼王》告诉你,做科研为什么不能闭门造车……985博导亲测:用DeepSeek写国自然本子,3天完成30天工作量来自公众号:药研小木子本文以传播知识为目的,如有侵权请后台联系我们,我们将在第一时间删除。来自人工智能(AI)的洞见最终可能会改变药物开发,如果生物学和化学数据的质量与数量能够得到提升。药物发现极其困难。德国汉堡的生物技术公司 Evotec 的计算化学家 David Pardoe 指出:“在约100年的当代医学史中,我们只找到了大约7000种罕见病中约500种的治疗方法。” 他说:“这太费时,成本也太高。” 但从理论上讲,并且令许多人感到兴奋的是,AI有望解决这两个问题。位于美国马萨诸塞州波士顿的人工智能生物技术公司 Insilico Medicine 的机器人实验室。图片来源:Insilico MedicineAI 应该能够整合潜在类药分子的三维几何结构和原子结构,并构建其如何与靶点蛋白结合或适配的图景。然后可以调整设计,以提高潜在药物的药效,或者算法可以识别全新的可探索靶点。AI 系统还可能考虑药物与其靶点相互作用的关键背景:患者体内复杂的生物环境。与各种非靶点蛋白发生的非预期相互作用,可能会使一个原本有前景的分子产生副作用。开发能够推动药物发现过程的系统的关键在于大量高质量的数据。与 AI 正在应用的某些其他领域的科学家相比,寻求将这项技术应用于药物开发的研究人员拥有坚实的基础:世界各地的实验室都在持续产生大量生物数据。然而,尽管现有数据的规模可能暗示着 AI 对药物开发的转型势在必行,但这不一定成为现实。数据的质量并非总是达标,因为其中大部分数据并非为机器学习而收集。实验方法和数据记录方式缺乏一致性会带来问题,只发表阳性结果的偏倚也是如此。虽然有些人认为大量的数据本身就是解决方案,但另一些人则认为学术界和产业界的研究人员必须携手合作,提高用于机器学习模型的数据质量。AI药物设计并不像人们认为的那么简单哪些问题最紧迫,哪些解决方案应优先考虑,这些仍有待讨论。《自然》杂志采访了一些活跃在该领域的研究人员,以期探寻可以采取哪些措施,从而使 AI 能够达到许多人期望的程度来改变药物发现和开发。1、规范报告和方法学术界科学家以其灵活性为荣。他们使用现有设备进行实验。如果有机会将更好的机器或流程纳入他们的方法,他们就会抓住这个机会。这种态度使他们跟紧前沿,但这可能会给机器学习带来问题。“对 AI 来说,一个巨大的问题是数据的产生方式”位于巴黎的 AI 生物技术公司 Owkin 的首席数据科学官 Eric Durand 说。Bioptimus 正在构建第一个通用的 AI 基础模型,将生物学在不同尺度上连接起来:从分子到细胞、组织和整个生物体当不同实验室使用不同的方法、试剂和机器时,由此产生的数据中可能会引入被称为批次效应的不一致之处。样本处理方案的微小差异、不同批次试剂和细胞之间的变异,甚至像分子结构的描述或命名方式这样基本的问题,都是变异的来源,而对模式高度敏感的 AI 模型可能会错误地将其解读为具有生物学意义。“你不能简单地将由两个实验室生成的数据集共同分析,而不进行预处理。” Durand 说。这削弱了许多在 AI 浪潮到来之前建立的大型公共数据库的效用。例如,ChEMBL 是一个免费、精心整理的生物活性分子数据库,汇集了研究报告、专利及其他数据库的信息,被广泛用于药物发现领域。它由位于英国欣克斯顿的欧洲生物信息学研究所维护,并试图最大限度地减少批次效应,但其整合信息的方式意味着不一致之处仍然存在。“你需要小心”位于马萨诸塞州剑桥的生物技术公司 Relay Therapeutics 的计算化学家 Pat Walters 说。“你的数据来自实验方式不同的实验室,因此很难进行公平比较。”一些人认为,生成 AI 所需规范化数据的最佳方法是制定关于如何进行实验和报告结果的规则。例如,疾病和基因的名称可以从一开始就统一,实验方案可以预先商定。一个实践中的例子是人类细胞图谱(Human Cell Atlas),这是一个2016年启动的全球项目,已经以严谨且标准化的方式绘制了人体数百万个细胞的图谱。这提供了具有一致性的数据,是 AI 算法寻找潜在药物靶点的理想“食粮”。人类肺细胞已由人类细胞图谱项目绘制,这是一个全球联合体,旨在创建所有人类细胞的全面参考图谱。图片来源:Nathan Richoz Univ. Cambridge一项名为 Polaris 的用于药物发现的基准平台——也旨在帮助清理和标准化用于机器学习的数据集。它在2024年末的一篇预印本文章中提出了指导原则,目前正在征集反馈意见。Polaris 概述了数据集的基本检查。例如,创建者必须解释数据是如何生成的以及应如何使用,并且必须引用其借鉴的来源。它警告说,检查明显的重复数据和模糊不清的数据是创建者的责任。“我们还会请专家审查一些公开可用的数据集,以便让社群了解哪些数据质量高,哪些不高。” Walters 说。Polaris 为那些达到标准的数据集引入了认证标记。Pardoe 表示,如果不能进一步努力生成统一且相关的数据,持续开发更先进的算法可能价值不大。“一旦有了那些‘好的’数据,我们就能朝着正确的方向取得快速而显著的进展。”Polaris(https://polarishub.io/)的抗病毒药物研发平台2、认识到阴性结果的价值对学术研究人员而言,报告实验失败通常收获甚微。那些尝试报告的人通常发现他们的研究成果很难发表。科学界这种固有的偏向发表阳性结果的倾向并非新鲜事,但这给 AI 的使用带来了特殊问题。来自已发表成果并输入到算法中的数据,必然会呈现一个扭曲的、粉饰太平的生物学图景。例如,关于在动物实验中显示出前景且无毒性作用的成熟化合物的数据比关于不成功的化合物的数据要多,因此,用于药物发现的 AI 模型将很大程度上缺乏关于许多隐藏失败的信息。伦敦国王学院的药物化学家 Miraz Rahman 指出了在研发新抗生素过程中存在的这种偏倚的一个例子。杀死微生物的关键一步是将化合物送进细菌细胞内部,许多已发表的研究表明,伯胺——一种结构类似于氨的小化合物——有助于药物进入细菌。“如果你基于已发表的研究询问一个 AI 模型,它会不断推荐含有伯胺的化合物,” Rahman 说。但他知道自己不得不忽略这个建议,“我的实验室有很多数据显示这行不通。” 对于 AI 来说,问题在于像 Rahman 的这些失败案例尚未被发表。这种偏向分享阳性结果的偏倚也困扰着制药公司。Rahman 说:“什么会被发表的总是成功案例?”当公司选择不公开他们的阴性发现时,呈现在算法面前的表象就会比现实更简单、更光鲜。解决这个问题的一种方法是从一开始就明确旨在汇编阴性和阳性结果。一个备受关注的此类项目由加州大学旧金山分校的结构生物学家 James Fraser 领导,并由美国卫生高级研究计划局(ARPA-H)资助。其关注点在于所谓的药代动力学,它描述了人体如何处理化合物。AI生成的结构很美,但是不一定对。药物的命运取决于其被人体吸收、分布、代谢和排泄的方式——这统称为 ADME。如果人体清除化合物过慢,可能会带来安全风险。但清除过快也同样是个问题。“你可能会设计出一个与目标靶点紧密结合的分子,但如果这个分子被快速排泄,它就没有药物价值。” Walters 说,他是这个项目的支持者。药物还可能与体内的非靶点蛋白相互作用,这可能引发毒性,并减缓或减少药物到达预期靶点的剂量。这些 ADME 问题往往只在药物开发的后期出现,并可能导致代价高昂的失败。“目前这个过程有点像打地鼠。” Fraser 说。“你设计新分子来解决一个缺陷,然后又出现另一个缺陷,你又围绕它再次进行优化。”Fraser 将他目前旨在为 AI 工具提供发现这些陷阱所需数据的工作称为“避开组学”(avoid-ome)项目,因为它寻求生成的不是药物靶点的数据,而是研究人员通常希望避开的蛋白数据。目的是建立一个与 ADME 相关的蛋白结合的实验和结构数据集库。自十月获得资助以来,他的实验室已开始对 ADME 的代谢方面进行测试。 与药物代谢和药代动力学 (DMPK) 相关的“avoidome”相关的选定蛋白质的结构表示这些结果应有助于创建能够优化候选药物药代动力学的预测性 AI 模型。Fraser 说:“人们将合成更少的分子,对所有潜在缺陷有更全面的整体认识,并更快地找到一个能通过所有标准并进入人体测试的分子。”3、分享产业数据和专业知识制药公司拥有大量数据,包括阴性结果,并努力以标准化的方式收集这些数据,使其非常适合 AI 模型消化。然而,这些数据中只有一小部分进入公共领域—— Rahman 估计,更开放的制药公司仅发表约 15-30% 的数据,临床试验的数据公开率可高达 50%。这些数据所蕴含的价值,公司自身深知。2018年,瑞士巴塞尔的制药公司诺华(Novartis)首席执行官 Vas Narasimhan 曾描述将公司重塑为一家“医药和数据科学公司”,强调其拥抱 AI 进行药物发现的雄心。因此,大多数制药公司都极不情愿与学术界和彼此分享数据。“像诺华这样的公司——我曾在那里工作多年——有数万种化合物,他们评估了这些化合物与某些蛋白的结合情况,” Durand 说。“但他们不想与竞争对手分享这些,因为这确实是它们的主要资产。”Owkin 参与的一项旨在鼓励制药公司间数据共享的努力是欧盟资助的 Melloddy 项目。该项目采用了联邦学习方法,使得十家公司能够在不向竞争对手泄露敏感生物和化学数据的情况下协作训练预测性软件。在该项目中,训练用于关联分子化学结构与其生物活性的模型,其准确性显著高于大多数公司现有的模型。具有两个不同规模伙伴的联邦设置的概念表示,展示了跨端点和跨化合物联邦。然而,并非所有人都被打动。合并以不同方式产生的数据时出现的常见问题,也适用于来自不同公司的数据。此外,数据的匿名化可能会降低其丰富性。Walters 解释说:“在不泄露用于生成数据集的化学结构和检测方法性质的情况下,很难合并数据集。”该项目也没有改善学术界所依赖的公共数据集的状况,学术界的研究人员足够聪明,知道无论怎么请求也无法让他们轻易获取制药公司的数据资源库。相反,一些研究人员呼吁制药公司利用他们的另一个巨大优势来支持公共数据库:资金。研究人员可获得的最有价值的数据集之一是英国生物样本库(UK Biobank),它系统地收集了来自英国 50 万人的遗传、生活方式和健康信息以及生物样本。这项工作已获得超过 5 亿英镑(6.32 亿美元)的资助,但主要来自政府和慈善机构。波士顿的 AI 生物技术公司 Insilico Medicine 的创始人兼首席执行官 Alex Zhavoronkov 说:“大型制药公司应该资助诸如英国生物样本库之类的倡议。”UK Biobank是全球规模最大、可广泛获取的遗传流行病学数据集。该数据集包含50万个体的基因型、全外显子组和全基因组测序数据,并与数千份自我报告的性状、医院和初级保健记录、生物标志物指标、心理健康信息和影像数据相关联4、充分利用现有资源一些研究人员认为,海量的数据——以及更智能的处理——将在很大程度上克服利用 AI 进行药物发现的困难。Zhavoronkov 说:“有了足够的数据,你就能学会如何泛化。” Insilico Medicine 将来自美国政府数十亿美元研究资助项目的数据,与已发表论文、临床试验、专利以及遗传和化学数据库关联起来。Zhavorovkov 说:“现代 AI 工具能让你将创新追溯到资助项目。”Zhavoronkov表示,制药公司应该支持诸如英国生物样本库(一个包含来自 50 万人信息的生物医学数据库)之类的项目。接着对这些原始数据进行处理。在 Insilico,这包括引入评分,例如,帮助算法权衡结果的重要性和真实性。Zhavoronkov 说:“我们有一个工具可以评估发表论文的科学家的可信度。如果一个人以前有过不实行为,那么他们再次不实的可能性就更高。” Insilico 还追踪公司公布临床试验结果后的股票价格走势。如果股价急剧下跌,无论公司怎么说,都会被假定结果是阴性的。2019年末,Insilico 的 AI 驱动药物发现平台 PandaOmics 发现了一个涉及过度瘢痕组织形成的纤维化疾病靶点。然后,它使用其生成式 AI 平台 Chemistry42 寻找能够阻断该靶点的化合物⁴。该算法利用包括 ChEMBL 在内的大型现有分子数据库,学习化学结构中的模式并设计潜在药物。去年八月,Insilico 完成了一项 IIa 期小分子药物研究,用于治疗患有特发性肺纤维化(一种肺部瘢痕形成疾病)的成年人。该公司目前正在计划后续试验,Zhavoronkov 期待取得更多成功。他说:“自 2019 年以来,我们已经确定了 22 个临床前候选药物。”利用人工智能开发的肠道限制性 PHD 抑制剂修复肠粘膜屏障并调节免疫的研究,图片来源于Nature biotechnology毫无疑问,一些大型公共数据库对于 AI 来说会更难利用。以整体 RNA 序列为例。它们由捣碎的组织样本汇编而成,对许多细胞的基因表达进行平均。如今,单细胞 RNA 序列被视为更优,因为它们可以用于检测稀有细胞正在产生哪些蛋白,并且在组织绘图中提供更好的分辨率。但 Zhavoronkov 主张不要忽视任何不尽理想的公共数据。他说:“这些数据必须被重新利用。许多动物为此牺牲了,AI 需要用这些数据进行训练。”他主张创建更小、高质量的数据集,用于测试在更大、可能存在缺陷的数据集上训练的 AI 模型是否能做出好的预测。他建议,这些数据可以来自自动化实验室,这些实验室可设置为以标准化的方式生成特定类型的数据。参考文献:Ash, J. R. et al. Preprint at ChemRxiv Fraser, J. S. & Murcko, M. A. Cell 187, 517–520 (2024).Heyndrickx, W. et al. J. Chem. Inf. Model. 64, 2331–2344 (2024).Fu, Y. et al. Nature Biotechnol. https://doi-org.libproxy1.nus.edu.sg/10.1038/s41587-024-02503-w (2024).
放射疗法
2025-04-15
Collaboration will support access of an innovative treatment developed for numerous aggressive cancers heavily influenced by metabolic pathways
ATHENS, Greece and SAN DIEGO, CA, USA I April 15, 2025 I
Er-Kim Pharmaceuticals
, an international company specializing in the commercialization of novel therapies for pharmaceutical and biopharmaceutical companies, today announced it has signed a distribution agreement with
Polaris Pharmaceuticals
to commercialize Pegargiminase (ADZODI) across 36 markets in the EMEA region. Pegargiminase is an enzyme-based cancer drug that breaks down the amino acid arginine, which cancer cells need to grow.
An aggressive and rare form of cancer, Malignant Pleural Mesothelioma (MPM) is caused by asbestos exposure. Combined with chemotherapy, Pegargiminase has the ability to restrict the body from producing a certain amino acid that fuels mesothelioma cancer growth.
Under the agreement, Er-Kim is appointed as the exclusive partner for pegargiminase in certain countries across Central & Eastern Europe, Eurasia, North Africa and Mediterranean regions.
Cem Zorlular, Chief Executive Officer of Er-Kim expressed his anticipation for working with Polaris and the local healthcare community to make Pegargiminase (ADZODI) accessible shortly after its initial approval in the US. He stated, “We are delighted to collaborate with Polaris to make this vital drug available to patients with limited treatment options for cancers like Malignant Pleural Mesothelioma (MPM) and to support these patients’ quality of life.”
“We are delighted to partner with Er-Kim and expand the reach of Pegargiminase (ADZODI) in these markets. This partnership unlocks the significant unmet need for access to life-altering cancer treatments and enables a substantial number of patients in multiple EMEA markets access to this novel product for various cancer treatments like Malignant Pleural Mesothelioma (MPM),” commented Dr. Steve Hsu, Chief Executive Officer of Polaris Pharmaceuticals.
About Er-Kim Pharmaceuticals
Established in 1981, Er-Kim stands at the forefront of biopharmaceutical innovation, partnering with over 40 global leaders to revolutionize patient care in key international markets. Our pioneering business models, tailored for sustainability and flexibility, have positioned us as a full-service solution, extending our reach to over 600 million patients through our fully-owned affiliates. With a dedicated team of over 280 professionals worldwide and revenues exceeding EUR 260M, Er-Kim is not just a partner but a trailblazer in healthcare, continually setting new standards in commercialization and patient access. For more information, please visit
http://www.er-kim.com/
.
About Polaris
Polaris Group is a biopharmaceutical company dedicated to pioneering advanced therapies, primarily focusing on metabolic-related diseases. Our lead drug candidate, Pegargiminase (ADZODI), is presently advancing through the BLA-enabling stage for MPM and clinical development for other indications. Pegargiminase is a biologic in late-stage clinical development for a wide range of cancers, including hepatocellular carcinoma, soft tissue sarcoma, glioblastoma, non-small cell lung cancer, melanoma, acute myeloid leukemia and others. Pegargiminase is designed to disrupt cancer cell metabolism, providing a novel approach to treating a wide range of cancers heavily influenced by metabolic pathways. Our mission is to revolutionize the treatment of complex diseases like cancer by concentrating on their metabolic foundations, ultimately striving to enhance patient outcomes globally. (
https://www.polarispharma.com
)
SOURCE:
Polaris Group
引进/卖出上市批准
2025-03-23
中华医学会肝病学分会肝炎学组和中华肝脏病杂志编辑委员会于2024年6月发表了《加速消除乙型肝炎病毒感染:扩大预防和治疗专家建议》(下称《专家建议》),对于包括慢乙肝全人群筛查、成人乙型肝炎疫苗接种、乙型肝炎病毒(HBV)DNA定量值的评价、启动抗病毒治疗的丙氨酸转氨酶(ALT)阈值、“不确定期”患者的治疗等《2022版乙肝防治指南》未达成共识的亟需解决的热点、难点问题进行了梳理,结合全球研究进展,提出建议。该建议旨在通过进一步扩大乙型肝炎的预防和治疗,早日实现世界卫生组织提出的“2030年消除病毒性肝炎作为公共卫生危害”的目标。本文就《专家建议》的要点进行介绍和解读,指导临床医生加强乙型肝炎的筛、诊、治、管。
1 一般人群HBV感染筛查、检测和管理
HBV本身不直接造成肝细胞损伤,而且肝脏本身再生及代偿功能较强,因此慢性HBV感染者一般不会出现明显的临床表现、肝功能可能长期在正常范围内。因此,慢性HBV感染的诊断主要依靠血清学和病毒学检测。根据Polaris发布的中国消除乙型肝炎进展数据,中国慢性HBV感染人数为7974.2万,诊断率仅仅为24%,治疗率更低,仅仅为15%。扩大人群筛查是实现早期诊断和及时治疗的关键措施之一。《专家建议》提出,对于≥18岁人群一生至少检测1次;持续暴露危险因素的高危人群应定期检测;检测项目包括乙型肝炎表面抗原(HBsAg)、乙型肝炎表面抗体(抗-HBs)和乙型肝炎核心抗体(抗-HBc)3项指标。
筛查后的临床管理也至关重要。筛查后临床管理包括诊断、疾病严重程度评估和抗病毒治疗。与现行HBV筛查策略比较,普遍筛查联合筛查后50%临床管理,到2030年,新发肝细胞癌(HCC)将减少7.3%,慢性乙型肝炎死亡将减少8.5%,累积HBV相关死亡将减少5%。《专家建议》提出,筛查结果HBsAg阳性者应进一步评估和治疗。特别指出,抗-HBs和抗-HBc同时阳性或单项抗-HBc阳性者,需进一步检测HBV DNA载量。3项均阴性者,建议接种乙肝疫苗。
2 成人乙型肝炎疫苗接种
以2013—2020年中国法定传染病报告系统中报告的乙肝病例为依据,对发病情况进行估算,2013—2020年中国估计急性乙肝发病率为4.6/10万,其中31~60岁发病占65.5%(2158/3297)。而且乙肝疫苗安全性高、可及性高。因此《专家建议》提出,建议无乙型肝炎疫苗接种史的≥18岁人群接种乙肝疫苗,特别是有乙肝高危因素的人群更应该接种;此外明确指出成人接种乙肝疫苗剂量及接种程序,首次接种后无应答人群应如何再次接种。
3 HBV DNA定量检测结果评价
检测HBV DNA应该采用高灵敏、具有更低检测下限(<10~20 kU/L)、更广线性范围(10~108~9 kU/L)的检测方法,以及时发现低病毒载量患者给予及时治疗,或及时发现治疗效果不佳患者及时给予调整治疗策略。HBV DNA定量检测试剂有的检测下限(LLOD)和定量下限(LLOQ)不同,简单说前者的HBV DNA载量较后者更低。《专家建议》指出,判断疾病自然史分期、启动抗病毒治疗、判断抗病毒治疗效果等应用的HBV DNA值,均以LLOQ为标准,认为只有检测到HBV DNA定量值,方可定为阳性。
4 ALT正常值上限与治疗阈值
各大指南对ALT的正常值均有不同推荐,大多数建议男性ALT正常值为30 U/L、女性为19 U/L;2018年AASLD指南建议男性ALT正常值为35 U/L,女性为25 U/L;而EASL和APASL指南建议男女ALT正常值均为40 U/L。2015年APASL指南定义了正常高值ALT,为0.5~1倍的正常值上限(ULN)。由于正常高值ALT的慢性乙型肝炎患者,肝组织学病变比例更高、肝病相关不良结局发生率更高,因此《专家建议》提出以正常高值作为ALT治疗的阈值,扩大治疗人群,可显著改善这部分患者肝病长期预后。
5 HBsAg阴性的乙型肝炎肝硬化患者抗病毒治疗策略
Kim等对829例HBsAg清除的慢性HBV感染者的回顾性研究发现,经3464人年的随访,肝硬化患者HCC年发生率为2.85%,显著高于非肝硬化患者(0.29%)。《专家建议》指出,对于HBsAg阴性的乙型肝炎肝硬化患者,都应该继续抗病毒治疗,争取肝硬化逆转或再代偿。对于功能性治愈的乙肝肝硬化患者,应继续治疗至肝硬化逆转;隐匿性乙型肝炎肝硬化患者(血清或肝组织HBV DNA阳性),应立即开始抗病毒治疗;HBV Pre-S/S突变株感染导致的乙肝肝硬化患者,如HBV DNA检测阳性,建议立即治疗,如HBV DNA阴性,应肝活检后决定是否抗病毒治疗。
6 临床(功能性)治愈的优势人群
由于聚乙二醇干扰素(PegIFN)α相比于核苷类似物(NAs),不良反应相对较多,目前仍建议选择优势人群采用Peg-IFN α单药或联合治疗。目前中国很多研究探讨经治或初治慢乙肝患者Peg-IFN α治疗的临床治愈率,并推荐优势人群。“珠峰项目”5年数据报告,NAs经治的基线HBsAg≤500 kU/L慢乙肝患者,联合Peg-IFN α治疗至48周,HBsAg清除率为42.9%。“破冰项目”2年数据显示,初治乙型肝炎e抗原(HBeAg)阴性、ALT正常慢性HBV感染者,如基线HBV DNA<1000 kU/L,HBsAg<500 kU/L,Peg-IFN α治疗48周临床治愈率高达52.4%。基于此,《专家建议》推荐了临床治愈的优势人群。
7 “不确定期”的定义及其治疗策略
“不确定期”患者难以被自然史分期明确分期,主要包括不能明确区分HBeAg阳性慢性HBV感染者与HBeAg阳性慢性乙型肝炎(CHB)患者,以及不能明确区分HBeAg阴性HBV感染者与HBeAg阴性CHB患者。相较于真正的免疫耐受期或非活动期人群,这部分患者疾病进展风险相对较高,也可能需要抗病毒治疗。《专家建议》指出,HBeAg阳性“不确定期”患者,建议做肝活检,根据组织学改变或无创检测评估决定是否抗病毒治疗;HBeAg阴性“不确定期”患者,只要HBV DNA阳性,建议抗病毒治疗。
8 合并感染和并发症患者的抗病毒治疗
关于HBV感染者同时存在人类免疫缺陷病毒、丙型肝炎病毒、丁型肝炎病毒感染的情况,很多研究分析比较了单独感染和合并感染患者的不良临床结局的发生情况,研究结果提示合并其他病毒感染的HBV感染者肝功能更差、肝硬化及肝癌发生率更高。存在代谢相关危险因素的患者,包括肥胖、高血压病、高脂血症、糖尿病,代谢危险因素与HCC发生正相关。因此,《专家建议》提出,对于合并其他病毒感染及代谢相关危险因素的慢性HBV感染者,应积极抗病毒治疗。
除了以上8个部分的建议以外,《专家建议》推荐简化的慢乙肝治疗理念,优先评估HBV DNA和血清学指标,然后考虑ALT和患者年龄,再考虑家族史和疾病严重程度及进展风险,另外在抗病毒治疗的同时,要联合抗纤维化治疗。《专家建议》的目的在于成人进行普遍筛查,科学地指导未感染者乙型肝炎疫苗接种;对HBV感染者进行评估、治疗和长期随访管理,最大限度地让新版指南中关于扩大抗病毒治疗的理念得以惠及更多患者,让符合适应证的患者尽早启动治疗,向乙型肝炎全治迈进一大步。
相关阅读
23%乙肝患者达到临床治愈!NEJM:侯金林领衔新疗法,探索停药后持续“清除”病毒
中国乙肝患者约7500万!《柳叶刀》子刊:约3000万人不知晓已感染
《柳叶刀》子刊:停药后持续“清除”乙肝感染24周,创新药助力功能性治愈
全球乙肝感染者,65%在亚太地区!《自然》子刊:关注8大关键策略
向治愈乙肝进发!95%中国患者需考虑抗病毒治疗,4类人群应尽快治疗
欢迎投稿:学术成果、前沿进展、临床干货等主题均可,点此了解投稿详情。
免责声明:药明康德内容团队专注介绍全球生物医药健康研究进展。本文仅作信息交流之目的,文中观点不代表药明康德立场,亦不代表药明康德支持或反对文中观点。本文也不是治疗方案推荐。如需获得治疗方案指导,请前往正规医院就诊。
分享,点赞,在看,传递医学新知
疫苗临床研究
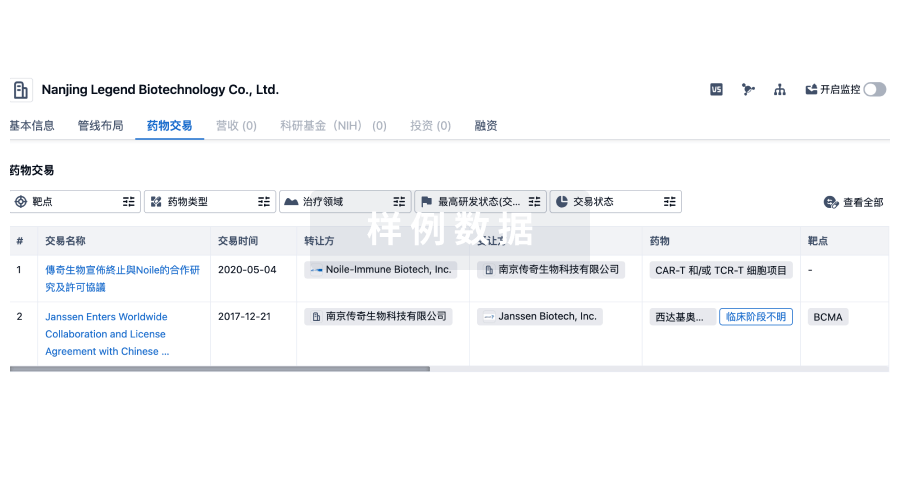
100 项与 Polaris Inc. 相关的药物交易
登录后查看更多信息
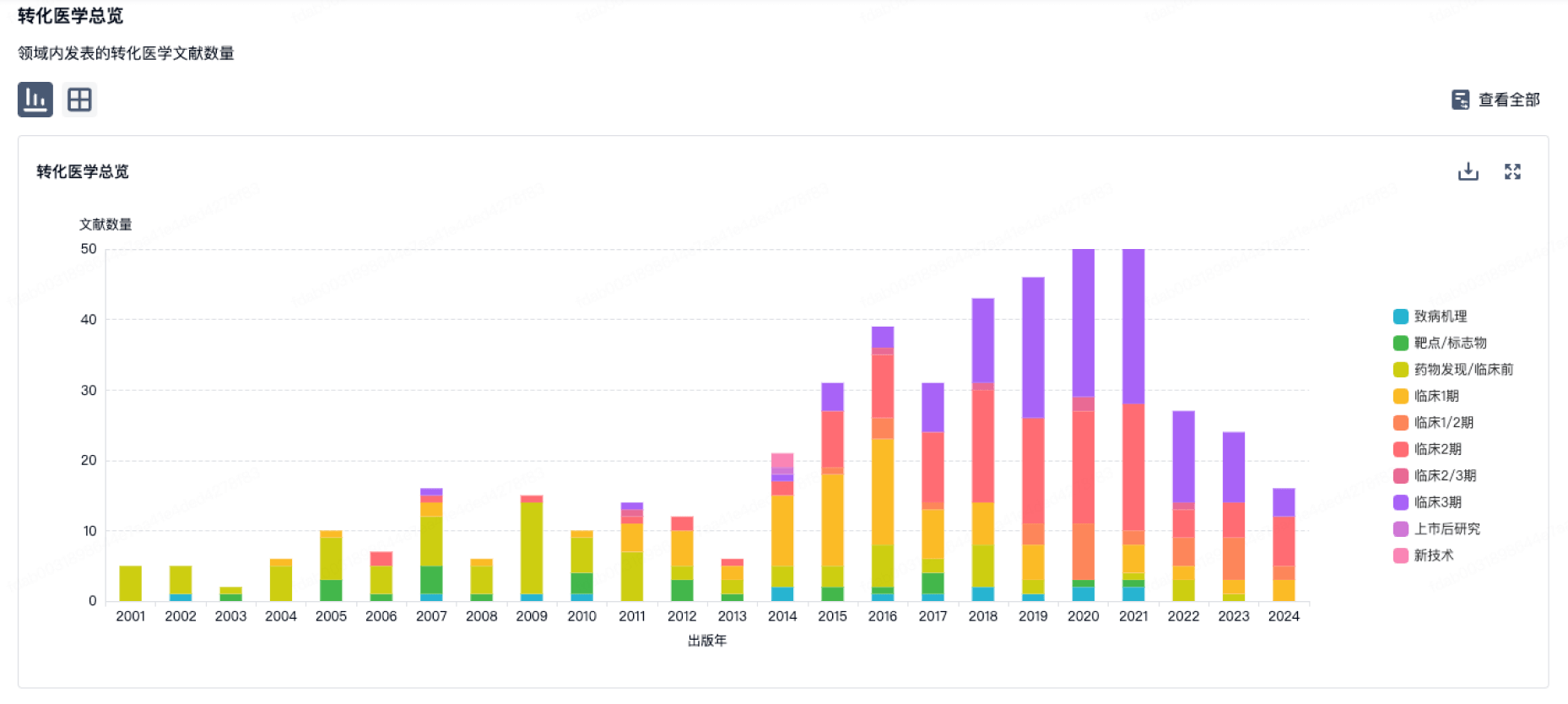
100 项与 Polaris Inc. 相关的转化医学
登录后查看更多信息
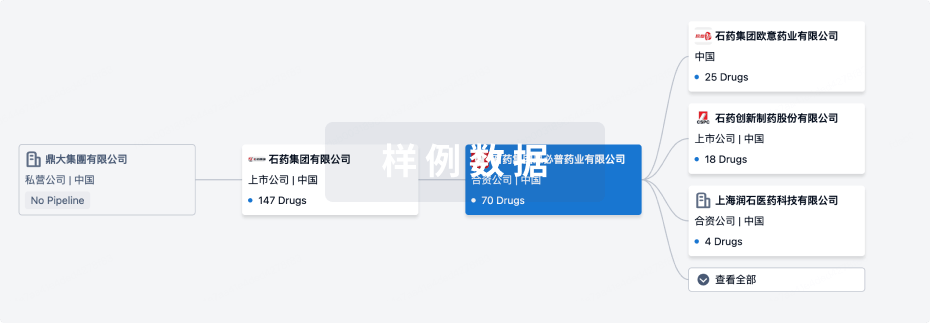
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年08月30日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
临床2期
1
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
聚乙二醇化重组假丝酵母尿酸氧化酶(Polaris) ( Uric acid ) | 肿瘤溶解综合征 更多 | 临床2期 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
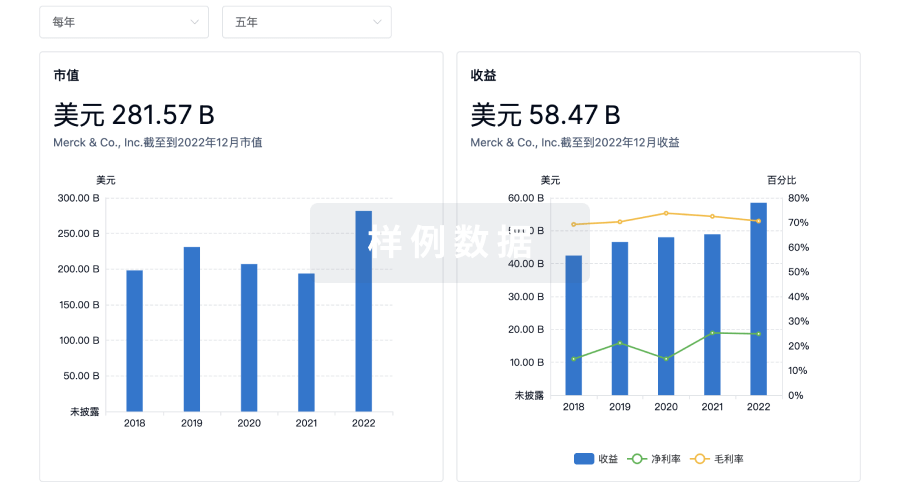
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
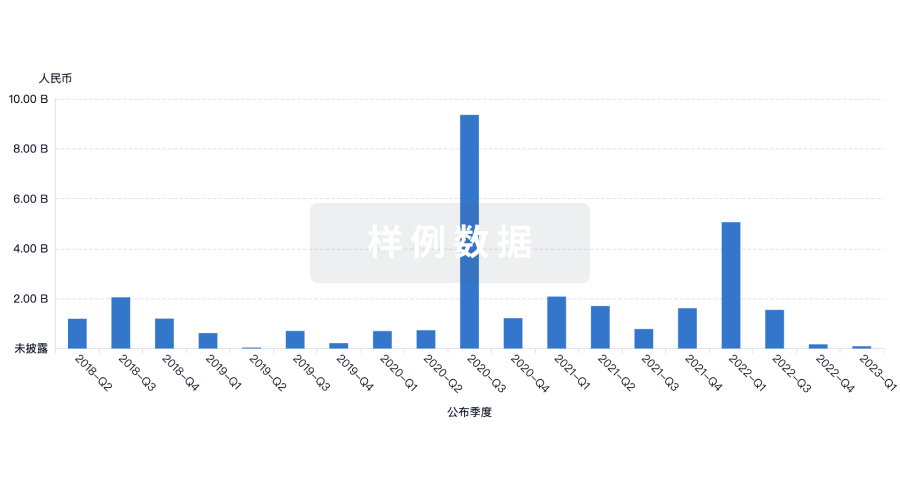
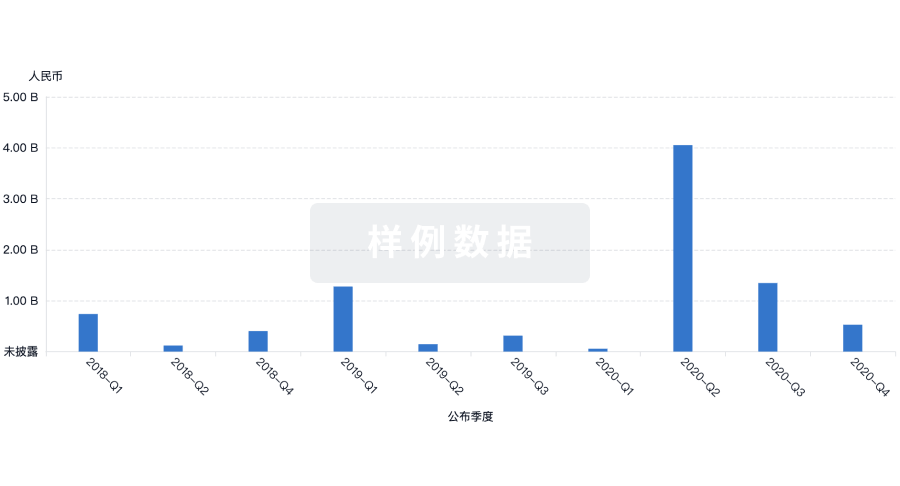
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用