预约演示
更新于:2025-06-19

Creative Biosciences (Guangzhou) Co., Ltd.
更新于:2025-06-19
概览
关联
4
项与 广州康立明生物科技股份有限公司 相关的临床试验NCT05374369
Retrospective Analysis of Colorectal Cancer Screening Results Among People Aged 40-74 in Shipai Town, Dongguan City, China
The purpose of this study is to retrospectively analyze colorectal cancer screening data of 40-74 year old population in Shipai Town, Dongguan City.
In this study, the data of SDC2 Gene Methylation Test and Fecal Immunochemistry Test (Q-FIT) were screened from about 11,000 subjects who participated in Colorectal Cancer Screening in Shipai Town People's Livelihood Project from May 2021 to May 2022. Data from 822 subjects with positive SDC2 Gene Methylation Test and/or positive Fecal Immunochemistry Test (Q-FIT) results and with colonoscopy and/or pathological results were selected for retrospective analysis.
This retrospective study evaluated the screening performance of SDC2 Gene Methylation Test and/or Fecal Immunochemistry Test (Q-FIT) for colorectal cancer using colonoscopy and/or pathological results as the clinical standard method.
In this study, the data of SDC2 Gene Methylation Test and Fecal Immunochemistry Test (Q-FIT) were screened from about 11,000 subjects who participated in Colorectal Cancer Screening in Shipai Town People's Livelihood Project from May 2021 to May 2022. Data from 822 subjects with positive SDC2 Gene Methylation Test and/or positive Fecal Immunochemistry Test (Q-FIT) results and with colonoscopy and/or pathological results were selected for retrospective analysis.
This retrospective study evaluated the screening performance of SDC2 Gene Methylation Test and/or Fecal Immunochemistry Test (Q-FIT) for colorectal cancer using colonoscopy and/or pathological results as the clinical standard method.
开始日期2022-03-29 |
申办/合作机构 |
NCT05337189
A Multicenter, Single-blind, Observational Clinical Trial of URISAFE
The primary objective of this study is to assess the safety and effectiveness of Human Multigene Methylation Detection Kit (Fluorescent PCR Method) for help diagnose bladder cancer by comparing with clinical standard method (includes medical imaging (MRI, CT, etc.), cystoscopy, pathological examination).
开始日期2022-03-09 |
申办/合作机构  广州康立明生物科技股份有限公司 广州康立明生物科技股份有限公司 [+1] |
NCT05337163
A Multicenter, Single-blind, Pair-matched, Observational Clinical Trial of LUNSAFE
The primary objective of this study is to assess the safety and effectiveness of Human Multigene Methylation Detection Kit (Fluorescent PCR Method) for help diagnose lung cancer by comparing with clinical standard method (includes chest CT examination or pathological examination).
开始日期2022-02-25 |
申办/合作机构  广州康立明生物科技股份有限公司 广州康立明生物科技股份有限公司 [+1] |
100 项与 广州康立明生物科技股份有限公司 相关的临床结果
登录后查看更多信息
0 项与 广州康立明生物科技股份有限公司 相关的专利(医药)
登录后查看更多信息
10
项与 广州康立明生物科技股份有限公司 相关的文献(医药)2025-01-11·Gastroenterology Report
Effectiveness of single-target fecal DNA methylation test in regional mass screening for colorectal cancer and precancerous lesions in China
Article
作者: Wang, Xianshu ; Wu, Qiuning ; Yu, Zhiqiang ; Zhang, Zhi ; Kong, Xianhe ; Zou, Hongzhi ; Niu, Feng
Abstract:
Background:
Colorectal cancer (CRC) is the third-most-common malignancy and the second-leading cause of cancer-related deaths worldwide and current screening methods such as guaiac-based fecal occult blood test (gFOBT), fecal immunochemical test (FIT), and colonoscopy have their own pros and cons. This study aimed to assess the effectiveness of a fecal DNA methylation test by using methylated SDC2 (mSDC2) as the epigenetic biomarker for detecting CRC in a screening-naïve population.
Methods:
Fecal mSDC2 test and FIT were simultaneously performed on eligible 40- to 74-year-old adults of a regional township in China. Subjects with positive results were recommended for colonoscopy. Data of positivity rates, positive predicted values (PPVs), and detection rates associated with clinical characteristics were analysed.
Results:
The positivity rate of mSDC2 was 7.6% for 10,578 participants with valid results from both fecal mSDC2 test and FIT. With an adherence rate of 63.8% to colonoscopy referral, 25 CRCs, 189 advanced adenomas (AAs), and 165 non-advanced adenomas (NAAs) and polyps were detected. The PPVs of mSDC2 were 4.93%, 37.28%, and 32.54% for CRC, AA, and non-advanced lesions, respectively. When the CRCs and AAs were counted as positive findings, the fecal mSDC2 test showed a higher detective rate than FIT (relative risk [RR], 1.313 [1.129–1.528], P < 0.001). When NAAs and polyps were also specified as treatable lesions, the mSDC2 test was more effective in detecting these benign growths (RR, 1.872 [1.419–2.410]; P < 0.001). A combination of mSDC2 and FIT detected 29 CRCs, 298 AAs, and 234 NAAs and polyps. Overall, the fecal mSDC2 test had a higher detection rate for both advanced and non-advanced colonic lesions. The false-positive rate of the fecal mSDC2 test was comparable to that of FIT (RR, 1.169 [0.974–1.403]; P = 0.113).
Conclusions:
The single-target stool-based mSDC2 test can effectively and accurately detect CRC and precancerous lesions in a large-scale CRC-screening program.
Trial registration number:
NCT05374369.
2022-12-01·BMC cancer2区 · 医学
A novel and sensitive DNA methylation marker for the urine-based liquid biopsies to detect bladder cancer
2区 · 医学
ArticleOA
作者: Zhu, Yueting ; He, Lei ; Deng, Leihong ; Yu, Zhaojun ; Wang, Xianshu ; Deng, Huanhuan ; Gong, Yun ; Liu, Lirong ; Zeng, Tao ; Liao, Caizhi ; Tang, Zhimin ; Wang, Qingping ; Huang, Longwu ; Zhao, Rongsong ; Li, Feng ; Chao, Haichao ; Qi, Yan ; Zou, Hongzhi
Abstract:
Background:
Better prognostic outcome is closely correlated with early detection of bladder cancer. Current non-invasive urianalysis relies on simultaneously testing multiple methylation markers to achieve relatively high accuracy. Therefore, we have developed an easy-to-use, convenient, and accurate single-target urine-based DNA methylation test for the malignancy.
Methods:
By analyzing TCGA data, 344 candidate markers with 424 primer pairs and probe sets synthesized were systematically screened in cancer cell lines, paired tissue specimens, and urine sediments from bladder cancer patients and normal controls. The identified marker was further validated in large case-control cohorts. Wilcoxon rank sum tests and c2 tests were performed to compare methylation levels between case-control groups and correlate methylation levels with demographic and clinical characteristics. In addition, MSP, qMSP, RT-PCR, western blot analysis, and immunohistochemistry were performed to measure levels of DNA methylation, mRNA transcription, and protein expression in cancer cell lines and tissues.
Results:
A top-performing DMRTA2 marker identified was tested in both discovery and validation sets, showing similar sensitivity and specificity for bladder cancer detection. Overall sensitivity in the aggregate set was 82.9%(179/216). The specificity, from a control group consisting of patients with lithangiuria, prostatoplasia, and prostatitis, is 92.5%(468/506). Notably, the methylation assay had the highest sensitivities for tumors at stages of T1(90.4%) and T2(95.0%) compared with Ta (63.0%), T3(81.8%), and T4(81.8%). Furthermore, the test showed admirable detection rate of 80.0%(24/30) for recurring cancers. While methylation was observed in 39/54(72.2%) urine samples from patients with carcinomas of renal pelvis and ureter, it was detected at extremely low rate of 6.0%(8/133) in kidney and prostate cancers. Compared with SV-HUC-1, the normal bladder epithelial cell line, DMRTA2 was hypermethylated in 8/9 bladder cancer cell lines, consistent with the results of MSP and qMSP, but not correlated with mRNA and protein expression levels in these cell lines. Similarly, DMRTA2 immunostaining was moderate in some tissues but weak in others. Further studies are needed to address functional implications of DMRTA2 hypermethylation.
Conclusions:
Our data demonstrated that a single-target DNA methylation signature, mDMRTA2, could be highly effective to detect both primary and recurring bladder cancer via urine samples.
2021-09-01·Materials Express
Mechanisms of Paeoniflorin against myocardial ischemia reperfusion injury based on network pharmacology
作者: Luo, Chunyu ; Ling, Wenpei ; Qin, Shuzhi ; Li, Feng ; Zhao, Chengguo ; Yin, Meifang
Ischemic heart disease (IHD) is the primary reason of death of cardiovascular diseases. Paeoniflorin (PF), a monoterpene glycoside extracted from Radix Paeoniae Rubra or Paeoniae Radix Alba, can ameliorate myocardial ischemia/reperfusion injury (MIRI), but its mechanism is not
still defined. In this study, network pharmacology was utilized, the protein interaction network between PF and MIRI targets were screened for bioenrichment analysis. Moreover, the anti-MIRI effects of PF (30, 60 and 120 mg/kg) were investigated in vivo on rats for verification. The
myocardial infarction area was assessed by TTC/Evans blue staining and morphological changes of tissues were evaluated using hematoxylin and eosin staining. The contents of myocardial enzymes and oxidation resistance were measured. The cell apoptosis was evaluated using TUNEL staining and
the expression of proteins was estimated using Western Blot. In the results, the relevant targets and the biological processes of PF against MIRI were screened out, indicating its anti-MIRI potential pharmacological effects of PF. 120 mg/kg PF can shrink infarction area after ischemia/reperfusion,
ameliorate pathological morphology in myocardial tissue, lower the levels of myocardial enzymes, and attenuate oxidative stress. Furthermore, PF could reduce the positive rate of TUNEL staining caused by MIRI. Moreover, 120 mg/kg PF could depress the protein levels of Bax, Caspase-3, Beclin-1
and Cathepsin B and increase the protein level of Bcl-2 on rats after reperfusion. In conclusion, Paeoniflorin has an anti-MIRI effect in rats via coordinate regulation of anti-oxidative stress, anti-apoptosis and inhibition of autophagy.
14
项与 广州康立明生物科技股份有限公司 相关的新闻(医药)2025-02-28
·氨基观察
氨基观察-创新药组原创出品
作者 | 黄恺
中国生物制药持续引进管线。
2月27日,中国生物制药宣布,与先为达生物签署独家战略合作协议,就其研发的人白细胞介素-29项目CPX102在中国(含港澳台)、巴西、沙特阿拉伯、泰国、新加坡等19个国家达成独家许可与合作。
CPX102是在IL-29的基础上,经蛋白质工程优化得到的雾化吸入溶液,属于III型干扰素的一种。目前中国生物制药正针对该项目在中国开展IIb期临床试验,用于治疗儿童呼吸道合胞病毒(RSV)感染。
百济神州业绩出色。
2月27日,百济神州发布Q4财报。2024年第四季度,全球总收入达11亿美元,同比增长78%,全年全球总收入达38亿美元,同比增长55%;GAAP经营亏损持续收窄,实现全年非GAAP经营利润为正。
在过去的一天里,国内外医药市场还有哪些热点值得关注?让氨基君带你一探究竟。
/ 01 /
市场速递
1)赛生药业引进卫材小分子抗癌新药
2月28日,赛生药业宣布,已就成纤维细胞生长因子受体选择性酪氨酸激酶抑制剂tasurgratinib与卫材达成授权许可协议。Tasurgratinib是一种口服新型酪氨酸激酶抑制剂,对FGFR1、FGFR2和FGFR3表现出选择性抑制活性。根据协议条款,赛生药业将负责tasurgratinib在中国的产品开发和商业化。
2)中国生物制药引进先为达RSV新药
2月27日,中国生物制药宣布,与先为达生物签署独家战略合作协议,就其研发的人白细胞介素-29项目CPX102在中国(含港澳台)、巴西、沙特阿拉伯、泰国、新加坡等19个国家达成独家许可与合作。 CPX102是在IL-29的基础上,经蛋白质工程优化得到的雾化吸入溶液,属于III型干扰素的一种。目前中国生物制药正针对该项目在中国开展IIb期临床试验,用于治疗儿童呼吸道合胞病毒(RSV)感染。
/ 02 /
资本信息
1)百济神州2024年第四季度收入11亿美元
2月27日,百济神州发布Q4财报。2024年第四季度,全球总收入达11亿美元,同比增长78%,全年全球总收入达38亿美元,同比增长55%;GAAP经营亏损持续收窄,实现全年非GAAP经营利润为正。
2)再鼎医药2024年第四季度收入1.09亿美元
2月27日,再鼎医药公布Q4财报。2024年第四季度,公司总收入为1.091亿美元,同比增长66%。2024年全年总收入为3.990亿美元,同比增长50%;2025年全年收入指引为5.60亿美元至5.90亿美元。
/ 03 /
医药动态
1)神州细胞抗PD-1单抗联合疗法获批,一线治疗肝癌
2月28日,据NMPA官网,神州细胞菲诺利单抗注射液)与贝伐珠单抗注射液联合疗法的上市许可申请已获得批准,本次获批的适应症为:适用于既往未接受过系统治疗的不可切除或转移性肝细胞癌患者。
2)科兴制药英夫利西单抗在孟加拉国获批上市
2月28日,科兴制药宣布,引进管线英夫利西单抗在孟加拉国获批上市。
/ 04 /
器械跟踪
1)科曼医疗急救转运呼吸机获注册许可
2月28日,据NMPA官网,科曼医疗急救转运呼吸机获注册许可。
2)一影医疗移动式C形臂X射线机获注册许可
2月28日,据NMPA官网,一影医疗移动式C形臂X射线机获注册许可。
3)康立明生物人类SDC2基因甲基化检测试剂盒(荧光PCR法)获注册许可
2月28日,据NMPA官网,康立明生物人类SDC2基因甲基化检测试剂盒(荧光PCR法)获注册许可。
/ 05 /
数字医疗日报
1)京东健康旗下医疗大模型全面开源
近日,京东健康旗下“京医千询”医疗大模型启动开源,成为国内医疗行业首个全面开源的垂类大模型。
PS:欢迎扫描下方二维码,添加氨基君微信号交流。
财报临床2期临床3期临床1期临床终止
2024-05-09
TDS2024检测自动化以及创新测序技术在阿尔兹海默症、肿瘤、遗传、病原等领域应用论坛;合作热线:17701860390文章来源:药陌摘要ICL是指独立于医疗机构,为各级医院、社区卫生服务中心、乡镇卫生院、体检中心、疾控中心等提供的医学诊断检测服务。提供第三方医学诊断服务的医学检验中心通常被称为独立医学实验室。从第三方医学诊断提供的服务来看,可将其主要划分为医学检验与病理诊断两大板块的业务。医学检验包括常规的生化检验、免疫学检验等以及高端检验(如基因检测等)。病理检验包括细胞病理诊断、组织病理诊断等。 1 ICL(第三方医学检验实验室)行业定义独立医学实验室(Independent Clinical Laboratory)简称ICL,也称第三方医学实验室。一般来说是指获得了卫生行政部门许可的、具有独立法人资格的、专业从事医学检测的服务性医疗机构。国家卫健委将其定义为:以提供人类疾病诊断、管理、预防和治疗或健康评估的相关信息为目的,对来自人体的标本进行临床检验,包括临床血液与体液检验、临床化学检验、临床免疫检验、临床微生物检验、临床细胞分析遗传学检验和临床病理检查等,并出具检验结果,具有独立法人资质的医疗机构。 2 ICL(第三方医学检验实验室)行业分类中国ICL行业分为普检与特检,其中普检的客户为公立一级、二级医院;而特检的客户为公立三级医院。普检的检测范围为《医疗机构临床检验项目目录》中规定的检测范围,而目录外的检测范围属于特检的范畴。就技术难度来看,普检的技术难度较特检的技术难度相对较低 3 ICL(第三方医学检验实验室)行业特征中国ICL(第三方医学实验室)现阶段主要分为三大特征:第一,由于ICL业务标准化,在各地开展业务普及较为容易。第二,国内外发展差距大,日本、美国和中国的医疗体系倒置的,导致渗透率不能在同一个维度下对比。中国公立医院是患者的主要流量入口,设备完善,大多数都能提供检测设备,普检业务外包的可能性较低。第三,普检市场呈现规模化占据龙头地位,特检市场呈现细分赛道高速发展,同时特检种类繁多,形成异质寡头的竞争格局,驱动行业增长。 4 中国ICL(第三方医学检验实验室)发展历程中国ICL行业发展至今已经进入了高速发展的时期,上世纪八十年代以前中高ICL步入了萌芽时期,医学检验业务主要由医院的检验科完成。上世纪80年代中后期,出现了独立医学实验室雏形且实现规模化、专业化的优势,接手医院的医学检验业务外包业务,提升了检验效率及检验水平。在实现规模化之后,受到四个主要影响推动了ICL的快速发展。第一,2009年卫生部印发《医学检验基本标准(试行)》,在医疗机构类别中增设“医学检验所”,确立了第三方医学检验的合法地位。第二,2016年原国家卫计委颁布了独立设置医疗机构相关标准,大量机构申请进入市场或者扩大业务范围。第三,2017年后市场竞争逐渐激烈,部分小型医学实验室开始被淘汰,大型医学实验室开始在专业细分领域纵深发展,择优淘劣后第三方检验市场开始走向集中。最后,在医保控费的大背景下,医院的检验科可能变为成本中心,第三方检验机构因其规模化、专业化服务可能在行业中占据更重要的行业地位。开始时间:1970 结束时间:1980 阶段:萌芽期行业动态:随着检验科技的进步和检验需求的上升,中小型医院因资金和技术限制无法提供齐全的诊断服务,而大型医院因业务量等压力无法完全满足检验及诊断业务需求阶段特征:上世纪80年代以前,中国的医学检验业务主要由医院的检验科完成。开始时间:1980 结束时间:1989 阶段:启动期行业动态:独立医学实验室凭借其规模化、专业化的优势接受医院的医学检验业务外包业务,提升了检验效率及检验水平。21世纪初,广州金域医学检验中心成为国内第一个被卫生行政部门批准的独立医学实验室。阶段特征:中国出现了独立医学实验室雏形。开始时间:2009 结束时间:2022 阶段:高速发展期行业动态:2009年卫生部印发《医学检验基本标准(试行)》,在医疗机构类别中增设“医学检验所”,确立了第三方医学检验的合法地位。2016年原国家卫计委颁布了独立设置医疗机构相关标准,大量机构申请进入市场或者扩大业务范围。2017年后市场竞争逐渐激烈,部分小型医学实验室开始被淘汰,大型医学实验室开始在专业细分领域纵深发展,择优淘劣后第三方检验市场开始走向集中。在医保控费的大背景下,医院的检验科可能变为成本中心,第三方检验机构因其规模化、专业化服务可能在行业中占据更重要的行业地位。阶段特征:第三方医学检验机构开始规模化发展。 5 ICL(第三方医学检验实验室)产业链分析ICL产业链上游主要提供检验分析设备及专利试剂盒,ICL产业链中游主要负责提供独立医学实验室服务,ICL产业链下游主要为医疗机构。上游主要为医学检测设备和试剂生产厂家,ICL上游器械供应商巨头有罗氏、迈瑞等,集中在医学影像领域。上游集中度整体偏高,海外上游检验设备供应商占据较大份额。ICL行业上游的话语权较强,2019年金域医学和迪安诊断的上游采购中,前五大供应商采购额分别达34%、 66.2%,其中迪安诊断最大的供应商罗氏,2019年采购金额占当年的总采购金额的52.22%。中国IVD诊断设备和试剂的国产化进程近几年推进很快,迈瑞、迈克、安图等国产厂商逐渐崛起,预计后续随着国产化进程的加速,产业链上游国产化率提高、成本下降,ICL行业上游国产化程度提升,特检的产业链上游分布在专利试剂盒领域。专利试剂盒目前已经有肺癌早筛试剂盒(凯保罗)、肠癌早筛试剂盒(康立明、诺辉)、基因测序(华大基因、贝瑞和康)。ICL行业产业链中游分为普检与特检。提供普检的公司主要有金域医学、迪安诊断、艾迪康、达安基因等。金域医学的市场占有率较高,年检验样本量维持在行业领先水平。衡量普检赛道的主要因素有年检验样本量、合作机构数量、实验室数量、检验收入,通过这些指标可以判断企业的规模化程度。提供特检项目的公司较多,行业呈现异质化龙头格局,主要项目集中在血液病检测、肿瘤检测、神经病学检测、遗传病检测、妇科检测、传染病检测。多数特检企业位于产业链上游,采用与中游独立实验室合作的模式进行检测。衡量特检赛道的主要因素有研发成本、研发技术、检测业务覆盖范围,通过这些指标可以判断企业的技术程度及业务协同作用。下游根据ICL独立医学实验室扣率不同,会影响医院的收入状况,从而影响医院的利润率。以TCT检测为例,患者付费固定为220元,第三方独立医学实验室成本为30-40元,医院自行提供检测的成本在70-80元。当扣率在60%时,第三方独立医学实验室的利润率可以达到77.3%,医院的利润仅有20.5%。当扣率在40%时,第三方独立医学实验利润率达到65.9%,医院利润率升高至47%。由于成本考量,第三方独立医学实验室的利润率基本均高于医院。当医院采用ICL独立医学实验室利润率在20.5%-47%之间,根据扣率不同,利润率会有较大浮动。 6 ICL(第三方医学检验实验室)行业规模2016-2020年,中国ICL独立医学实验室行业市场规模(以终端收入计)从11,739.2百万元人民币增至30,694.9百万元人民币,期间年复合增长率为27.2%。预计至2025年,行业市场规模将达到47,946.2百万元,期间年复合增长率为6.7%。ICL相对于医院实验室的独特优势。ICL享有相对于医院实验室的各种优势。首先,ICL为不同背景及需求的医疗终端提供服务。其次,ICL一般较个别医院实验室提供更多的检验项目,满足临床医生广泛的检测需求。第三,通过提供大量的检测服务,ICL可实现规模效益,为医院带来更佳的成本效益。第四,ICL较医院实验室更灵活使用新技术及设备,并往往会更积极地改善其质量控制及招募行业专家,提供更好的检验服务,节省医生与病患的时间。中国ICL行业市场规模,2016-2025E 7 ICL(第三方医学检验实验室)政策梳理政策名称:《国务院关于印发“ 十三五”深化医药卫生体制改革规划的通知》 颁布主体:国务院 生效日期:2016-12-27 影响:6政策性质:鼓励性政策 政策内容:健全完善医疗卫生服务体系。优化医疗卫生资源布局,明确各级各类医疗卫生机构功能定位,加强协作,推动功能整合和资源共享。合理控制 公立综合性医院数量和规模。大力推进面向基层、偏远和欠发达地区的远程医疗服务体系建设,鼓励二、三级医院向基层医疗卫生机构提供远 程服务,提升远程医疗服务能力。 政策解读:鼓励社会力量举办医学检验机构、病理诊断机构、医学影像检査机构、消毒供应机构和血液净化机构,鼓励公立医院面向区域提供相关服务, 实现区域资源共享。加强医疗质量控制,推进同级医疗机构间以及医疗机构与独立检査检验机构间检査检验结果互认。 政策名称:《关于支持社会力量提供多层次多样化医疗服务的意见》 颁布主体:国务院 生效日期:2017-05-23 影响:6 政策性质:指导性政策 政策内容:加快发展专业化服务。积极支持社会力量深入专科医疗等细分服务领域,扩大服务有效供给,培育专业化优势。在眼科、骨科、口腔、妇产、 儿科、肿瘤、精神、医疗美容等专科以及康复、护理、体检等领域,加快打造一批具有竞争力的品牌服务机构。鼓励投资者建立品牌化专科医 疗集团、举办有专科优势的大型综合医院。 政策解读:支持社会力量举办独立设置的医学检验等专业机构,面向区域提供相关服务。 政策名称:《关于进一步改革完善医疗机构、医师审批工作的通知》 颁布主体:国家卫健委 生效日期:2018-06-19 影响:5政策性质:规范类政策 政策内容:在保障医疗质量安全的前提下,医疗机构可以委托独立设置的医学检验实验室、病理诊断中心、医学影像诊断中心、医疗消毒供应中心,或者 有条件的其他医疗机构提供医学检验、病理诊断、医学影像、医疗消毒供应等服务。同时应当签订委托协议书,明确具体服务项目,厘清双方 权利、义务和责任。 政策解读:明确提出了第三方医疗机构的共享机制;医疗机构与独立设置的医疗机构签订协议,可作为相关诊疗科目的登记依据。独立设置的医疗机构参 与医疗机构、城市医疗集团与县域医疗共体均有了明确的实施路径。 政策名称:《关于开展社区医院建设试点工作的通知》 颁布主体:国家卫健委 生效日期:2019-02-27 政策性质:鼓励性政策 政策内容:在医技等科室方面,至少设置医学检验科(化验室)、影像诊断、临床检验等科室可由第三方机构或者医联体上级医疗机构提供服务。政策解读:大力推动结果互认制度。制订完善检查检验技术标准和操作规范,广泛开展相关人员培训,提高操作和诊断水平。发挥医学检验、医学影像、 病理等专业质控中心作用,加大医疗质量控制力度,提高检查检验同质化水平。在医联体内率先实现医学检验、医学影像、病理检查等资料和 信息共享。通过省级、市级等相关专业医疗质量控制合格的,要在相应级别行政区域内实行检查检验结果互认,不断增加互认的项目和医疗机 构数量。有条件的地区可以引入第三方保险,建立起检查检验结果互认的风险共担机制,减少因互认造成的医疗纠纷和经济损失。 政策名称:《促进社会办医持续健康规范发展意见的通知》 颁布主体:国家卫健委 生效日期:2019-06-10 影响:6 政策性质:鼓励性政策 政策内容:发挥三级公立医院带动作用。各地要完善医联体网格化布局,社会办医可以选择加入,综合力量或者专科服务能力较强的社会办医可牵头组建 医联体,鼓励适度竞争。支持公办和社会办医按照平等自愿原则组建专科联盟。支持社会办医参加远程医疗协作网,提高诊疗服务能力。 政策解读:严格控制公立医院数量和规模,为社会办医留足发展空间。各地在新增或调整医疗卫生资源时,要首先考虑由社会力量举办或运营有关医疗机 构。支持三级公立医院与社会办医共享医学影像、医学检验、病理诊断等服务,形成全社会医疗合作管理体系。 政策名称:《关于引发医学检验实验室管理暂行办法的通知》 颁布主体:国务院 生效日期:2020-08-01 影响:2 政策性质:规范类政策 政策内容:在新冠肺炎疫情防控过程中,独立设置的医学检验实验室在核酸检测中发挥了积极作用。为进一步加强独立设置的医学检验实验室管理,保证 医疗质量和医疗安全,国务院联防联控机制医疗救治组针对部分地区在组织全员核酸检测过程中存在的问题,组织制定了《医学检验实验室管 理暂行办法》,对各地医学检验实验室提出具体要求。 政策解读:集中组织一次对辖区内所有医学检验实验室的全面检査,重点检査样本数量与检测能力不匹配、检测流程不规范、报吿反馈不及时等问题,对 发现的问题建立台账,明确责任人,实行限时整改。 政策名称:《关于进一步规范医疗行为促进合理医疗检査的指导意见》 颁布主体:国家卫健委、发改委 生效日期:2020-12-29 影响:3政策性质:鼓励性政策 政策内容:加强机制创新,进一步促进资源共享。一是推进检查检验结果互认。明确互认机构范围、条件、诊疗项目(内容)及技术标准等,提出逐步实 现区域内医疗机构间检查检验结果互认的目标要求。二是促进检查检验资料共享,探索设置区域医学影像、检验、病理等诊断中心。三是加快 医疗联合体内结果互认,提出目标要求。 政策解读:鼓励有条件的地区按照标准独立设置医学影像中心、医学检验中心、病理诊断中心,并统一纳入卫生健康部门医疗质量控制体系,为区域内医 疗机构提供检査服务,实现资源共享。 政策名称:《广州市战略性新兴产业发展“十四五”规划》 颁布主体:广州市政府 生效日期:2022-03-23 影响:5 政策性质:鼓励性政策 政策内容:在医学检验领域,提出积极支持实验室自建检测方法(LDT)试点,鼓励开发“整合式”平台技术,研发高端检验检测一体化设备,攻克仪器的 稳定性、可靠性、微型化和智能化等关键技术。鼓励医检业务外包,将第三方医学检验作为公立医疗机构的补充。支持检验检测产品纳入医保 目录。要培育发展新型健康服务业,瞄准精准医疗。 政策解读:广州把发展壮大战略性新兴产业作为经济工作的首要工程,其中,生物医药与健康产业增加值2025年目标达到2100亿元,并分别在医学检验、 基因检测、精准医疗、智慧医疗等方面做出了规划。 政策名称:《“十四五”全民医疗保障规划的通知》 颁布主体:国务院 生效日期:2022-09-23 影响:4 政策性质:规范类政策 政策内容:医疗保障是减轻群众就医负担、增进民生福祉、维护社会和谐稳定的重大制度安排。习近平总书记指出,要加快建立覆盖全民、城乡统筹、权 责清晰、保障适度、可持续的多层次医疗保障体系。 政策解读:优化提升医疗卫生服务体系。完善区域卫生规划和医疗机构设置规划,健全城市三级医院、县级医院和基层医疗卫生机构分工协作的现代医疗 卫生服务体系,支持整合型医疗卫生服务体系建设,加强分级诊疗体系建设,推进基层医疗卫生机构发展,促进基层医疗卫生服务有效利用和 患者有序就医。促进定点医药机构行业行为规范、成本控制和行业自律。支持中医药传承创新发展,强化中医药在疾病预防治疗中的作用,推 广中医治未病干预方案。支持儿科、老年医学科、精神心理科和康复、护理等紧缺医疗服务发展。鼓励日间手术、多学科诊疗、无痛诊疗等医 疗服务发展。完善检查检验政策,推进医疗机构检查检验结果互认。支持远程医疗服务、互联网诊疗服务、互联网药品配送、上门护理服务等 医疗卫生服务新模式新业态有序发展,促进人工智能等新技术的合理运用。 8 ICL(第三方医学检验实验室)竞争格局ICL普检行业呈现规模化程度较高、利润较低的主要现象,ICL特检行业整体呈现规模化程度较低、利润较高的现象。特检与普检之间并不存在相互竞争的现象。主营业务是普检的企业主要有金域医学、迪安诊断、艾迪康、凯普,主营业务是特检的企业主要有华大基因、贝瑞和康、康圣环球、微远基因、燃石医学、泛生子、金匙医学、予果基因、杰毅生物,分别覆盖不同的领域。普检行业呈现规模化程度较高、利润较低的现象,特检行业呈现规模化程度较低、利润较高的现象。特检与普检并不存在竞争状况,金域医学、迪安诊断等普检行业巨头都已经开始进行注资特检行业的战略布局。根据ICL产业链利润与盈利能力分析,产业链上游毛利率位于50%-65%之间,盈利能力较强,资产负债率低于ICL中游。产业链中游特检行业ROE较高,然而资产负债率与净利率都不可观,因为特检行业属于新兴行业,目前成本增长幅度仍然较高,但盈利能力可观,当行业格局稳定时,预计收入较为可观。普检行业由于已经处于稳定的竞争格局,盈利能力较为一般,需要寻求新的技术突破。X轴——盈利能力:主要多维度参考营业收入、毛利率等,辅助参考ROE、净利率。对于企业进行综合评估后,赋值1-10。Y轴——规模化程度:企业在ICL行业的的技术成熟度和商业化能力以及市场应用等多个方面进行参考。以下列企业为基础进行1-10的赋值。气泡大小——市场占有情况:依照沙利文和头豹研究院的市场占有率数据予以评分,赋值1-10分。气泡深浅——业务类型:依照ICL行业的市场分类,分别对于普检行业的企业赋值5。对于特检行业企业赋值10.主要用于区分普检特检企业,无实义。 9 ICL(第三方医学检验实验室)代表企业分析 广州金域医学检验集团股份有限公司企业类型 : 股份有限公司(上市、自然人投资或控股)成立时间 : 2006-05-26经营范围 : 投资咨询服务;商品信息咨询服务;生物技术开发服务;生物技术咨询、交流服务;软件开发;信息技术咨询服务;信息系统集成服务;计算机房维护 服务;水质检测服务;环境保护监测;水污染监测;化工产品检测服务;医学研究和试验发展;生物技术转让服务;企业总部管理;房屋租赁;场地租赁 (不含仓储);物业管理;电话信息服务;食品检测服务;租赁业务(外商投资企业需持批文、批准证书经营);品牌名称 : 广州金域医学检验集团股份有限公司广州金域医学检验集团股份有限公司竞争优势 实验室布局:金域医学已在内地及香港地区建立了38家中心实验室,拥有遍布全国的远程病理协作网,服务网络覆盖全国90%以上人口所在 区域,并以香港为桥头堡,服务粤港澳大湾区以及“一带一路”沿线国家和地区。研发团队:金域医学注重搭建国际化高端化人才和团队,拥有超过1200名科研人员,海内外知名专家200余人,其中从海外归国学者30余人 ,并成立了由钟南山院士担任主席,曾溢滔、陈润生、侯凡凡、谢晓亮、陈晔光、谭蔚泓、张学等7位院士担任顾问。平台服务:金域医学拥有全球领先的肾脏病超微病理诊断中心、对接国家级平台的呼吸道病毒诊断研究中心,获批建立了医学检测技术与服 务国家地方联合工程实验室、国家级的博士后科研工作站、广东省院士工作站、广东省企业重点实验室等国家、省部级的研发机构和研发平 台。年检验量:通过对接国际和自主创新等多种方式,金域医学提供超过2800项检测项目。年检测标本量超1亿例,积累了全球领先的东方人种大 样本、大数据库,并以此为基础推动体外诊断产业和人工智能诊断的原始创新。 迪安诊断技术集团股份有限公司成立时间 : 2001-09-05经营范围 : 一般项目:技术服务、技术开发、技术咨询、技术交流、技术转让、技术推广;第一类医疗器械销售;第二类医疗器械销售;企业管理咨 询;业务培训(不含教育培训、职业技能培训等需取得许可的培训);信息系统运行维护服务;货物进出口;技术进出口;第二类医疗器械 租赁(除依法须经批准的项目外,凭营业执照依法自主开展经营活动)。许可项目:第三类医疗器械经营;第三类医疗器械租赁(依法须经批准 的项目,经相关部门批准后方可开展经营活动,具体经营项目以审批结果为准)。以下限分支机构经营:一般项目:第一类医疗器械生产(除 依法须经批准的项目外,凭营业执照依法自主开展经营活动)。股票类型 : A股品牌名称 : 迪安诊断技术集团股份有限公司迪安诊断技术集团股份有限公司竞争优势 肿瘤业务:迪安诊断的优势学科是肿瘤诊断业务。迪安诊断肿瘤学科下设血液病诊断中心、肿瘤高通量基因检测中心、肿瘤防治筛查中心, 为肿瘤患者、高危人群和健康人群,以及相关领域研究人员,提供科学专业的分子诊疗及科研服务解决方案。战略合作:迪安诊断专注于诊断技术平台创新,与约翰•霍普金斯大学、罗氏、西门子等多家国际知名机构达成战略合作。与国内众多体外诊 断机构合作打通渠道,建立了覆盖浙江、北京、广东、云南、新疆等地区各等级医疗机构的产品销售与服务体系,代理产品来自罗氏诊断、 梅里埃、希森美康、伯乐等国际领先厂商。两大平台:依托诊断服务、健康管理两大业务平台以及采样点网络建设,打造医生端、用户端,方便对出院患者开展健康管理,患者出院后 可以应用医生制定的随访方案进行定期随访,就近在迪安采样点进行采样,数据实时同步给医生,实现对身体指标的持续监测。 杭州艾迪康医学检验中心有限公司 统一社会信用代码: 91330106757229413U企业类型 : 有限责任公司(自然人投资或控股)成立时间 : 2004-01-16经营范围 : 服务:医学检验科,临床体液、血液专业,临床微生物学专业,临床化学检验专业,临床免疫、血清学专业,临床细胞分子遗传学专业(不 含产前筛查项目),病理科,新型诊断试剂及诊断技术、医药及生物工程新技术、新产品、医疗信息技术的技术开发、成果转让,计算机软 硬件、医疗卫生系统应用软件、电子通讯技术及其他计算机软硬件技术开发、技术服务、技术咨询、成果转让,计算机网络系统集成,机械 设备租赁(除拆、装),成年人的非证书劳动职业技能培训(涉及前置审批的项目除外);货物进出口(国家法律、行政法规禁止的项目除 外,法律、行政法规限制的项目取得许可证后方可经营)。(依法须经批准的项目,经相关部门批准后方可开展经营活动)品牌名称 : 杭州艾迪康医学检验中心有限公司杭州艾迪康医学检验中心有限公司竞争优势 物流网络覆盖广,时效高。艾迪康医学检验中心在全国范围内(除港澳台外),共计3014个县(区),物流已经覆盖1520个县(区),实验 室所在地的样本可实现12H送达实验室,外包物流最快可实现当日达。物流网络覆盖30个省、自治区、直辖市30个。物流服务人员1300余 人。全面的检测技术平台及检验项目支持。艾迪康丰富的检验经验、全面的检测技术平台及丰富的检测项目将为广大医疗机构提升检验检查水平 与医技能力。艾迪康依托现有的100+战略合作伙伴资源,可为实验室提供国内外先进检验设备和一揽子试剂耗材整体解决方案,解决实验室 仪器设备不足、试剂耗材使用订购不合理的问题,在提升医院技术平台与检测项目多样性的同时为医院降本增效,建立安全、可追溯的全方 位技术平台服务体系。丰富的第三方独立医学检验实验室行业经验和运营能力。艾迪康成立于2004年1月8日,是浙江省第一家独立医学实验室,也是全国跨地区连 锁经营的独立医学实验室,具有丰富的医学检验实验室行业经验及为医院客户合作的经验。公司具有丰富的实验室建设和运营经验,可提供 不同类型实验室的规划设计服务,同时提供建设完成后实验室的整体全流程协同运营服务,用数据驱动临床路径的优化,保障医疗安全和医疗质量。ENDTDS2024实验室检测自动化建设以及在阿尔兹海默症、肿瘤、遗传、病原等领域应用论坛合作热线:17701860390戳“阅读原文”立即领取限量免费参会名额!
2023-12-12
·动脉网
动脉网第一时间获悉,近日,软式内窥镜新星深圳科思明德医疗科技有限公司(以下简称“科思明德”)宣布完成数千万元人民币A轮融资。本轮融资由IDG资本领投,老股东同伟创业和国家高性能医疗器械创新中心(以下简称“国创中心”)继续超额跟投。本次融资也是科思明德继2023年1月完成Pre A轮融资以来,年内完成的第二轮融资。在新老股东的合力下,公司将持续强化软式电子内窥镜产品的创新与研发,扩大市场影响力和占有率,加速软镜行业的国产替代。科思明德成立于2022年,公司专注于软式电子内窥镜创新产品的研发,致力于挖掘临床需求,精细打造优质产品,为临床用户提供最佳的诊断及治疗解决方案。科思明德团队具备丰富的产品研发及生产经验,围绕软式电子内窥镜平台构建了完善的底层技术储备,能实现主机、镜体的深度自研自制,全新的技术方案涵盖几十项专利技术。 2023年8月公司总部迁址到深圳龙华区锦绣科学园三期目前,科思明德已推出全新的高端智能一体化软镜平台V1000,以及配套的创新型胃镜、肠镜产品,并围绕软镜平台布局了多项革新性产品,覆盖消化、呼吸、五官、妇科、泌尿等临床领域。V1000,全新一代智能电子内窥镜系统在2023年,公司陆续亮相上海春季CMEF、深圳秋季CMEF、消化内科专业峰会和论坛,公司产品凭借崭新的产品定义、高品质的图像质量和一流的操控性能,受到了行业的广泛关注。根据部分权威世界卫生组织市场报告数据分析显示,恶性肿瘤的发病率和死亡率随年龄的增加而上升,从40 岁以后开始快速升高。另一方面,随着我国老龄化的不断加重,消化道癌症发病率日渐增高。在现阶段,由于中国民众对于早癌筛查认识不足并且对于胃肠镜检查的接受度有限,叠加内镜医师资源不足以及医疗资源分布不均衡等因素,中国目前仍存在早癌筛查意识较为淡薄、筛查体系不够完善、筛查普及率偏低等问题,导致中国目前仍然难以开展大规模的胃肠癌普查。随着人口老龄化加剧,消化道早癌筛查、医疗基建、分级诊疗等多重利好政策推进,以及内窥镜新术式的开展,内镜诊疗需求快速释放,中国消化内镜市场规模正不断扩大。目前,软式电子内窥镜仍是消化道癌症最主要的筛查和治疗设备。消化道癌前疾病和肿瘤的“早发现、早诊断、早治疗”逐渐成为共识。内镜下活检或切除标本的病理检查是消化道癌确诊的金标准,镜下切除癌前病变可降低消化道癌的发病率和死亡率。然而,据中国医采网2021年招投标数据,内窥镜领域国产品牌市场占有率不足10%,国内医院仍被进口品牌主导。国产厂家在镜体工艺、十二指肠镜、4K软镜、光学放大镜、超声内窥镜等细分技术领域仍亟待突破。据中信证券研究数据,软镜设备的国内市场容量快速增长,预计将于2025年达81.2亿规模,于2030年达到110亿规模。随着我国老龄化程度持续加深,消化道癌症早筛及诊断治疗需求将随之提升,其密切相关的软镜器械国产品牌将成为产业与市场关注的热点。同时,软镜作为兼具诊断和治疗功能的严肃医学产品,用户会非常重视产品的安全性和有效性,而科思明德这样具备多年医疗器械产业化积累,既能把握技术创新,又能保证产品质量与稳定性的企业会更加受到市场青睐。IDG资本表示,消化内镜是我们持续关注的医疗器械的大赛道,科思明德团队在这个领域有非常清晰的产品思路、成功的产品开发经验、全模块的自研能力,同时公司非常聚焦、富有创业精神和创新思维。我们很认同科思明德“普及创新内镜技术”的理念,提升消化道疾病的早筛、早诊和早治的渗透率。未来,IDG希望支持科思明德一起为消化内科提供更好的解决方案,创造更大的临床价值。同创伟业创始合伙人黄荔女士表示,上轮投资以来,科思明德在产品研发和团队建设上都取得了较大的进展。在临床端,专家们对公司推出的新一代内镜产品做出了很高的评价。另外,公司也储备了一些原创的创新管线。内镜领域此前被进口品牌垄断,在国产替代红利、中国智造整体提升的大背景下,我们期待科思明德这匹黑马,推动内镜赛道形成新的格局,并在其中成为领军品牌。我们相信,团队能持续开发出优秀产品,在国内和国外市场创造临床价值,为患者带来更多获益。国家高性能医疗器械创新中心副总经理刘恒博士表示,自国创中心上轮投资之后,科思明德在团队建设、产品研发、市场拓展准备等方面展现出了专业、高效、团结的作风和强大的战斗力,整体发展超出了我们此前的预期。国创中心持续看好软式内窥镜赛道以及国产厂家在其中的成长前景,在投资科思明德后已积极协助公司顺利落户深圳市龙华区全新场地,未来也将继续为以科思明德为代表的国内优秀医疗器械创新企业提供多维度、全周期的赋能,共同助力中国高端医疗器械产业发展。科思明德团队表示,感谢IDG资本的大力支持,同创伟业和国创中心等新老股东的再次助力。作为根植深圳的医疗科技公司,创新、专注、高效、合作、全球视野是目前科思明德的指导性方向。在未来,科思明德立志于以创新技术和先进理念,继续响应临床需求,赋能微创手术,普及先进内镜设备并开发更多创新性软镜产品,完善诊疗一体化解决方案。在未来,科思明德将力争成为国内软式内窥镜领军企业,以及国际一流的软式内窥镜整体解决方案提供商,在回馈投资方助力的同时,也造福广大的人民群众。关于IDG资本IDG资本于1993年起率先在中国开展风险投资业务,是中国历史最悠久的私募股权投资机构,也是中国管理资产规模最大的私募股权基金管理人之一。经过30年的发展,公司累计管理资产近2000亿人民币。多年来,IDG资本始终高度关注医疗健康领域的发展。在过去不到5年时间里,IDG资本在医疗领域出手了约70个项目,重点布局生物医药、器械诊断、人工智能等细分赛道,并关注政策驱动下创新医疗模式带来的机会。在生物医药领域,IDG资本不仅布局新药研发类企业,如科伦博泰、先为达生物、晟斯生物,同时也关注产业链上下游企业,如百奥智汇、臻格生物、南方模式生物、诺思格、凯瑞斯德等;器械诊断方面,IDG资本则投资了元心科技、汇禾医疗、康立明等项目;而在人工智能领域,IDG资本下注了长木谷和冰洲石等项目;由于密切关注着国家医保政策调整和医疗服务改革可能带来的机会,IDG资本从中发掘了微脉医疗、思派健康科技等明星项目。关于同创伟业深圳同创伟业资产管理股份有限公司(简称“同创伟业”)成立于2000年6月26日,是中国第一批本土专业创投机构。公司拥有超过22年的投资管理经验,管理超300亿人民币,陆续投资超过600家企业,100余家企业上市,其中科创板上市企业达到24家,是国内处于领先地位、运作时间长和回报持续优异的本土品牌专业投资机构。同创伟业以产业链投资为切入点,聚焦于新兴产业,专注于大健康、大科技、大信息、大消费等细分领域,在硬核科技以及前沿科技领域积累了丰富的投资经验,以稳健的投资策略深度挖掘隐形冠军,并以赋能式投资支持创新创业,全力服务实体经济。同创伟业以“创业企业的同行者,伟大企业的引路人”为理念,致力于以开放的心态与创业者、企业家同进步、共成长,做企业的“超级合伙人”。关于国创中心国家高性能医疗器械创新中心(简称“国创中心”)是由中国科学院深圳先进技术研究院、深圳迈瑞生物医疗电子股份有限公司、上海联影医疗科技股份有限公司、先健科技(深圳)有限公司和哈尔滨工业大学等单位牵头组建,于2020年4月获工业和信息化部批复建设,是深圳首个国家级制造业创新中心,也是国家在医疗器械领域设立的唯一的创新中心。国创中心围绕与医疗健康密切相关的预防、诊断、治疗、康复领域的高端医疗设备的重大需求,聚焦高端医学影像、体外诊断和生命体征监测、先进治疗、植介入器械、康复与健康信息等重点方向,致力突破行业发展的共性核心关键技术,完成技术开发、转移扩散到首次商业化应用各个环节,打造贯穿创新链、产业链和资金链的高性能医疗器械产业创新生态系统。近期推荐声明:动脉网所刊载内容之知识产权为动脉网及相关权利人专属所有或持有。未经许可,禁止进行转载、摘编、复制及建立镜像等任何使用。动脉网,未来医疗服务平台
临床3期医药出海
100 项与 广州康立明生物科技股份有限公司 相关的药物交易
登录后查看更多信息
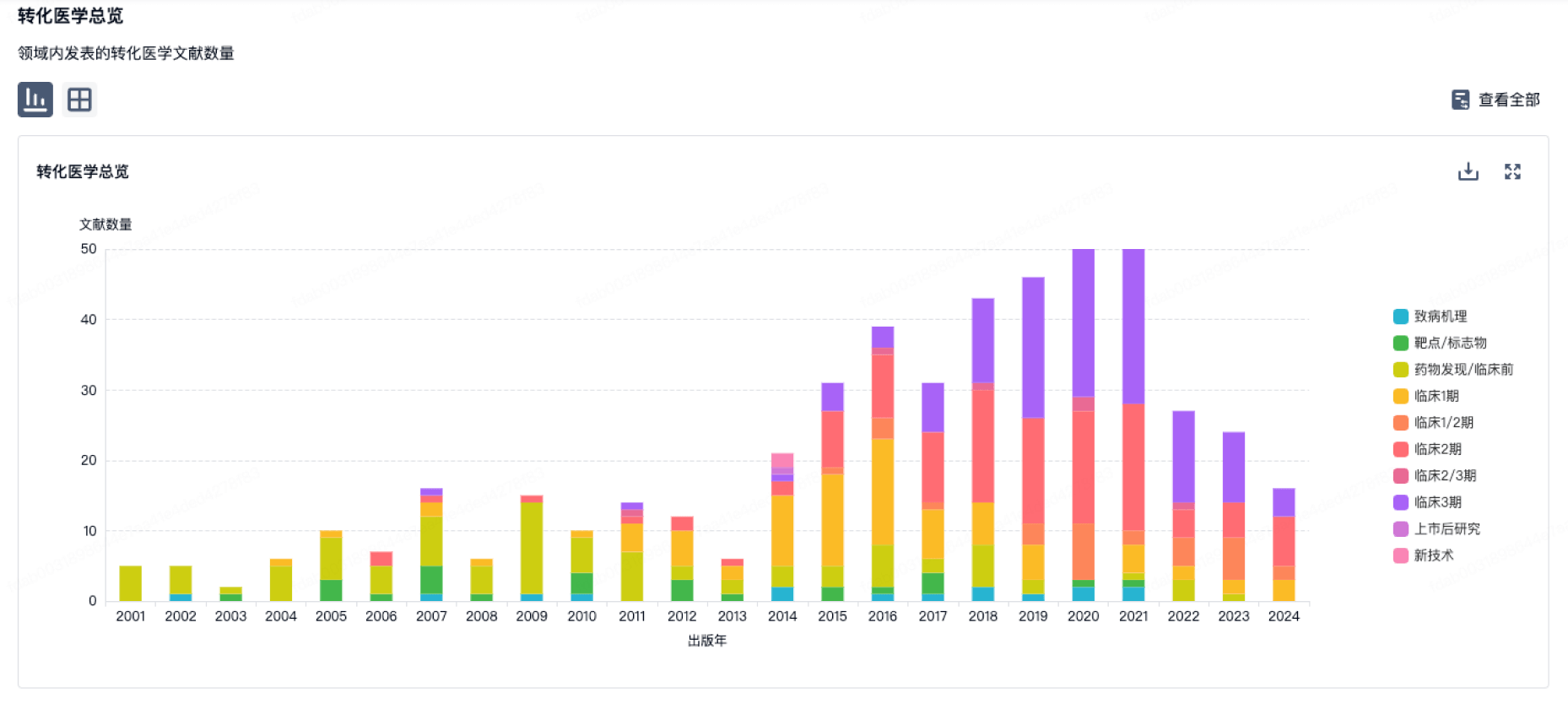
100 项与 广州康立明生物科技股份有限公司 相关的转化医学
登录后查看更多信息
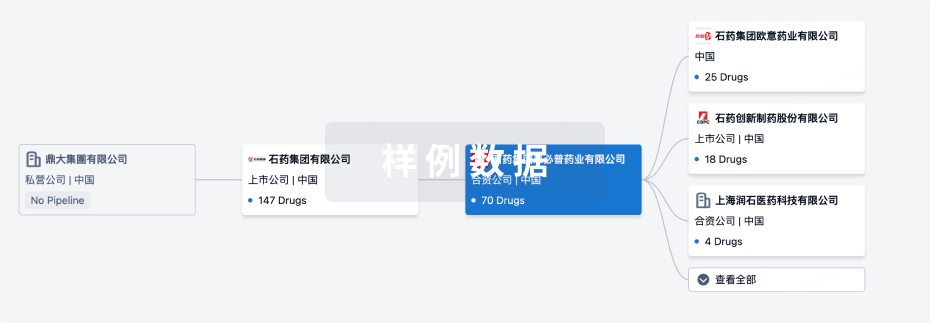
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年07月19日管线快照
无数据报导
登录后保持更新
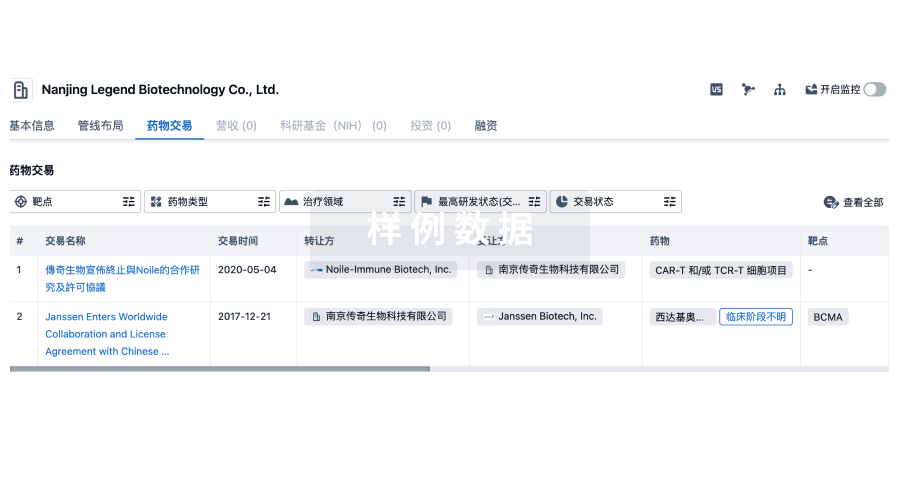
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
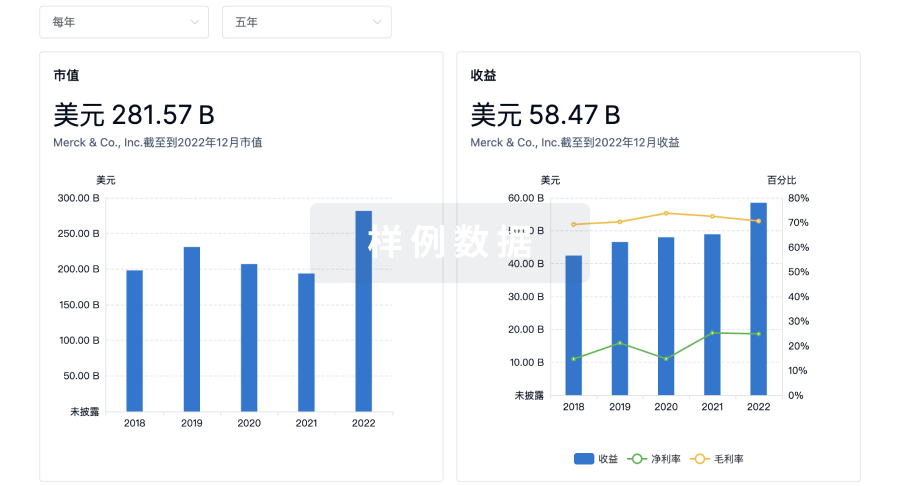
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用