预约演示
更新于:2025-09-09
Le Centre Hospitalier Universitaire de Toulouse
更新于:2025-09-09
概览
标签
内分泌与代谢疾病
消化系统疾病
血液及淋巴系统疾病
小分子化药
放射与诊断药物
合成多肽
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 小分子化药 | 1 |
| 放射与诊断药物 | 1 |
| 合成多肽 | 1 |
| 腺相关病毒基因治疗 | 1 |
| 单克隆抗体 | 1 |
关联
5
项与 Le Centre Hospitalier Universitaire de Toulouse 相关的药物作用机制 APLNR激动剂 [+1] |
非在研适应症- |
最高研发阶段临床1期 |
首次获批国家/地区- |
首次获批日期- |
US20220304965
专利挖掘靶点 |
作用机制- |
非在研适应症- |
最高研发阶段药物发现 |
首次获批国家/地区- |
首次获批日期- |
WO2024146880
专利挖掘靶点 |
作用机制- |
在研适应症 |
非在研适应症- |
最高研发阶段药物发现 |
首次获批国家/地区- |
首次获批日期- |
10
项与 Le Centre Hospitalier Universitaire de Toulouse 相关的临床试验CTIS2024-511821-75-00
- RC31/13/7030
开始日期2025-03-13 |
CTIS2022-501123-24-00
Pathophysiology of pain in Parkinson's disease: exploration of the serotonin system in positron emission tomography (PET [18F]-MPPF) - PD PAIN - RC31/21-0566
开始日期2024-06-10 |
CTIS2022-500879-31-00
- RC31/21/0610
开始日期2024-04-09 |
100 项与 Le Centre Hospitalier Universitaire de Toulouse 相关的临床结果
登录后查看更多信息
0 项与 Le Centre Hospitalier Universitaire de Toulouse 相关的专利(医药)
登录后查看更多信息
517
项与 Le Centre Hospitalier Universitaire de Toulouse 相关的文献(医药)2025-12-01·Current Osteoporosis Reports
Management of Bone Health in Adult Mastocytosis
Review
作者: Bulai Livideanu, Cristina ; Degboé, Yannick ; Maëva, Masson ; Alary, Pauline ; Laroche, Michel ; Nezzar, Coralie
Abstract:
Purpose of Review:
The present review will examine bone disease in mastocytosis, analyze the existing literature on its management, and propose a strategy for osteoporosis treatment in systemic mastocytosis. This strategy is based on both the available scientific evidence and the experience gained at our expert center (CEREMAST).
Recent Findings:
Systemic mastocytosis is a rare disorder, primarily affecting the bone and leading to osteoporosis, bone pain, and bone structural abnormalities. While traditionally described in indolent systemic mastocytosis, bone involvement is also observed in bone marrow mastocytosis. The true prevalence of systemic mastocytosis is likely underreported, highlighting the importance for clinicians to be familiar with the condition, particularly in cases of osteoporosis. Osteoporosis management typically involves bisphosphonates, with potential benefits from combining them with specific treatments like interferon in severe osteoporosis with vertebral fractures. The potential of new mast cell-targeting molecules to treat bone involvement needs to be demonstrated.
Summary:
This review provides a guide for osteoporosis and bone pain management in systemic mastocytosis.
2025-10-01·INTERNATIONAL JOURNAL OF CARDIOLOGY
Impact of Tafamidis on survival in elderly patients: Insights from the Healthcare European Amyloidosis Registry
Article
作者: Inamo, Jocelyn ; Broussier, Amaury ; Gellen, Barnabas ; Taieb, Charles ; Mouhat, Basile ; Zaroui, Amira ; Damy, Thibaud ; Bauer, Fabrice ; Roubille, François ; Piriou, Nicolas ; Jeanneteau, Julien ; Fraix, Antoine ; Dagrenat, Charlotte ; Eicher, Jean-Christophe ; Habib, Gilbert ; Donal, Erwan ; Jobbé-Duval, Antoine ; Bisson, Arnaud ; Margerit, Léa ; Trésorier, Romain ; Legallois, Damien ; Bouchot, Océane ; Delelis, François ; Lairez, Olivier ; Kharoubi, Mounira ; Réant, Patricia ; Gueffet, Jean-Pierre ; Charron, Phillipe ; Von Hunolestein, Jean-Jacques ; Courand, Pierre-Yves ; Costa, Jérôme ; Puscas, Tania
BACKGROUND:
Cardiac transthyretin amyloidosis (ATTR-CM) is a life-threatening cardiomyopathy. Tafamidis has been demonstrated to be an effective treatment. Our aim was to analyze clinical characteristics and survival of patients with ATTR-CM aged ≥80 years diagnosed after November 2018, treated with tafamidis 80/61 mg, and compare them with a non-treated group diagnosed before that date.
METHODS:
Data from the two groups were extracted from the Healthcare European Amyloidosis Registry (HEAR). Propensity score matching was used to adjust for baseline differences between the groups. Kaplan-Meier survival curves and Cox regression analyses were applied to assess survival outcomes.
RESULTS:
Out of 1380 patients, 1194 were treated with tafamidis 80/61 mg. Treated patients were significantly less severe at baseline, with a lower occurrence of NYHA class III-IV compared to the untreated group (24 vs. 46 %, p < 0.001). The median NT-proBNP at baseline was lower in the treated group (2330 vs. 4854 pg/ml, p < 0.001), as was the average level of high-sensitivity troponin T (55 vs. 74 ng/ml, p < 0.001), and the interventricular septal thickness (16 vs. 18 mm, p < 0.001). The 3-year survival rate for treated patients was 57 %, and 40 % for untreated patients. In the treated group, the 3-year survival rate was 68 % for patients aged 80-85 years and 58 % for those over 85 years. Survival rates were confirmed after propensity score analyses.
CONCLUSIONS:
This study demonstrates that tafamidis provides significant survival benefits for elderly patients with ATTR-CM, even in those over 85 years old. The findings emphasize the importance of early diagnosis and treatment.
2025-10-01·European Journal of Emergency Medicine
Guideline adhesion in the management of severe acute pulmonary oedema: a French survey involving 1048 cardiologists, emergency physicians, and intensivists
Article
作者: Delmas, Clément ; Angoulvant, Denis ; Chouihed, Tahar ; Aissaoui, Nadia ; Laribi, Saïd ; Puymirat, Étienne ; Muller, Grégoire ; Sauvage, Brice ; Danchin, Nicolas
Background and importance:
Acute pulmonary oedema is a frequent and potentially life-threatening emergency. Its management targets four key objectives: improving oxygenation, reducing volume overload, maintaining adequate blood pressure, and treating the underlying cause. Severe cases are mainly handled by cardiologists, emergency physicians, and intensivists, which may lead to variations in care and thus nonadherence to guidelines.
Objective:
To evaluate interspecialty differences in the management of patients with severe acute pulmonary oedema and compare physicians’ practices to 2021 European guidelines.
Design:
A national cross-sectional survey using clinical vignettes.
Settings and participants:
Four clinical vignettes, developed by a multidisciplinary scientific committee representing French cardiology, emergency medicine, and intensive care societies were distributed between June and September 2022 to physicians from the three specialties and to a panel of 20 experts.
Outcome measures and analysis:
The primary outcome was adherence to European guidelines. Interspecialty differences and predictors of nonadherence were assessed using univariate and multivariate analyses.
Main results:
A total of 1048 physicians responded (59% emergency physicians, 22% intensivists, and 19% cardiologists). Adherence rates were 66, 65, 69, and 76%, respectively among cardiologists, emergency physicians, intensivists, and experts. Intensivists and emergency physicians were more prone to initiate noninvasive ventilation than cardiologists (respectively 87, 82, and 71%, P < 0.001 and P < 0.01). Intensivists and cardiologists were more likely to intubate patients than emergency physicians (respectively 73, 65, and 43%, P < 0.001 for both comparisons). Cardiologists more frequently administered intravenous diuretics (98%) compared with emergency physicians and intensivists (both 90%, P = 0.002). Emergency physicians chose more frequently the correct door-to-balloon delay than cardiologists for ST-segment elevation myocardial infarction–related acute pulmonary oedema (43 versus 28%, P = 0.003). Multivariate analysis showed lower adherence among physicians compared with experts. Adherence was also lower among physicians older than 40 years and those working in nonuniversity hospitals.
Conclusions:
This nationwide survey highlights marked discrepancies between European guidelines and clinical practice in the management of acute pulmonary oedema, with substantial variation across specialties regarding initiation of oxygen therapy, invasive ventilation, nitrates, or delay for thrombolysis of an ST-segment elevation myocardial infarction.
1
项与 Le Centre Hospitalier Universitaire de Toulouse 相关的新闻(医药)2025-05-12
Novo Nordisk presented positive findings from a late-stage basket study of once-weekly Sogroya (somapacitan) at the joint congress of the European Society for Paediatric Endocrinology (ESPE) and the European Society of Endocrinology (ESE) on Monday, bolstering the growth hormone analogue’s label expansion filings in the US and EU for certain paediatric growth disorders.Specifically, Sogroya demonstrated clinical non-inferiority to once-daily Norditropin (somatropin) in pre-pubertal children born small for gestational age (SGA), or with Noonan syndrome (NS), or idiopathic short stature (ISS). The drug also showed superiority over Norditropin in children with NS and against lower doses of Norditropin in children born SGA.Highlighting the cumulative negative impact of regularly missing doses of growth hormone, Martin Lange, Novo’s executive VP for development, said: “We are committed to providing…therapies with flexibility in administration timing and missed doses, which may better suit the needs of children with growth failure.”The Phase III REAL8 trial — part of the broader REAL programme — employed a basket design to evaluate once-weekly Sogroya across four paediatric growth disorders — SGA, NS, ISS and Turner syndrome (TS). Children with NS, TS, or ISS were randomised to receive either weekly Sogroya or daily Norditropin, while those with SGA were assigned to Sogroya, or two different Norditropin doses — lower and higher than the standard dose.Results showed the study achieved its primary endpoints across three indications. In children born SGA, Sogroya demonstrated superior estimated mean height velocity compared with a lower dose of Norditropin (11.0 vs 9.4 cm/year) and non-inferior results compared with a higher dose (11.0 vs 11.1 cm/year). In children with NS, Sogroya showed superior results (10.4 vs 9.2 cm/year), while in those with ISS, it demonstrated non-inferiority (10.5 vs 10.5 cm/year) compared with Norditropin.Meanwhile, the weekly therapy showed no safety and tolerability issues compared with the daily formulation, with similar insulin-like growth factor 1 responses observed across treatment groups. Novo noted that based on the data from REAL8 and another ongoing study REAL9, it submitted marketing applications with the FDA and the EMA for the three indications last month. Results from the TS participants are expected later this year.Sogroya is currently approved to treat growth failure due to inadequate secretion of endogenous growth hormone in children aged 2.5 years and above and as a replacement for endogenous growth hormone in adults with growth hormone deficiency.
临床结果临床3期上市批准
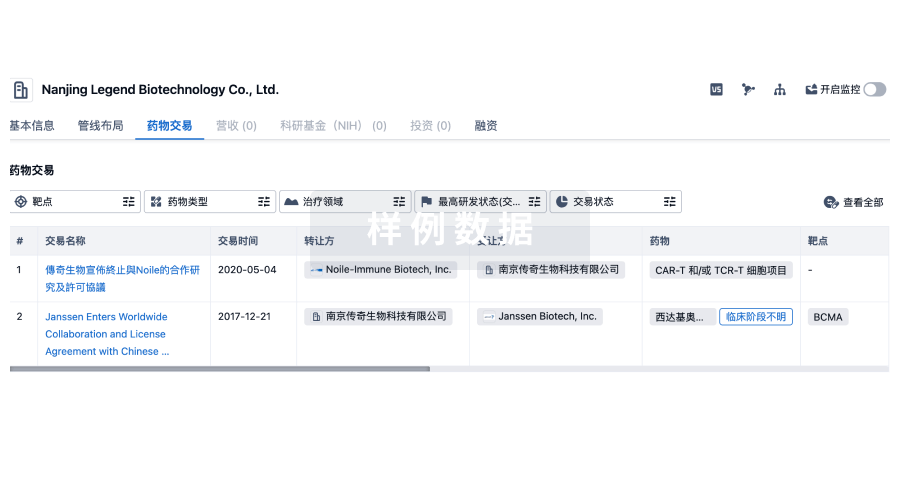
100 项与 Le Centre Hospitalier Universitaire de Toulouse 相关的药物交易
登录后查看更多信息
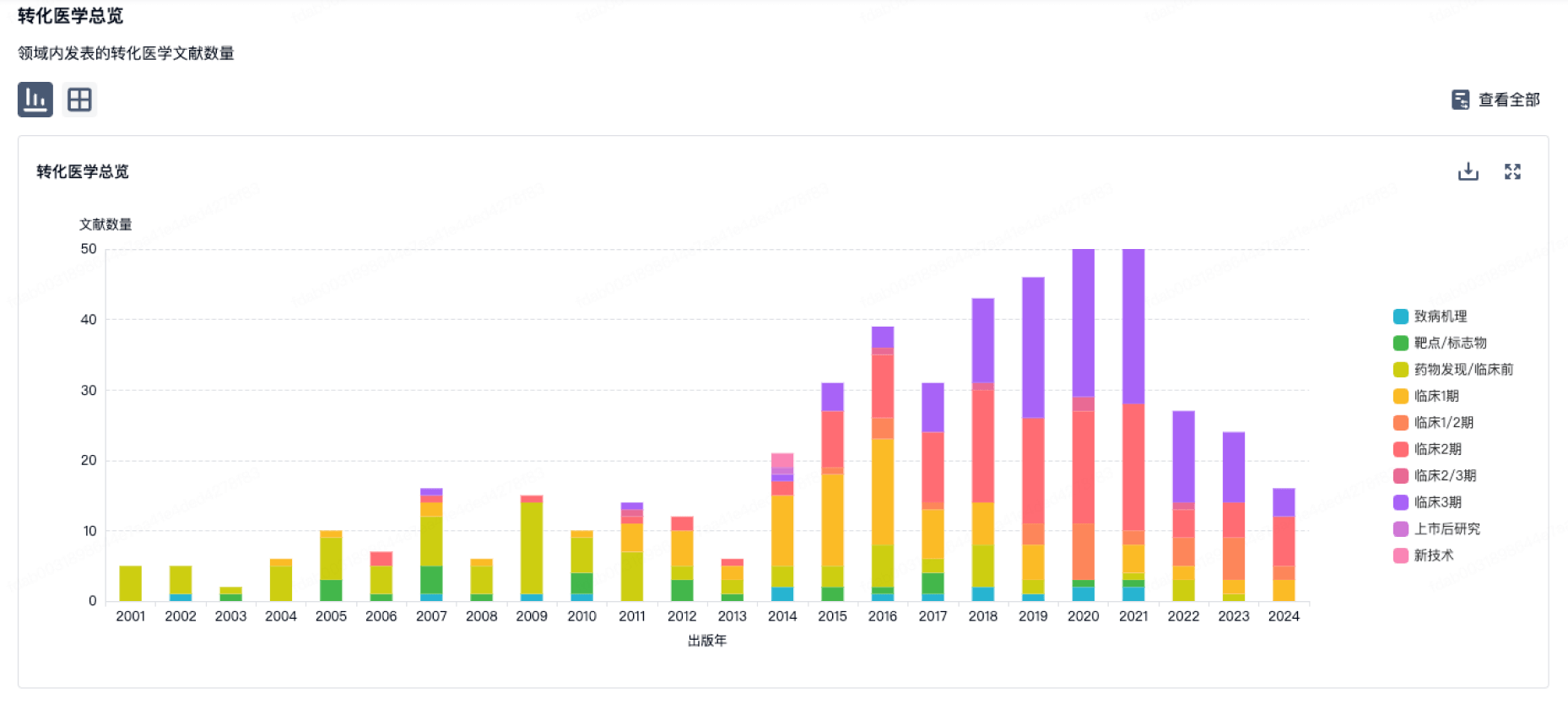
100 项与 Le Centre Hospitalier Universitaire de Toulouse 相关的转化医学
登录后查看更多信息
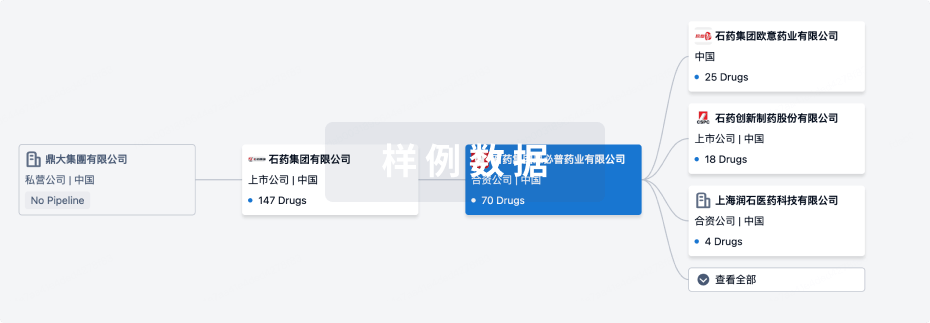
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年11月05日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
药物发现
4
1
临床1期
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
Apelin-13 ( APLNR x SIRT1 ) | 2型糖尿病 更多 | 临床1期 |
US20220304965 ( GABBR1 )专利挖掘 | 消化系统疾病 更多 | 药物发现 |
WO2024175604 ( NAGLU )专利挖掘 | 营养和代谢疾病 更多 | 药物发现 |
WO2024146880 ( mEH )专利挖掘 | 肿瘤 更多 | 药物发现 |
WO2024115935 ( CD39 )专利挖掘 | 淋巴组织增生性疾病 更多 | 药物发现 |
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
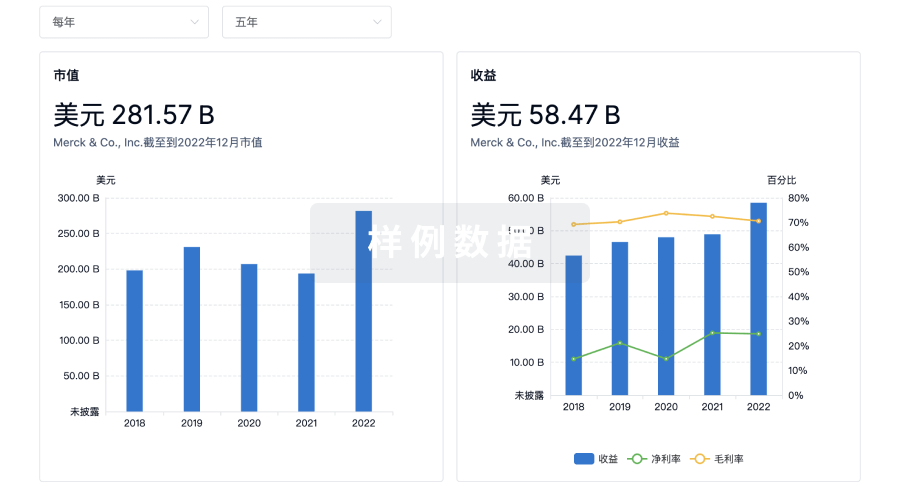
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用


