预约演示
更新于:2025-01-23
Fortis Jessa Ram Hospital
India
India
更新于:2025-01-23
概览
关联
177
项与 Fortis Jessa Ram Hospital 相关的临床试验NCT06746168
Infiltration of Local Anesthetics Between the Popliteal Artery and Capsule of the Knee (iPACK) with Femoral Triangle Block (TFB) Versus Surgical Local Infiltration Analgesia (LIA) in Unilateral Total Knee Arthroplasty (TKA): a Multicenter Double-blind, Prospective Randomized Controlled Study.
The goal of this study is to compare the anesthetic combination iPACK with femoral triangle block versus surgical LIA for unilateral TKA. We hypothesize that an iPACK block with femoral triangle block is non-inferior to surgical LIA. Furthermore, due to visualization of the relevant neural and vascular structures, the risk of accidental popliteal block, nerve damage or LAST with (a blindly performed) LIA could theoretically be reduced.
开始日期2025-01-10 |
申办/合作机构 |
NCT06734546
The Effect of Exercise of High Vs. Moderate Intensity on the Brain in Type 2 Diabetes
The goal of this clinical trial is to learn if exercise training of high or moderate intensity is most optimal to improve brain health and prevent neurodegeneration in type 2 diabetes patients. The main question it aims to answer is:
What is the effect of exercise training of high vs. moderate intensity on brain metabolism, brain perfusion, and cognition in type 2 diabetes?
Researchers will compare the exercise training groups to a control group without exercise training to determine the effect of exercise training on the brain in type 2 diabetes.
Participants will exercise for 6 months, 3 times per week. Before and after these 6 months, they will undergo:
* a brain MRI scan
* cognitive tests
* blood sampling
What is the effect of exercise training of high vs. moderate intensity on brain metabolism, brain perfusion, and cognition in type 2 diabetes?
Researchers will compare the exercise training groups to a control group without exercise training to determine the effect of exercise training on the brain in type 2 diabetes.
Participants will exercise for 6 months, 3 times per week. Before and after these 6 months, they will undergo:
* a brain MRI scan
* cognitive tests
* blood sampling
开始日期2024-11-08 |
申办/合作机构  Hasselt University Hasselt University [+3] |
NCT05598385
Groin Complications in Open Vs. Percutaneous Peripheral Cannulation for Cardiopulmonary Bypass in Minimally Invasive Cardiac Surgery
The aim of this randomized trial is to investigate the groin complications in open vs percutaneous peripheral cannulation for cardiopulmonary bypass in minimally invasive cardiac surgery
开始日期2024-11-01 |
申办/合作机构 |
100 项与 Fortis Jessa Ram Hospital 相关的临床结果
登录后查看更多信息
0 项与 Fortis Jessa Ram Hospital 相关的专利(医药)
登录后查看更多信息
1
项与 Fortis Jessa Ram Hospital 相关的新闻(医药)2024-04-02
SABIC has demonstrated the feasibility of recycling used medical plastic back into the medical materials stream. The project was initiated together with the dialysis department at Jessa Hospital.
Serving as a pilot proof-of-concept, used medical plastic generated at Jessa’s hospitals was converted to pyrolysis oil in a recycling process, delivering circular feedstock for SABIC’s production of TRUCIRCLE polymers in medical grade quality with same performance, purity and physiological safety as virgin-based medical grade polymers.
Lada Kurelec, general manager, polymers technology & innovation at SABIC, said: “Working with Jessa Hospital has been an immensely rewarding experience, where we learned how individual belief in circularity can mobilise industry to work together. I value how this collaboration enabled creation of an ecosystem to collect and recycle non-contaminated medical waste in a very short time. Thanks to this collaboration, we are creating a certified circular TRUCIRCLE polymer portfolio able to serve the healthcare market. We are inviting other players in the value chain to join us and Jessa in this ground-breaking initiative to accelerate the circularity of plastics in the medical industry.”
Advanced recycling technology and the vast experience gained through its TRUCIRCLE solutions put SABIC in a strong position to provide a circular solution designed to help Jessa Hospital reduce the environmental footprint of its medical products by avoiding their incineration after use. Approximately 85% of the used medical plastic generated at the hospital is not contaminated and therefore requires no specialised treatment. This allows it to be repurposed as feedstock for advanced recycling and subsequent production of high-quality medical grade polymers, saving virgin raw material and contributing to a more circular medical economy.
Karl Zwinnen, project engineer at Jessa said: “We are very pleased with the advanced and circular recycling approach enabled by SABIC to improve our medical waste management. The setup of an efficient collection system for used medical plastic has met with strong support among our medical and healthcare staff. Besides contributing to enhanced sustainability and circularity, the solution also has an enormous potential for reducing our disposal costs. We look forward to implementing it across all Jessa locations.”
As a result of this successful pilot project, SABIC is currently in the process of actively engaging partners to scale up operations and create a fully closed-loop recycling model for used medical plastic in larger volumes.
SABIC’s certified circular materials are produced using mass balance accounting according to the International Sustainability & Carbon Certification (ISCC) PLUS program, which defines a set of transparent rules for tracking the material flow across complex supply chains from the feedstock to final applications. The resulting certified circular polymers form part of the company’s TRUCIRCLE portfolio and services.
SABIC’s TRUCIRCLE portfolio and services include certified circular polymers as well as design for recyclability, mechanically recycled products, certified renewable polymers from bio-based feedstock, and closed loop initiatives to recycle plastic back into high-quality applications and help prevent valuable used plastics from becoming waste.
100 项与 Fortis Jessa Ram Hospital 相关的药物交易
登录后查看更多信息
100 项与 Fortis Jessa Ram Hospital 相关的转化医学
登录后查看更多信息
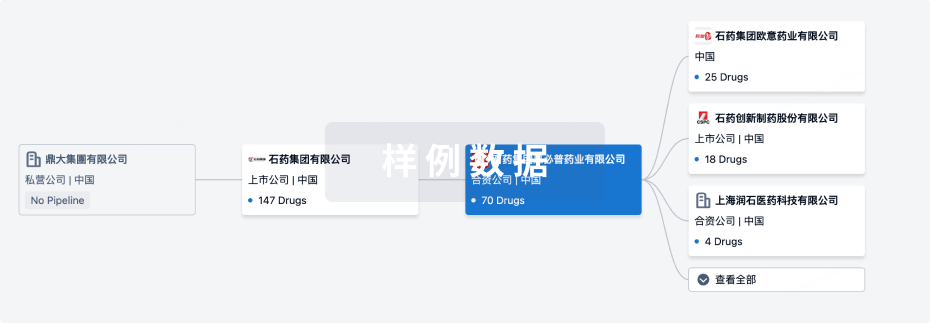
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年04月26日管线快照
无数据报导
登录后保持更新
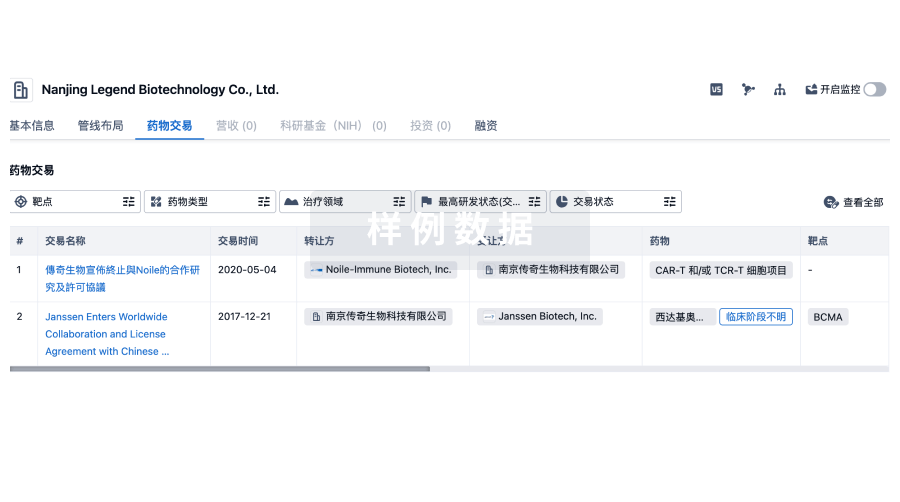
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
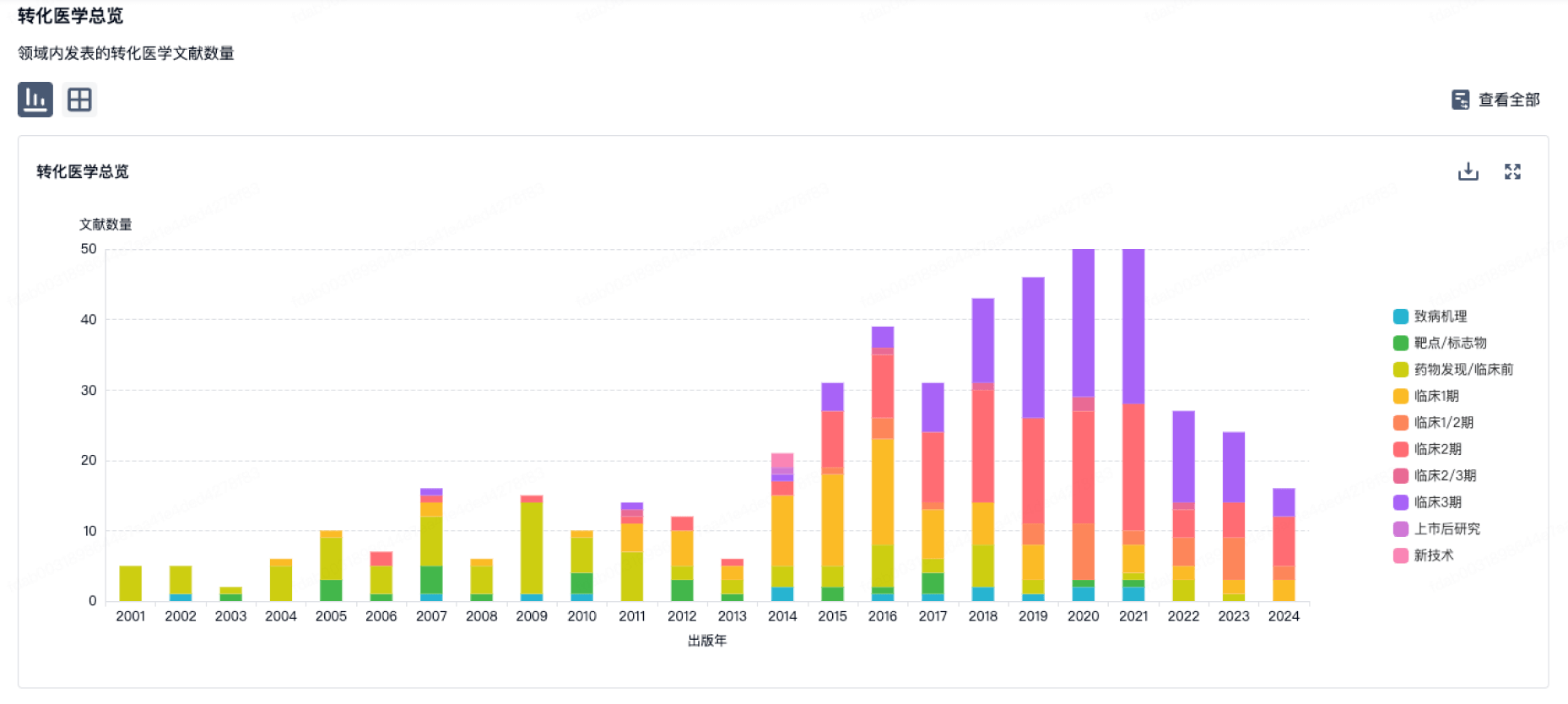
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
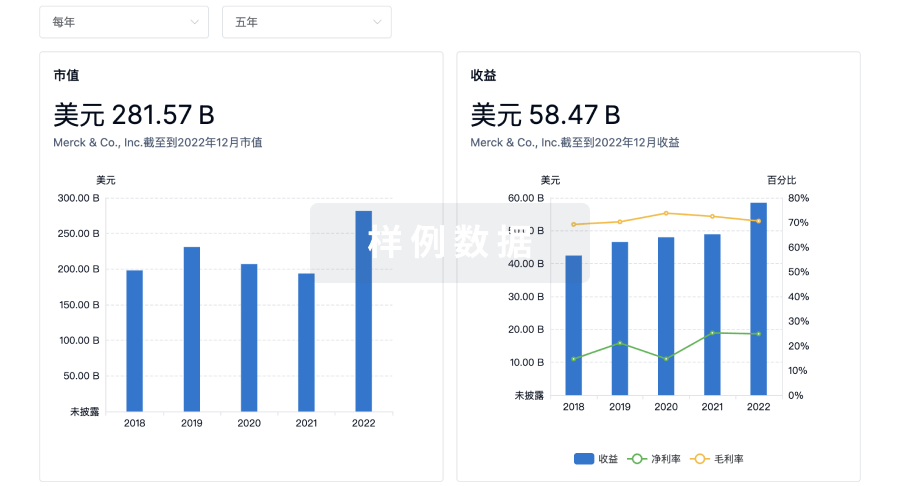
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

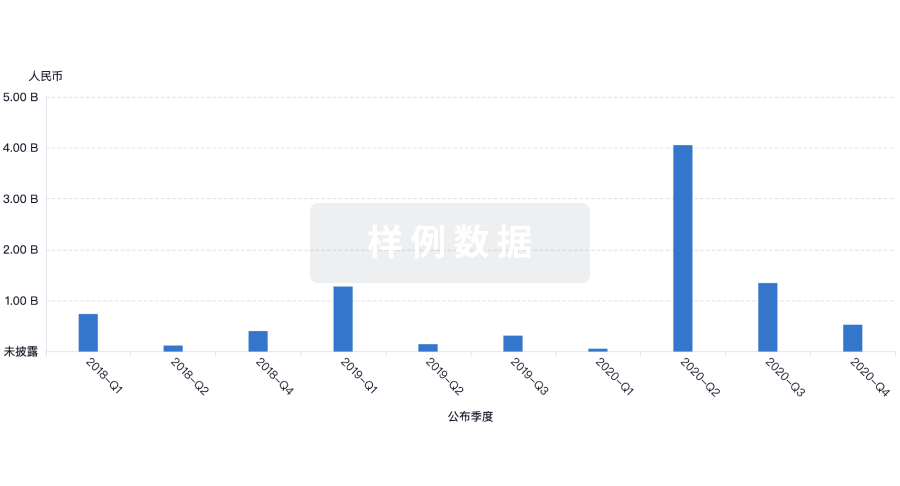
投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
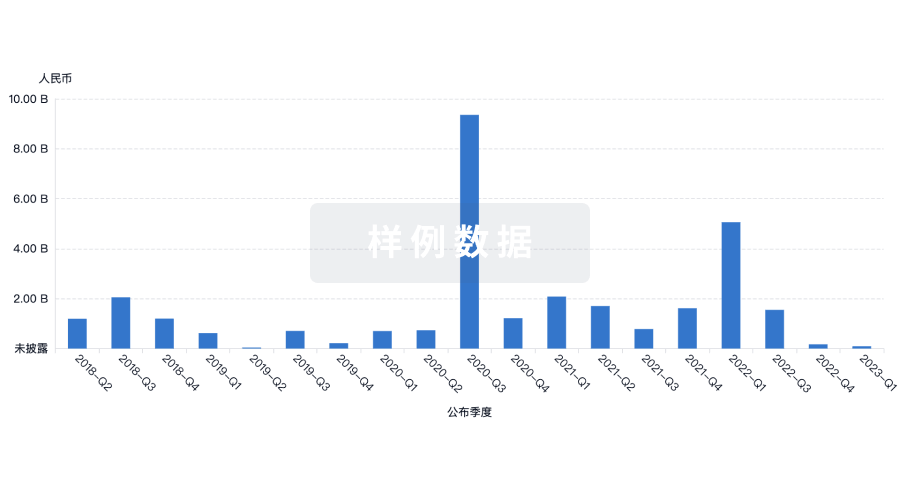
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
来和Eureka LS聊天吧
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用