更新于:2024-11-04
Cryopraxis Criobiologia Ltda.
更新于:2024-11-04
概览
关联
3
项与 Cryopraxis Criobiologia Ltda. 相关的临床试验Clinical study to evaluate the safety and tolerability of intravenous infusion of plasma from human umbilical cord and placental blood (Plasmacord®) in patients with Severe Acute Respiratory Syndrome resulting from Sars-Cov-2 infection
开始日期2020-07-27 |
申办/合作机构 |
Phase I Study of a Filler Agent Composed of Mesenchymal Stem Cells Obtained From Autologous Adipose Tissue Associated With Hyaluronic Acid
Lipodystrophies are part of a clinically heterogeneous group of disorders characterized by loss (lipoatrophies) and / or accumulation of fat, which usually results in a change of normal tissue surface. Millions of plastic and reconstructive surgeries are performed annually to repair soft tissue defects due to trauma, tumor resection and congenital defects. Surgical options for lipoatrophy, the lipodystrophy type characterized by subcutaneous adipose tissue atrophy, include: Transfer of autologous fat, Dermis - fat graft, Skin flaps and Commercially available fillers.
Currently, the most commonly filler agent used for the lipodystrophy treatment is polymethylmethacrylate, considered permanent and with a history of short- and medium-term adverse effects. Biocompatible and temporary filler agents such as hyaluronic acid, polylactic acid and collagen have been used for over 25 years for cosmetic purposes and in lipoatrophies. More recently, the use of autologous fibroblasts proved to be efficient solving acne scars and enabling dermis regeneration. Studies in mice showed that the combination of pre - adipocytes with a biomaterial is much more effective in tissue reconstitution than the injection of adipose tissue only, providing volume and also stimulating cell proliferation and differentiation with increased production of extracellular matrix.
This project aims a phase I clinical trial of a filler agent, composed of mesenchymal stem cells derived from autologous adipose tissue associated with hyaluronic acid.
Currently, the most commonly filler agent used for the lipodystrophy treatment is polymethylmethacrylate, considered permanent and with a history of short- and medium-term adverse effects. Biocompatible and temporary filler agents such as hyaluronic acid, polylactic acid and collagen have been used for over 25 years for cosmetic purposes and in lipoatrophies. More recently, the use of autologous fibroblasts proved to be efficient solving acne scars and enabling dermis regeneration. Studies in mice showed that the combination of pre - adipocytes with a biomaterial is much more effective in tissue reconstitution than the injection of adipose tissue only, providing volume and also stimulating cell proliferation and differentiation with increased production of extracellular matrix.
This project aims a phase I clinical trial of a filler agent, composed of mesenchymal stem cells derived from autologous adipose tissue associated with hyaluronic acid.
开始日期2015-03-01 |
Phase II Study of Intramyocardial Injection of Autologous Bone Marrow Stem Cells for Refractory Angina in Patients With Normal or Slightly Reduced Left Ventricular Function.
Therapeutic neovascularization is an innovative strategy for cardiac tissue recovery due to chronic, intense ischemia. Thus stem cell therapy has become a promising procedure for the large number of patients with refractory angina due to coronary disease, despite of the use of multiple anti-angina medications, remain severely symptomatic with disabling angina.
Stem cell therapy using autologous cells from the patient's bone marrow, has been shown to be safe and associated with improved myocardial perfusion, reducing the symptoms of advanced coronary artery disease and increasing the functional capacity of patients whose therapeutic armamentarium available today has been exhausted.
The study hypothesis was that the infusion of autologous mononuclear cells derived from the patient's bone marrow and delivered via intramyocardial injection in patients with refractory angina and normal or slightly depressed ventricular function, promote improvement in the anginal symptoms and myocardial perfusion by the inducing neoangiogenesis.
Stem cell therapy using autologous cells from the patient's bone marrow, has been shown to be safe and associated with improved myocardial perfusion, reducing the symptoms of advanced coronary artery disease and increasing the functional capacity of patients whose therapeutic armamentarium available today has been exhausted.
The study hypothesis was that the infusion of autologous mononuclear cells derived from the patient's bone marrow and delivered via intramyocardial injection in patients with refractory angina and normal or slightly depressed ventricular function, promote improvement in the anginal symptoms and myocardial perfusion by the inducing neoangiogenesis.
开始日期2005-07-01 |
申办/合作机构 |
100 项与 Cryopraxis Criobiologia Ltda. 相关的临床结果
登录后查看更多信息
0 项与 Cryopraxis Criobiologia Ltda. 相关的专利(医药)
登录后查看更多信息
3
项与 Cryopraxis Criobiologia Ltda. 相关的文献(医药)2019-07-03·Gynecological endocrinology : the official journal of the International Society of Gynecological Endocrinology4区 · 医学
Hormonal oral contraceptive influence on isolation, Characterization and cryopreservation of mesenchymal stem cells from menstrual fluid
4区 · 医学
Article
作者: Coimbra, Anna Carolina ; Santamaria, Xavier ; Machado, Janaína J. dos Santos ; Baracat, Edmund Chada ; Haddad, Jorge Milhem ; Fiorelli-Arazawa, Lilian Renata ; Nicola, Maria Helena ; Soares, José Maria
The purpose of the study was to evaluate whether the intake of hormonal oral contraceptive influences the viability of mesenchymal stem cell. Sixteen healthy female volunteers with regular menstrual cycles were invited to participate. Menstrual fluid was collected on the day of maximum flux, and collected cells were analyzed by a 'minimal standard' for MSC characterization: plastic adherence, trilineage (adipogenic, osteogenic, chondrogenic) in vitro differentiation and a minimalistic panel of markers assessed by flow cytometry (CD731, CD901, CD1051, CD34-, CD45-) using monoclonal antibodies. The participants were divided into two groups: Group 1 - no hormonal contraceptive use; Group 2 - hormonal oral contraceptive use. The median of the menstrual fluid volume was 5.0 and the median number of cells was 5.2 × 106. Median of cell viability was 89.3%. After culture, mesenchymal stem cells increased from 0.031% of the total cells to 96.9%. The cells formed clusters and reached confluence after 15-21 days of culture in the first passage. In the second passage, clusters and the confluence were observed after 3 days of culture. No difference was observed between the groups. Our data suggest that oral hormonal contraceptive intake maintains the viability of mesenchymal stem cells from menstrual fluid.
2015-06-01·Cell transplantation3区 · 医学
Long-Term and Sustained Therapeutic Results of a Specific Promonocyte Cell Formulation in Refractory Angina: ReACT®(Refractory Angina Cell Therapy) Clinical Update and Cost-Effective Analysis
3区 · 医学
ArticleOA
作者: Branco, João Nelson Rodrigues ; Goldenberg, Regina Coeli Dos Santos ; Azevedo, Silvia ; Machado, Janaina ; De Siqueira Mac Dowell Coimbra, Anna Carolina Teixeira ; Miller, Leslie W. ; Buffolo, Enio ; Sanberg, Paul R. ; De Oliveira, José Salvador Rodrigues ; Regazzi, Germana ; Invitti, Adriana Luckow ; Stolf, Noedir Antonio Groppo ; Nelson, Americo Hossne ; Cruz, Eduardo
Mononuclear stem cells have been studied for their potential in myocardial ischemia. In our previous published article, ReACT®phase I/II clinical trial, our results suggest that a certain cell population, promonocytes, directly correlated with the perceived angiogenesis in refractory angina patients. This study is ReACT's clinical update, assessing long-term sustained efficacy. The ReACT phase IIA/B noncontrolled, open-label, clinical trial enrolled 14 patients with refractory angina and viable ischemic myocardium, without ventricular dysfunction, who were not suitable for myocardial revascularization. The procedure consisted of direct myocardial injection of a specific mononuclear cell formulation, with a certain percentage of promonocytes, in a single series of multiple injections (24—90; 0.2 ml each) into specific areas of the left ventricle. Primary endpoints were Canadian Cardiovascular Society Angina Classification (CCSAC) improvement at the 12-month follow-up and ischemic area reduction (scintigraphic analysis) at the 12-month follow-up, in correlation with ReACT's formulation. A recovery index (for patients with more than 1 year follow-up) was created to evaluate CCSAC over time, until April 2011. Almost all patients presented progressive improvement in CCSAC beginning 3 months ( p = 0.002) postprocedure, which was sustained at the 12-month follow-up ( p = 0.002), as well as objective myocardium ischemic area reduction at 6 months (decrease of 15%, p < 0.024) and 12 months (decrease of 100%, p < 0.004) The recovery index ( n = 10) showed that the patients were graded less than CCSAC 4 for 73.9 ± 24.2% over a median follow-up time of 46.8 months. After characterization, ReACT's promonocyte concentration suggested a positive correlation with CCSAC improvement ( r = −0.575, p = 0.082). Quality of life (SF-36 questionnaire) improved significantly in almost all domains. Cost-effectiveness analysis showed decrease in angina-related direct costs. Refractory angina patients presented a sustained long-term improvement in CCSAC and myocardium ischemic areas after the procedure. The long-term follow-up and strong improvement in quality of life reinforce effectiveness. Promonocytes may play a key role in myocardial neoangiogenesis. ReACT dramatically decreased direct costs.
2009-12-01·Cell transplantation3区 · 医学
Refractory Angina Cell Therapy (ReACT) Involving Autologous Bone Marrow Cells in Patients without Left Ventricular Dysfunction: A Possible Role for Monocytes
3区 · 医学
ArticleOA
作者: Hossne, Nelson Americo ; Invitti, Adriana Luckow ; Azevedo, Silvia ; Stolf, Noedir Groppo ; Sanberg, Paul R. ; de Oliveira, Jose Salvador Rodrigues ; Buffolo, Enio ; Cruz, L. Eduardo
Autologous bone marrow mononuclear cell (BMMC) transplantation has emerged as a potential therapeutic option for refractory angina patients. Previous studies have shown conflicting myocardium reperfusion results. The present study evaluated safety and efficacy of CellPraxis Refractory Angina Cell Therapy Protocol (ReACT), in which a specific BMMC formulation was administered as the sole therapy for these patients. The phase I/IIa noncontrolled, open label, clinical trial, involved eight patients with refractory angina and viable ischemic myocardium, without left ventricular dysfunction and who were not suitable for conventional myocardial revascularization. ReACT is a surgical procedure involving a single series of multiple injections (40–90 injections, 0.2 ml each) into ischemic areas of the left ventricle. Primary endpoints were Canadian Cardiovascular Society Angina Classification (CCSAC) improvement at 18 months follow-up and myocardium ischemic area reduction (assessed by scintigraphic analysis) at 12 months follow-up, in correlation with a specific BMMC formulation. Almost all patients presented progressive improvement in angina classification beginning 3 months ( p = 0.008) postprocedure, which was sustained at 18 months follow-up ( p = 0.004), as well as objective myocardium ischemic area reduction at 12 months (decrease of 84.4%, p < 0.004). A positive correlation was found between monocyte concentration and CCSAC improvement ( r = −0.759, p < 0.05). Improvement in CCSAC, followed by correlated reduction in scintigraphic myocardium ischemic area, strongly suggests neoangiogenesis as the main stem cell action mechanism. The significant correlation between number of monocytes and improvement strongly supports a cell-related effect of ReACT. ReACT appeared safe and effective.
100 项与 Cryopraxis Criobiologia Ltda. 相关的药物交易
登录后查看更多信息
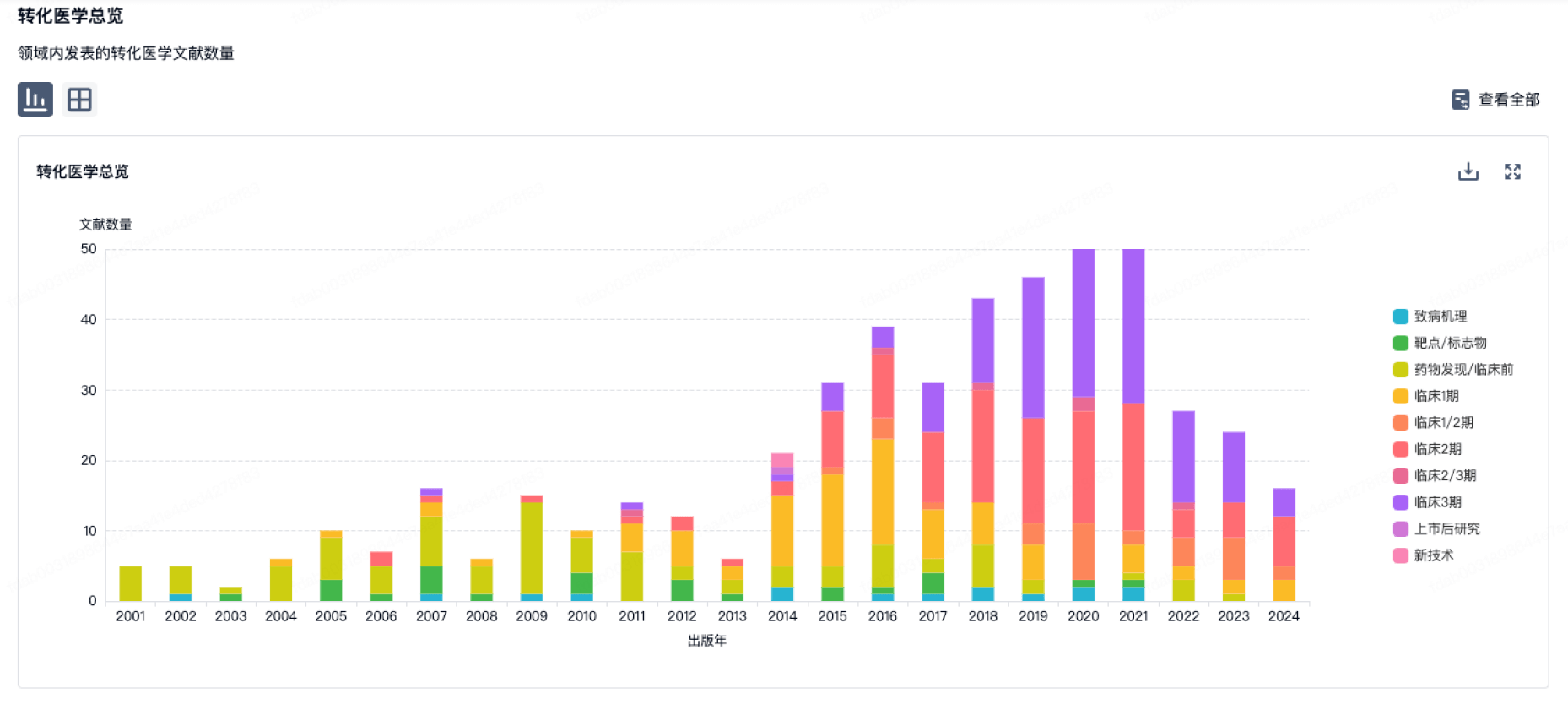
100 项与 Cryopraxis Criobiologia Ltda. 相关的转化医学
登录后查看更多信息
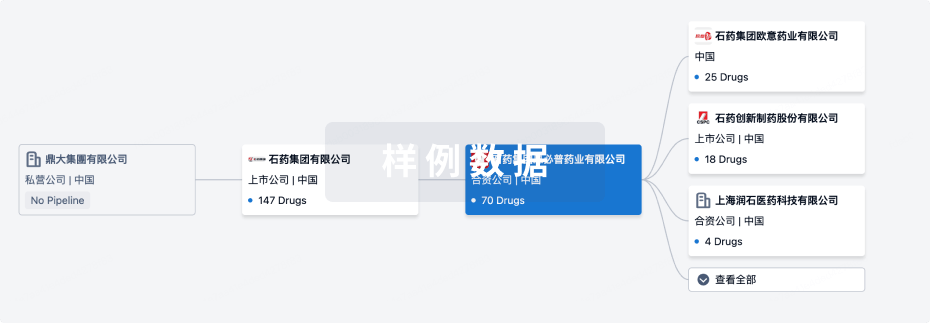
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2024年11月20日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
其他
1
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
Autologous stem cell therapy (CellPraxis/Cryopraxis) | 心绞痛 更多 | 无进展 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或

转化医学
使用我们的转化医学数据加速您的研究。
登录
或
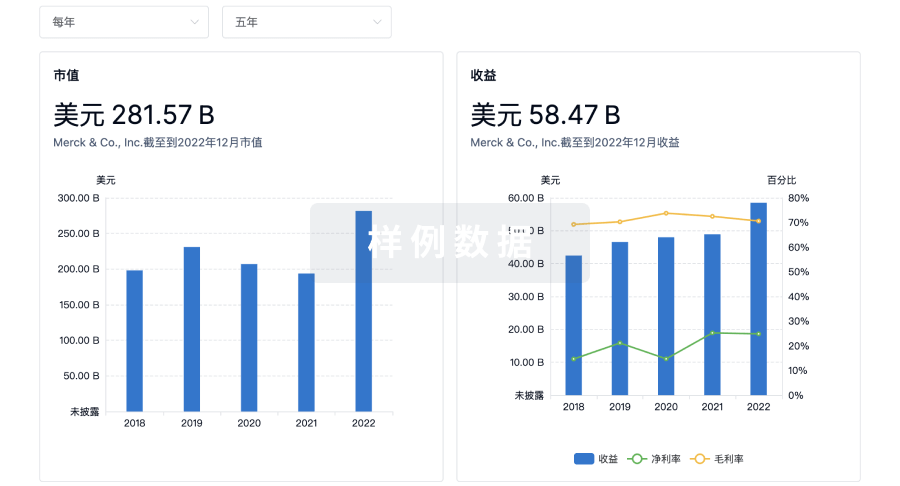
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或

融资
发掘融资趋势以验证和推进您的投资机会。
登录
或

标准版
¥16800
元/账号/年
新药情报库 | 省钱又好用!
立即使用
来和芽仔聊天吧
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用