预约演示
更新于:2025-05-07

HAN University of Applied Sciences
更新于:2025-05-07
概览
关联
30
项与 HAN University of Applied Sciences 相关的临床试验NCT06626360
SCreening fOr Malnutrition and Obesity in Patients With COVID-19 and Other Diseases
More than half of the Dutch population is overweight or obese, which is associated with an increased risk of COVID-19 and worse outcomes during a COVID-19 infection. In addition, malnutrition and loss of muscle mass are often reported with COVID-19, as well as with cancer and other diseases. Malnutrition and overweight or obesity can coexist, even within the same individual. It is still unclear which mechanisms contribute to the worse outcomes of COVID-19 and other diseases in case of overweight, malnutrition, and a combination of both. The aim of this study is to identify which parameters are associated with worse disease outcomes through literature research and database research (COVID-19 and cancer, more than 150.000 participants). In addition, a clinical study will be conducted aiming to develop a simple screening tool for the recognition of the coexistence of malnutrition and overweight or obesity in clinical practice.
开始日期2024-10-02 |
申办/合作机构 |
NCT06282757
The Effect of Physiotherapists' Placebo or Nocebo Communication About Virtual Reality on Treatment Beliefs in Patients With CMP
Rationale: Chronic musculoskeletal pain (CMP) is a common and disabling condition. Physiotherapy is the most frequently administered non-pharmacological treatment option for patients with CMP and recently virtual reality (VR) was introduced in physiotherapy care as a novel treatment modality. Proper communication about physiotherapy treatment (modalities) is important to improve treatment outcomes, by applying placebo effects enhancing communication and avoiding nocebo effects enhancing communication. However, yet is still unknown to what extent this applies to communication of physiotherapists about VR in patients with CMP.
Objective: To determine the effect of physiotherapists' placebo or nocebo therapeutic communication about VR, on treatment credibility and expectation in patients with CMP
Study design: Web-based randomized controlled trial.
Study population: 100 participants
Intervention: The placebo intervention group will be shown an educational video about VR, containing placebo effects enhancing verbal language. The nocebo intervention group will be shown an educational video about VR, containing nocebo effects enhancing verbal language.
Primary study parameters: The primary study parameters are treatment credibility and treatment expectation. Treatment credibility and treatment expectations will be measured using the Dutch credibility and expectancy questionnaire (CEQ).
Objective: To determine the effect of physiotherapists' placebo or nocebo therapeutic communication about VR, on treatment credibility and expectation in patients with CMP
Study design: Web-based randomized controlled trial.
Study population: 100 participants
Intervention: The placebo intervention group will be shown an educational video about VR, containing placebo effects enhancing verbal language. The nocebo intervention group will be shown an educational video about VR, containing nocebo effects enhancing verbal language.
Primary study parameters: The primary study parameters are treatment credibility and treatment expectation. Treatment credibility and treatment expectations will be measured using the Dutch credibility and expectancy questionnaire (CEQ).
开始日期2024-04-01 |
NL-OMON53210
The effect of collagen supplementation on human tendon protein synthesis - Collagen for tendon remodelling
开始日期2024-02-28 |
100 项与 HAN University of Applied Sciences 相关的临床结果
登录后查看更多信息
0 项与 HAN University of Applied Sciences 相关的专利(医药)
登录后查看更多信息
1,595
项与 HAN University of Applied Sciences 相关的文献(医药)2025-06-01·International Journal of Nursing Studies Advances
Nurses' self-efficacy and outcome expectancy in evidence-based practice: Translation, construct validity and internal consistency of the Dutch scales
Article
作者: Echteld, Michael ; de Vos, Annemarie ; Ramis, Mary-Anne ; Hoegen, Peter ; de Bot, Cindy ; Vermeulen, Hester ; Mokkink, Lidwine ; Demirçay, Derya
2025-06-01·Clinical Nutrition
Decoding unintentional weight loss: How the right questions make a difference
Article
作者: Borkent, Jos W ; de van der Schueren, Marian A E ; van der Meij, Barbara S
2025-06-01·Clinical Nutrition
The GLIM consensus approach to diagnosis of malnutrition: A 5-year update
Article
作者: Klek, Stanislaw ; Steiber, Alison ; Correia, M Isabel T D ; Evans, David C ; Mori, Naoharu ; Muscaritoli, Maurizio ; Schueren, Marian de van der ; Cuerda, Cristina ; Hiesmayr, Michael ; Jager-Wittenaar, Harriët ; Jáquez, Anayanet ; van Gossum, André ; Hasse, Jeanette M ; Wang, Jaw-Yuan ; Barazzoni, Rocco ; Carrasco, Fernando ; Mundi, Manpreet ; Shi, Han Ping ; Cruz Jentoft, Alfonso J ; Singer, Pierre ; Nyulasi, Ibolya ; Braz, Diana Cardenas ; Gonzalez, M Cristina ; Jensen, Gordon L ; Tappenden, Kelly A ; Schneider, Stephane ; Blaauw, Renee ; Jahit, Shukri ; Gramlich, Leah ; Fukushima, Ryoji ; Yu, Jianchun ; Compher, Charlene ; Hiki, Naoki ; Siltharm, Soranit ; Keller, Heather ; Mogensen, Kris M ; Fuchs-Tarlovsky, Vanessa ; Ng, Doris ; Cederholm, Tommy ; Pisprasert, Veeradej ; Winkler, Marion F ; Malone, Ainsley ; Pirlich, Matthias
100 项与 HAN University of Applied Sciences 相关的药物交易
登录后查看更多信息
100 项与 HAN University of Applied Sciences 相关的转化医学
登录后查看更多信息
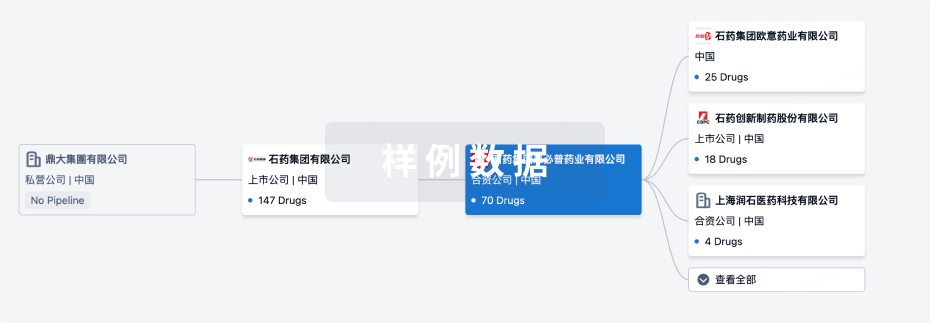
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年06月30日管线快照
无数据报导
登录后保持更新
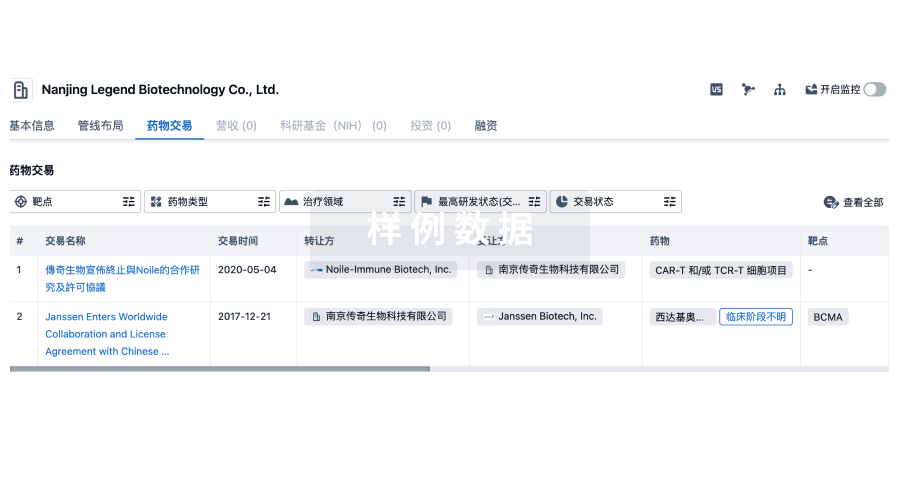
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
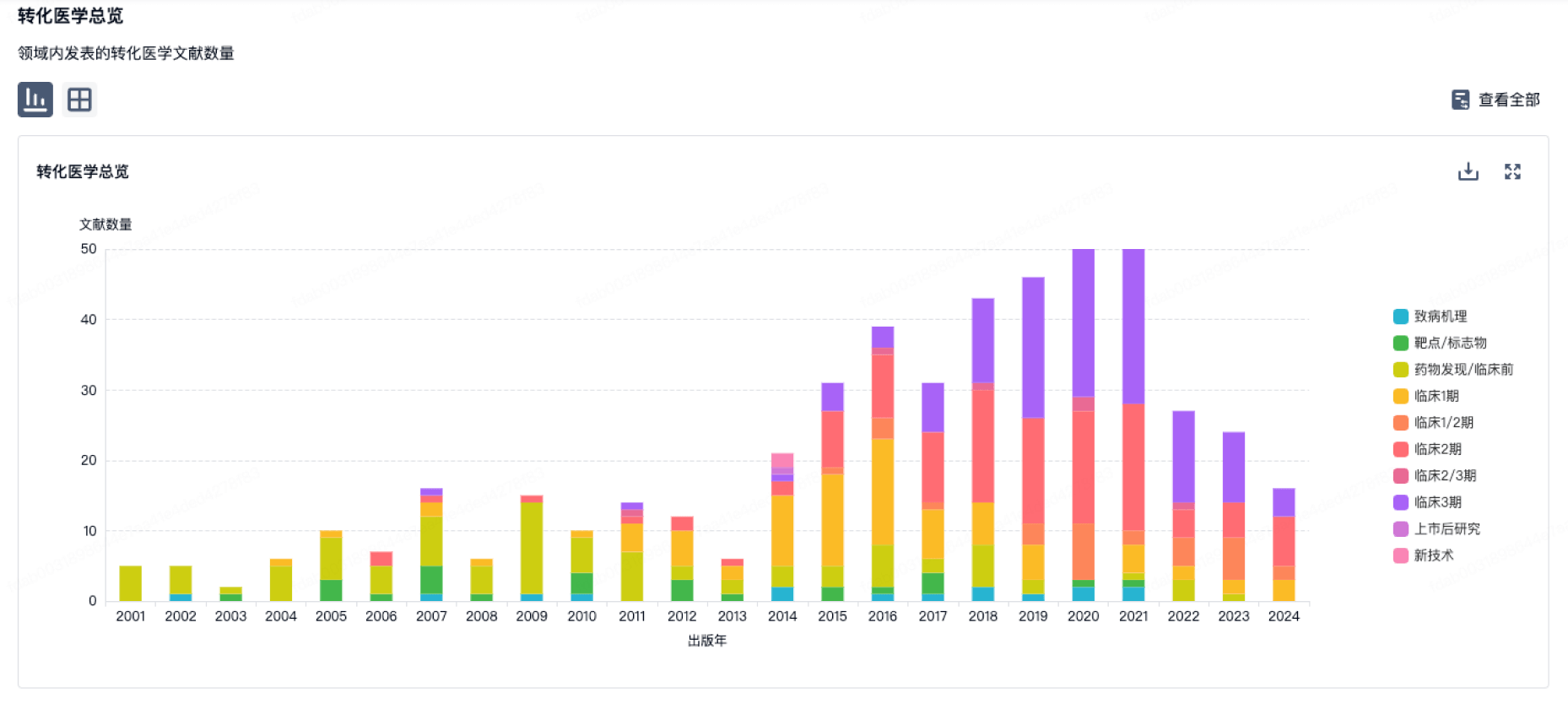
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
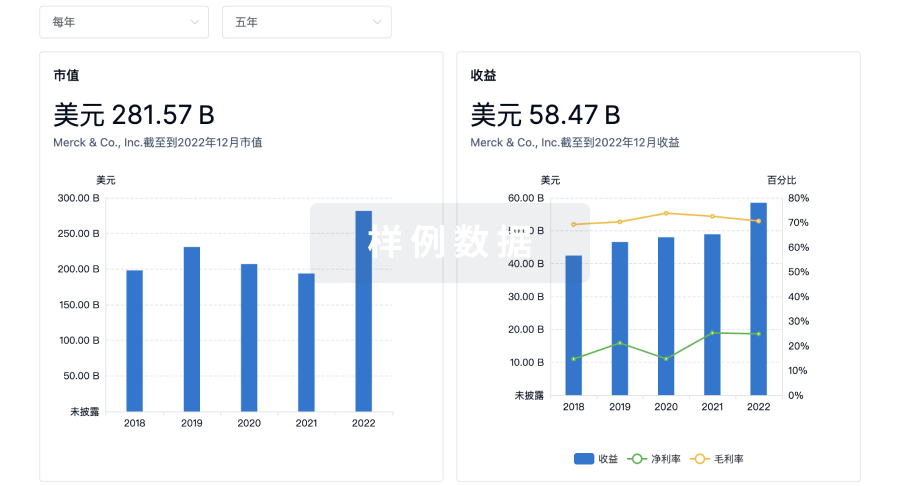
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用