预约演示
更新于:2025-05-07

Texas Scottish Rite Hospital for Children
更新于:2025-05-07
概览
关联
23
项与 Texas Scottish Rite Hospital for Children 相关的临床试验NCT06559215
Prospective Evaluation of Post-operative Pain Management Using Exparel in the Pediatric Population
The goal of this randomized clinical trial is to determine if administration of Exparel via local infiltration for medial patellofemoral ligament (MPFL) reconstruction procedures in pediatric orthopaedic sports medicine patients provides significant pain relief and decreased narcotic use. The main questions it aims to answer are:
* Does Exparel significantly reduce Visual Analog Scale (VAS) pain scores and pain levels up to one week postoperatively?
* Does Exparel significantly decrease narcotic use (number of pills taken) up to one week postoperatively?
Researchers will compare the pain outcomes and narcotic use of patients who receive Exparel and Marcaine via local infiltration to those of patients who receive only Marcaine via local infiltration for their MPFL reconstruction surgery. The goal is to understand if there is a significant difference in patient pain outcomes and narcotic use outside the first 24 hours postoperatively.
Participants will:
* receive either Exparel + Marcaine intraoperatively or Marcaine only intraoperatively during their MPFL reconstruction surgery
* receive and complete questionnaires at postoperative days 1, 4, and 7 regarding their pain scores, levels, and outcomes, effective pain treatments, overall pain interference, narcotic use (number of pills taken), and overall pain treatment satisfaction
* receive and complete secondary outcome measures of functional and psychological outcomes regarding their MPFL reconstruction surgery at postoperative day 1
* Does Exparel significantly reduce Visual Analog Scale (VAS) pain scores and pain levels up to one week postoperatively?
* Does Exparel significantly decrease narcotic use (number of pills taken) up to one week postoperatively?
Researchers will compare the pain outcomes and narcotic use of patients who receive Exparel and Marcaine via local infiltration to those of patients who receive only Marcaine via local infiltration for their MPFL reconstruction surgery. The goal is to understand if there is a significant difference in patient pain outcomes and narcotic use outside the first 24 hours postoperatively.
Participants will:
* receive either Exparel + Marcaine intraoperatively or Marcaine only intraoperatively during their MPFL reconstruction surgery
* receive and complete questionnaires at postoperative days 1, 4, and 7 regarding their pain scores, levels, and outcomes, effective pain treatments, overall pain interference, narcotic use (number of pills taken), and overall pain treatment satisfaction
* receive and complete secondary outcome measures of functional and psychological outcomes regarding their MPFL reconstruction surgery at postoperative day 1
开始日期2025-06-01 |
NCT06559137
Prospective Evaluation of Post-operative Pain Management Using Peripheral Nerve Blocks in the Pediatric Population
The goal of this randomized clinical trial is to determine if single-shot ropivacaine peripheral nerve blocks (PNB - perineural injections) for anterior cruciate ligament (ACL) reconstruction procedures in pediatric orthopaedic sports medicine patients provides significant pain relief and decreased narcotic use. The main questions it aims to answer are:
* Does ropivacaine significantly reduce Visual Analog Scale (VAS) pain scores and pain levels up to one week postoperatively?
* Does ropivacaine significantly decrease narcotic use (number of pills taken) up to one week postoperatively?
Researchers will compare the pain outcomes and narcotic use of participants who receive a single-shot ropivacaine peripheral nerve block to those of participants who do not receive a single-shot ropivacaine peripheral nerve block for their ACL reconstruction surgery. The goal is to understand if there is a significant difference in participant pain outcomes and narcotic use outside the first 24 hours postoperatively.
Participants will:
* receive either a single-shot ropivacaine peripheral nerve block intraoperatively or no peripheral nerve block during their ACL Quadriceps tendon graft or bone patellar tendon bone graft reconstruction surgery.
* receive and complete questionnaires at postoperative days 1, 4, and 7 regarding their pain scores, levels, and outcomes, effective pain treatments, overall pain interference, narcotic use (number of pills taken), and overall pain treatment satisfaction
* receive and complete secondary outcome measures of functional and psychological outcomes regarding their ACL reconstruction surgery at postoperative day 1
* Does ropivacaine significantly reduce Visual Analog Scale (VAS) pain scores and pain levels up to one week postoperatively?
* Does ropivacaine significantly decrease narcotic use (number of pills taken) up to one week postoperatively?
Researchers will compare the pain outcomes and narcotic use of participants who receive a single-shot ropivacaine peripheral nerve block to those of participants who do not receive a single-shot ropivacaine peripheral nerve block for their ACL reconstruction surgery. The goal is to understand if there is a significant difference in participant pain outcomes and narcotic use outside the first 24 hours postoperatively.
Participants will:
* receive either a single-shot ropivacaine peripheral nerve block intraoperatively or no peripheral nerve block during their ACL Quadriceps tendon graft or bone patellar tendon bone graft reconstruction surgery.
* receive and complete questionnaires at postoperative days 1, 4, and 7 regarding their pain scores, levels, and outcomes, effective pain treatments, overall pain interference, narcotic use (number of pills taken), and overall pain treatment satisfaction
* receive and complete secondary outcome measures of functional and psychological outcomes regarding their ACL reconstruction surgery at postoperative day 1
开始日期2025-06-01 |
NCT06048419
Acceptability and Efficacy of GO MOVE: A Mobile Health Technology for Youth With Unilateral Cerebral Palsy
The goal of this clinical trial is to learn about the acceptability and efficacy of Go Move, a mobile website developed to assist youth with unilateral cerebral palsy and their caregivers with setting goals and selecting exercises and activities to meet the goals. The main question[s] it aims to answer are:
* Is Go Move accepted by youth with unilateral cerebral palsy and their caregivers?
* Does Go Move support goal attainment for youth with unilateral cerebral palsy?
Participants will set up and participate in a goal-driven home program using the Go Move mobile website. Participants will spend 1 hour and 15 minutes per week for 6 weeks working on their home program and will complete pre-intervention and post-intervention assessments.
* Is Go Move accepted by youth with unilateral cerebral palsy and their caregivers?
* Does Go Move support goal attainment for youth with unilateral cerebral palsy?
Participants will set up and participate in a goal-driven home program using the Go Move mobile website. Participants will spend 1 hour and 15 minutes per week for 6 weeks working on their home program and will complete pre-intervention and post-intervention assessments.
开始日期2024-02-20 |
100 项与 Texas Scottish Rite Hospital for Children 相关的临床结果
登录后查看更多信息
0 项与 Texas Scottish Rite Hospital for Children 相关的专利(医药)
登录后查看更多信息
1,398
项与 Texas Scottish Rite Hospital for Children 相关的文献(医药)2025-05-12·Brain Injury
Endophenotype presentation of athletes with concussion contingent on sex and time since injury
Article
作者: Cullum, C Munro ; Beitchman, Joshua A ; Chung, Jane S ; Stokes, Mathew ; Didehbani, Nyaz ; Miller, Shane M ; Hynan, Linda S ; Jones, Jacob C
2025-03-01·Spine Deformity
Spine deformity surgery in patients with Beals syndrome can be effectively performed but does risk revision surgery
Article
作者: Datcu, Anne-Marie ; Thornberg, David ; Booth, Anna ; Sucato, Daniel J ; Sucato, Daniel J.
2025-03-01·Clinical Orthopaedics & Related Research
Clinical Faceoff: The Role of Elective Bilateral Lower Limb Lengthening for Gaining Height
Article
作者: Birch, John ; Sabharwal, Sanjeev ; Paley, Dror
2
项与 Texas Scottish Rite Hospital for Children 相关的新闻(医药)2024-03-11
导读在科学的广袤星空中,一颗璀璨的女性之星闪耀其中。 她不仅在自己的科研领域取得了卓越的成就,更在生命的旅途中传承了爱与希望。从获得美国最高工程荣誉,到成为获诺贝尔奖的女性科学家,她的每一步都充满了坚韧与勇气。 然而,这位伟大的科学家更是一位深爱着家人的母亲,她经历了接连两任丈夫去世、丧子,自己还得了乳腺癌,却在如此困难的情况下,将科学事业迈向了新的高度。 本文来自Arnold在诺奖官网自述。今天让我们一同走进这位传奇女性的世界,感受她的非凡之旅。01热爱冒险与挑战的童年1956年7月25日,我出生在宾夕法尼亚州的东匹兹堡,我的母亲经过24小时的艰苦分娩,才将我生下来,然而出生时我看起来整个人变形且没有头发。父亲称呼我为他的“天鹅”(直到青春期时,这个昵称被“Vampira”所替代)。 当时,我25岁的父母威廉·霍华德·阿诺德(William Howard)和约瑟芬·因曼·鲁索(Josephine Inman Routheau)已经有一个两岁半的儿子比尔(Bill)。我出生13个月后,爱德华(Edward,一个可爱的小惊喜)也出生了,接着是大卫(David),最后是我12岁、足够独立照顾婴儿时,托马斯(Thomas)也来到了这个世界。 这群男孩(包括我自己)通常由比尔指挥,比尔和我父亲以及我祖父同名,祖父威廉·霍华德·阿诺德(William Howard Arnold)将军曾在二战期间的太平洋战区为美国军队效力,战后指挥美国驻奥地利军队,后来以美国第五军军长的身份退休。 我们是一个庞大的天主教家庭,家里的许多人至今仍会聚集在密歇根湖东岸的麦卡塔瓦的避暑别墅里。家里的女性掌管着一切,她们在家中将一切安排得井井有条。多年来,我们和祖父母一起住在他们建于世纪初的别墅“Stack Arms”里,和不同的表亲住在一起,直到1965年父亲建造了自己的房子。我的祖父,那位强大的将军,在他深爱的、更具威严的妻子伊丽莎白·威尔士·马伦(Elizabeth Welsh Mullen)于1976年因乳腺癌去世后,仅几周就因心碎而去世。 密歇根州的麦卡塔瓦对我来说是天堂,因为我可以自由地到处跑,有时成群结队,有时独自一人。有一天,妈妈看到码头尽头丢着我的三轮车,差点吓出心脏病来。人们最后在码头下找到我,当时我正在挖小龙虾。几年后的一个夏天,我不得不打消建造木筏横渡密歇根湖前往芝加哥的念头——那可是九十英里的距离。我在密歇根湖上学会了扬帆,学会了尊重自然、利用自然的力量。 在那个没有电视和网络的时代,书籍、自行车和朋友成了我们的乐趣所在。我阅读了父亲珍爱的《Analog Science Fiction and Fact 》杂志旁边的那一摞堆1950年代的《读者文摘》杂志的每一期。我尤其着迷于那些报道奇迹般的手术将断肢重新接上的文章。我曾幻想着追随我的早期偶像克里斯蒂安·巴纳德博士(Christiaan Barnard)——他在1967年进行了首例人体心脏移植手术。在一个夏天里,我把当地荷兰公共图书馆里所有能找到的医学书籍都翻了个遍。但当我发现自己仅仅是看到血就会感到恶心时,我就放弃了成为移植外科医生的念头。 图1. 1961年,Frances 夏天是美好的,但在匹兹堡的上学时光却又是另一番景象。20世纪60年代,没有人知道该如何应对一个聪明的小女孩。为了让我忙碌起来,父母让我学音乐(钢琴和小提琴),做各种各样的缝纫和艺术项目,学习滑冰——这意味着在寒冷的天气里步行一英里多去溜冰场——以及步行去威尔金斯堡上星期六的教理课,无论风霜雨雪。我尽可能多地待在户外,在石头下寻找蝾螈,并找到和收集用过的汽水瓶,然后拿到当地的杂货店换两美分。三个瓶子可以换一根冰棍。我带着弟弟去探险,探索大型排水管;如果因为经常因四英尺厚的积雪而停课无法探险时,我们就会坐在圆形的电视机前看《I Love Lucy》的重播,玩无穷无尽的战争游戏。 图2. 1961年,战争游戏Eddy,Frances and Bill 我父亲是一位实验物理学家,1955年以24岁的年龄从普林斯顿大学获得博士学位,1954年他在科罗拉多州埃文斯山顶进行实验。母亲对这样一个偏远的地方(海拔10700英尺)并不满意,因此在比尔出生前不久,他们搬下山来到了爱达荷州斯普林斯(海拔7500英尺)。在那里,我的父母都感染了脊髓灰质炎,并不得不在铁肺中度过一段时间,由我那无所畏惧的外祖母约瑟芬·鲁索(Josephine Routheau)照顾。毕业后,父亲放弃了学术研究,投身新兴的核工业。位于匹兹堡的西屋电气公司打算提供“便宜到无法计量的电力”,而我父亲则协助设计了实现这一梦想所需的压水反应堆技术。 20世纪60年代,我的父亲经常不在家。他似乎经常呆在内华达州;后来我才知道,那是为了进行核试验。他会从赌场给我们带回银元,因为他必须陪大老板们去赌场豪赌。他在家时,喜欢建造房子或制作飞机模型、听古典音乐、阅读,以及整理硬币和邮票收藏。我认为他是世界上最聪明的人,因为他知道所有的答案,能解释一切事物的运作原理,几乎什么都能修好。为了和他共度时光,埃迪和我竞相收集邮票的复制品。我们分配了世界版图:我负责英国殖民地;埃迪则负责世界其他地区。从集邮中,我学到了地理知识,了解到地理边界、政府,甚至语言都会随时间发生变化。我还了解到帝国的兴衰,以及前殖民地如何获得独立。 02求学生涯,学会自立以及结缘科学我在小学时的出色表现让我得以进入打字班。十岁时,我远超同班同学,大部分时间都在画画,为朋友们制作小纸人,以及完善我的镜像书写(身为左撇子的我,很容易写出反字,当朋友们将我的加密信息举到浴室镜子前时,总能给他们留下深刻印象)。我的父母不知怎么竟然说服了埃奇伍德小学,允许我到隔壁的高中上一些课程。我最喜欢的额外课程之一是打字,尽管我并不擅长。我踩在两本电话簿上才能够到打字机,而高中生们看着这个身材矮小、双腿悬在座位上的五年级学生,忍不住哈哈大笑。我至今仍保留着在课上给爸爸打的信。我还学习了机械制图,这门课同样具有挑战性,但它教会了我从不同角度观察和描述物体的重要技能。 到13岁时,我已经对课堂学习感到厌倦了。那是1969年,我们当时居住的巴尔的摩市正经历着动荡。我没能被那所私立女子学校邀请回去上九年级,尽管我妈妈费了很大劲才让我入学,但我本来就很讨厌那里。于是,我开始搭便车前往华盛顿特区的反战抗议活动。在父亲将我们带回匹兹堡之前,我只在市中心的一所大型公立高中上了半个九年级。搬回北方只是延长了我参加抗议活动的时间。 在匹兹堡松鼠山社区的一所优秀公立学校阿勒德里斯中学,我选择了意第绪语作为我的第二外语(仅次于法语),并乐在其中,因为相比于天主教文化里那些沉闷的描述,它提供了一套全新的、更加丰富多彩的表达方式。作为一个需要了解世界但缺乏驾驭能力的青少年,我渐渐与同学和父母疏远。我独自居住在一个破旧、糟糕、虫害肆虐的三楼公寓里,身处一个充满污垢的社区,我做过各种各样的工作来支付房租和账单,同时梦想着有一天能摆脱上世纪六七十年代作为年轻女性的局限。我做过的工作包括:卖种子(没错,我10岁那年就赚到了一辆自行车)、午餐柜台女服务员(14岁)、披萨店助手(15岁)、百货公司店员(16岁)、接待员(16岁)、酒吧女服务员(17岁),我告诉他们我22岁,从来没人查,因为那时年轻人很少有证件)、匹兹堡著名爵士乐俱乐部沃尔特·哈珀阁楼的女服务员,最后还做过出租车司机(18岁)。在我离家上大学之前,我已经能够熟练地在匹兹堡陡峭的山丘和坑坑洼洼的街道上驾驶一辆庞大的六十年代黄色出租车。那些街道比我开的出租车还窄,但我的顾客坚持认为我能通过,他们(通常)是对的。在没有GPS的情况下,我在脑海中构建地图,至今仍然受益于那时培养的方向感。开出租车是一项艰苦的工作。 那时,有时一天工作超过十个小时,只能挣到二十或二十五美元,但仅仅几周时间,我就从调度员给新司机的那些肮脏、破损的出租车升级到了干净、较新(但仍然一样宽)的出租车,小费也因此变得更多。然而,乐趣必须结束,因为我要去上大学了。 1974年,我设法说服了普林斯顿大学的招生官员,最终被录取。我想或许是因为我的申请文书写得很令人信服,或许是因为我是申请工程学的女生中非常罕见的一个,但也可能我父亲曾在该校获得物理学博士学位并且与工程学院院长交情匪浅也起了一定作用。1974年我入学时,普林斯顿大学才开始有女生毕业,因为该校直到1969年才开始招收女生。我那一届的学生中女生大约占了15%,而机械工程学和航天工程学的女生就更少了。不过,作为唯一的女生对我来说早已习以为常,我没有理由转到其他专业,于是留在了机械工程学和航天工程学系。我忙着吸收尽可能多的知识和新思想:意大利语、经济学、社会主义理论、俄语及文学、艺术史,以及大量的数学和物理学知识。我对化学不感兴趣,这在我的大一成绩中有所体现,因此当时我在化学方面没有取得什么进步。 在普林斯顿大学,我继续开出租车,在图书馆工作,组装电子设备,还为哲学家托马斯·S·库恩(Thomas S. Kuhn)打扫房子。我需要钱来支持我在莱克航空公司机票的费用,只要愿意在凌晨4点去曼哈顿的售票处排队,当天午夜左右就能以99美元的价格飞往伦敦。在普林斯顿大学的最后两年里,我每逢假期都去伦敦、意大利或巴黎游玩。 旅行打开了一个充满不同文化和美食的迷人世界(我热爱人们在食物上的创造力,并很高兴地发现日常食物可以如此美味)。高中三年级(1973年)结束后,我的外祖父母带着我的哥哥比尔和我去了欧洲旅行。他们多年来一直游历欧洲,前往他们钟爱的奥地利、德国、法国和意大利的小镇。我们在路上花了整整两个月的时间,从未在任何地方停留超过两晚。每个人都似乎认识并喜爱我的外祖父母爱德华上校和约瑟芬夫人。他们教我如何用很少的钱享受生活。“妈妈”和“爸爸”的秘诀是:在法国南部乡村小路边阳光照耀的草地上,享用一瓶葡萄酒、一个新鲜法式长棍面包和一点肉酱。 于是,我渴望重返欧洲,亲自体验那里的风土人情,我于1976年至1977年间,在普林斯顿大学读完大二后抽出时间,前往马德里和米兰工作。在此期间,我从不说英语,也发现了全新的文化和朋友。我和我的意大利男友骑着摩托车遍游意大利北部,夏天,我们骑着他的1956年款摩托古兹500(意大利宪兵队的经典车型)一路前往伊斯坦布尔,然后又原路返回。在还没有铺设公路的时候,我们就去了五渔村,在农民的家里搭帐篷或者睡觉。我弹着吉他,与愿意倾听的人分享鲍勃·迪伦(Bob Dylan)和意大利的弗朗西斯科·古奇尼(Francesco Guccini)的歌曲。 在普林斯顿大学最后两年,我重新燃起了对完成学业和寻找有意义的事情做的热情,以前那种对课程漫不经心的态度发生了改变。我热爱高年级的课程,并发现只要稍加努力,我在数学和工程学方面确实有天赋;1979年,我以优异的成绩获得了机械与航天工程学位。20世纪70年代的能源危机,以及普林斯顿大学导师们将科学与社会利益相结合的激情,激发了我对替代能源的终身兴趣。 毕业后,我再次背上背包,带着每天2美元左右的储蓄,从厄瓜多尔出发,前往巴西圣保罗,跟随后来成为巴西环境部长和乙醇燃料计划“之父”的若泽·戈尔德姆伯格(José Goldemberg)教授,在太阳能项目上进行实习。我乘坐公共汽车,沿着印加古道,用了六个星期的时间,从厄瓜多尔的瓜亚基尔前往玻利维亚的圣克鲁斯。从利马到阿亚库乔的行程超过36个小时,我们在崎岖的山路上缓慢攀登,还与一只身上长满跳蚤的山羊共用这辆公交车。我们似乎每小时都要停下来一次,因为联邦警察正在路检,他们会让我们下车,对我的护照感到困惑不解,几小时后才让我们继续前行。我喜欢秘鲁,但不喜欢那的食物,经常导致我食物中毒。那个夏天,我练成了在任何地方都能睡觉的本领,并增强了我的免疫系统。在巴西期间,我学会了一点葡萄牙语,还养成了对食堂每天午餐供应的豆子和米饭的喜好,尤其是周日中午供应的传统黑豆烩肉,这道菜需要一整天的时间来消化。 凭借机械工程学位以及卡特政府对于清洁、可再生能源的重视,我迎来了第一份“正式”工作(1979年至1980年),地点位于科罗拉多州戈尔登市的一个新兴国家实验室——太阳能研究所(现在更名为国家可再生能源实验室)。在弗兰克·克雷斯(Frank Kreith)的传热小组中,我的主要工作是开发新型被动式太阳能加热和冷却技术;我还帮助联合国撰写关于发展中国家太阳能问题的立场文件。在办公室之外,我学习如何驾驶越野摩托车,并提高了滑雪技能,这项技能是我在意大利居住时首次尝试的。作为交换,我住在一家马场,并在主人外出时照顾动物,以此换取免费住宿。为了对抗从每个电台传来的乡村西部音乐的猛烈冲击,我开始学习古典吉他。 031981年至1985年,加利福尼亚大学伯克利分校 随着罗纳德·里根(Ronald Reagan)当选为美国总统,被动式太阳能加热和冷却技术的未来似乎有些渺茫。我从未去过加利福尼亚州,但在1980年底,我把我寥寥无几的行李装进了我的1971年款红色大众甲壳虫,然后向西出发,开始在加利福尼亚大学伯克利分校攻读研究生。那里的化学工程师们决定冒险接纳一名既是女性又是机械工程师的学生,我于1981年1月被录取为博士研究生。 图3. 加利福尼亚大学伯克利分校化学学院,1984年 尽管我最初的想法是从事纤维素生物燃料的研究,但后来对该技术的兴趣已经减弱:汽车再次变得庞大,石油禁运也被人们遗忘。我们也忘记了如何关爱地球。替代能源项目的资金变得稀缺;我原本打算跟随的那位教授退休了;我不得不改变方向。然而,出生于澳大利亚、刚从特拉华大学被招募到伯克利分校的哈维·布兰奇教授(Professor Harvey Blanch),却准备支持即将兴起的一个全新行业——生物技术行业。加利福尼亚州和波士顿正在发生一场革命——像“基因泰克”(Genentech)和“安进”(Amgen)这样的新公司正在寻找工程师,希望利用重组DNA技术扩大生产蛋白质药物的工艺规模。需要有人生产和提纯这些重组蛋白,它们有望改变医学的面貌。 图4. 1981年,我在内华达山脉徒步旅行 于是,我开始从事生物分离领域的研究,学习亲和色谱法,并开发和验证色谱分离的数学模型。我也逐渐认识到与蛋白质打交道所面临的挑战:一切工作都围绕着让蛋白质保持稳定进行。这并不容易,因为蛋白质的稳定性只是勉强维持,似乎稍有刺激就会变性。此外,大多数蛋白质治疗药物涉及高度复杂、翻译后修饰的结构,在制造、纯化或储存条件不当的情况下,这些结构很容易变得无用。工艺工程师对蛋白质或生物化学知之甚少,而标准的化学工程分离工艺也不适合蛋白质的保存。 研究生院就像大学一样,是另一场学习的盛宴,但这次涉及的是有机化学、生物化学、免疫学、酶学、高等数学,当然还包括整个本科和研究生化学工程的课程。有机化学对我来说很容易理解——制造分子就像拼拼图一样。在修完这门课并获得学分后,我很高兴地旁听了多门有机化学课程,并担任学生运营的“黑闪电”笔记服务(该服务深受那些害怕早起上8点课的学生喜爱)的官方笔记员。杰出的生物化学家杰克·基尔施(Jack Kirsch)和朱迪思·克林曼(Judith Klinman)从定量和物理化学的角度向我介绍了酶惊人的催化能力,这尤其让我欣赏,而艾伦·威尔逊(Allan Wilson)则向我介绍了蛋白质序列的分子进化。我如饥似渴地吸收新知识,只为享受学习科学和数学课程的乐趣,这种习惯我几十年后仍在保持。 直到我研究生阶段的最后一年,我才想到尝试做一名教授。我曾与加州大学伯克利分校化学学院的一些年轻教授一起打牌和背包旅行,但对于教授的实际工作内容,除了教一两门课程外,我几乎一无所知。然而,我的博士导师哈维·布兰奇(Harvey Blanch)不仅创立了公司,还为工业界提供咨询,生物化学教授中也有一些人这样做,这种多元化的活动使我对学术事业产生了更浓厚的兴趣。我渴望与现实世界建立联系,同时也渴望获得我在之前各种工业和国家实验室职位中未曾体验过的独立。因此,我决定申请学术职位。1984年是申请学术职位的好时机:美国大学开始意识到,尽管越来越多的女性对科学和工程感兴趣,但工程学院的教师队伍中几乎没有女性。当时,化学工程师在开始学术生涯之前并不做博士后研究,我收到了包括麻省理工学院在内的许多优秀学校的职位邀请。1985年,我接受了明尼苏达大学的职位,该校化学工程排名全国第一。同时,我也利用众多工作邀请,获得了加州大学伯克利分校生物物理化学家伊格纳西奥·蒂诺科(Ignacio Tinoco)为期一年的博士后研究资金,以学习我认为将来会在实验室中使用的生物分子表征光谱方法,那时我29岁。 大约在那时,我遇到了杰伊·贝利(Jay Bailey),他是加州理工学院(Caltech)一位世界闻名的生物化学工程教授。加州理工学院是位于美国南加州的一所小型私立学院,我对它知之甚少。其化学工程系的教师人数很少,在工程领域则以非常“学术化”的研究而著称。加州理工学院的博士毕业生往往成为教授,而不是行业领袖。鉴于明尼苏达大学无法容纳贝利这样的优秀人才,我便向加州理工学院申请了助理教授职位。1987年,在麦克塔瓦(Macatawa)朋友的陪伴下(还有家人的陪伴),我和杰伊喜结连理。 04加州理工学院定向进化研究(1986-2003) 1986年年中,我搬到了加州理工学院,担任博士后研究员的临时职位(我的正式头衔是“客座研究员”,因为当时我已经是明尼苏达大学的助理教授)。我很高兴能在杰克·理查兹(Jack Richards)的实验室里拥有一席之地,在那里我将学习如何设计蛋白质的序列,这是我为自己的研究所需要的技术。杰克最近开发了一种名为“盒式诱变”的技术,这是蛋白质工程的第一批定点诱变方法之一。我第一次涉足分子生物学和基因工程,是为哈里·格雷(Harry Gray)的课题组制作了几种突变的细胞色素c蛋白,他们想用这些蛋白来探索生物电子转移。1986年一切都很难:合成寡核苷酸、DNA测序、克隆以及使用限制性内切酶都存在问题,而我排查克隆实验故障的经验也非常有限。但我坚持不懈,当我的第一个突变序列得到确认时,我成为了一名自豪的蛋白质工程师。 幸运的是,加州理工学院的两名化学工程教授另谋高就,这为新成立的“生物”化学工程部分空出了一个初级职位;我收到了加入教师团队的邀请,并于1987年1月开始担任加州理工学院化学工程助理教授。 杰伊·贝利(Jay Bailey)的实验室是第一个,或者至少是第一批使用分子生物学方法来解决工业生物技术问题的化学工程实验室之一。杰伊自己的教育和研究背景仅限于化学反应系统的数学建模,但他出色地展示了如何借助无畏的研究生将新技术引入实验室。他吸引了来自世界各地的最优秀的学生到加州理工学院,我感激地从这些杰出的人才中招募人员,以组建我自己的蛋白质研究团队。多年来,我不断磨练自己,提醒研究生和博士后,他们可以学习和做到任何事。新的阿诺德实验室将确保蛋白质工程成为化学工程的一部分,就像杰伊和其他人正在做的代谢工程一样。这些早期对生物系统进行基因工程的努力,为现在所谓的“合成生物学”奠定了重要且具有工业相关性的基础。 问题在于,当时确实没有人知道如何制造有用的蛋白质。蛋白质,尤其是酶,令人着迷,人们发现它们具有很多用途,从监测血糖水平到清除衣物污渍。然而,化学工程师(以及其他人员)在使用蛋白质进行工业应用时面临的一个主要问题是,蛋白质无法在非自然条件下发挥功能。蛋白质在脱离自然环境后,其性能通常较差,工程师必须开发出鲁布·戈德堡式的机制来提纯、储存和使用蛋白质。不过,随着蛋白质序列工程技术的发展,以及蛋白质属性的随之改变,20世纪80年代首次出现了按照过程工程师或工业生物技术专家的要求来设计蛋白质本身的可能性。我的团队将致力于设计蛋白质序列,让蛋白质按照特定过程或应用的要求发挥作用,而不是围绕蛋白质来设计过程或应用。 我还想证明,蛋白质可以通过工程改造获得一些不寻常但有用的属性,从而开拓全新的应用领域。麻省理工学院的亚历克斯·克利巴诺夫(Alex Klibanov)在20世纪80年代震惊了全世界,他证明酶在悬浮于干燥的非极性溶剂中也可以发挥作用。然而,将酶溶解在高浓度的极性溶剂中,会立即导致其失去活性,即使可以证明它们仍保持着折叠结构。当时的主流观点是,蛋白质无法表现出高度非自然的属性,例如在有机溶剂中发挥作用的能力。似乎有一种观点认为,因为自然界从未这样做过,所以人类也不可能做到。但事实上,正因为如此,我们才有可能做到,甚至可能很容易做到。因此,我接受了这一挑战,即改造酶,使其能在极性有机溶剂中催化反应,但当时没有人知道如何改变它们的序列来实现这一目标。我尝试通过“理性设计”为有机溶剂设计酶,但均以失败告终,当时旨在改进蛋白质的大多数实验也均以失败告终。虽然很容易削弱甚至破坏酶的功能,但很少有报道称能够制造出更好的酶。这个过程非常困难——需要获得酶的晶体结构(其中非常少),然后充分理解蛋白质的结构和功能,不仅要识别出有用突变的位点,还要确定应该放置哪些氨基酸。 在20世纪80年代,一些实验室开始利用噬菌体展示和其他方法,对核酸、肽甚至蛋白质进行工程改造,从而构建出庞大的生物分子库。随后,他们通过结合测定或遗传筛选等方法对这些生物分子进行筛选,以找到有用的序列。我充分认识到蛋白质的复杂性以及针对多个突变位点进行改造时序列可能性的组合爆炸,同时考虑到有益突变发生频率可能很低。因此,我开发出一种适合我感兴趣的问题——改进酶类性能的替代方法,这种方法具有高度的通用性。我们采用了一种新开发的简单方法,即在特定基因中随机制造突变,即易错条件下的聚合酶链式反应。我和我的学生们制造了基因库,其中的基因只在一个或两个位点上随机突变,随后使用平板或96孔板读取器上的快速测定法,对它们进行筛选,以找到我们想要的特性。然后,我们会选取最佳蛋白质的基因,并重复这一过程以积累优势,逐步进化蛋白质,直到实现功能目标。 令我欣喜的是,在我们实验室里通过进化得到的酶中出现了有益且令人惊讶的突变。有益突变并不罕见,只要我们精心控制筛选过程,就能找到它们,并且我们可以累积这些突变以进一步改进酶的性能。当我们将这些突变映射到蛋白质结构上时,惊讶地发现它们经常发生在酶的表面上,而当时蛋白质化学家们认为突变效应大多是中性的。激活突变也出现在远离酶活性位点的位置,没有人能够解释它们的作用,更不用说事先预测它们了。到1990年,我们终于走上了利用进化作为指导来改造有用酶的道路。 另一个值得纪念的时刻是,1990年4月,我的第一个儿子詹姆斯·霍华德·贝利(James Howard Bailey)诞生了。当时我34岁,尚未获得终身教职,工作繁重,但我有一个可爱的儿子,精力充沛,而且清楚地知道自己应该往哪里走。 然而,并非所有人都赞同我的方法。蛋白质工程领域主要根植于生物化学,非常注重“理性设计”。蛋白质化学家们认为,他们可以通过结构引导的方法和甚至计算方法来预测有益的突变和序列。我的一些加州理工学院化学系的同事,对当时流行的“组合化学”不屑一顾,这种方法涉及合成和筛选大量分子库以寻找药物候选物,他们认为我的随机诱变研究是智力上的懒惰。然而,我并未因此动摇,因为我有一个行之有效的方法。 当我在蛋白质工程领域终于步入正轨时,实验室之外的生活却陷入困境。我的婚姻破裂,杰伊前往瑞士,成为苏黎世联邦理工学院的一名教授。 加州理工学院伸出援手,在经济上给予我支持,帮助我带着一岁大的孩子在帕萨迪纳的一栋我负担不起的房子里独立生活。对此,我将永远心怀感激。加州理工学院教务长保罗·詹宁斯(Paul Jennings)和校长托马斯·埃沃哈特(Thomas Everhart)也在我艰难的终身教职评定过程中给予帮助,向我展示了真正的领导力意味着什么:真正的领导者拥有道德指南针,有时需要做出违背权势人物意愿的决定。获得终身教职后,我可以全身心投入到我最热爱的工作中,即通过定向进化来改造酶。我放弃了所有与蛋白质-金属识别相关的其他项目,这些项目曾是我物理化学训练背景下更具“标准”性的研究工作,转而专注于酶的进化。 1992年,在蒙特雷湾水族馆举办的帕克德学者年会上,我结识了才华横溢、魅力四射的年轻宇宙学家安德鲁·兰格(Andrew Lange)。我们两人都在1989年获得了帕克德奖学金,但不知为何从未谋面。我们几乎是一见钟情。整个1993年,我们都在努力寻找在同一个地方工作的机会。安德鲁每周四会在教完大一物理课后从奥克兰飞往帕萨迪纳,然后赶在周二早上上课前飞回。他想要一个家庭,和我在一起后,他立刻就拥有了一个。我的儿子詹姆斯非常喜欢他。作为实验物理学家的安德鲁,通过亲手拆解在加州理工学院垃圾箱里找到的各种物品,鼓励詹姆斯探索机械世界的自然好奇心。那时候垃圾箱里有很多示波器,我至今还保留着从各种拆解项目中淘来的阴极射线管。1994年,当加州理工学院为安德鲁提供教授职位时,他从伯克利搬了下来。有些物理教授真心认为自己是为加州理工学院招到全国最有前途的年轻宇宙学家的功臣,但这份殊荣应归我所有。不久后,我们喜迎威廉·安德鲁·兰格(William Andrew Lange,1995年)和约瑟夫·因曼·兰格(Joseph Inman Lange,1997年)加入我们的家庭。 我们在建立各自事业的同时,努力抚养三个小男孩。安德鲁为了进行实验和参加团队会议,经常前往南极洲和其他遥远的地方,一去就是好几个星期。他是一位尽职尽责、充满爱心的父亲,但他对科学的热爱也丝毫不减。他渴望在实验部署期间与团队在一起。他1998年的BOOMERANG实验,将气球绕南极洲一圈,收集来自早期宇宙的光子,取得了巨大成功,使他在天体物理学和宇宙学领域名声大噪。他是加州理工学院的宠儿,据说有望获得诺贝尔奖。 我从未如此自豪,也从未如此疲惫。如果没有我们亲爱的“妈妈”卡门(Carmen),我的生活将变得一团糟。卡门向我的孩子们倾注了无尽的爱,为他们的轻微疾病提供家传的疗法,烹饪美味佳肴,并传授实用的洛杉矶公共交通系统导航技巧。在20世纪90年代,我参加了一些当地会议,有时甚至是身怀六甲,但出远门的次数相对较少。虽然我的工作远没有安德鲁那么引人注目,但进展顺利。来自不同学科的杰出科学家纷纷来到加州理工学院,与我及我的学生讨论定向进化问题。在此期间,我将酶的研究推向了全新的方向。该领域正在迅速发展,定向进化方法也得到了广泛采用。我与宝洁公司(Proctor & Gamble)、德固赛公司(Degussa)和陶氏化学公司(Dow Chemical)合作,共同应对工业挑战,这使我能够用“真实”问题(而非模型系统)来展示定向进化的力量。我仍感激这些公司的科学家向我介绍有趣且富有挑战性的问题,并与我分享他们关于酶作用机制的深刻经验。我特别感激的是,他们投入时间和金钱支持一项由年轻女性工程师主导的全新且尚未得到充分验证的技术。值得一提的是,皮姆·斯特默(Pim Stemmer)在1993年我发表论文一年后独立发表了关于定向酶进化的论文,并于1996年在加州理工学院逗留数周。我们计划成立一家新创业公司——马克西根公司(Maxygen),将我们共同的愿景——利用进化创造几乎任何蛋白质或基因——商业化。马克西根公司与加州理工学院就所有定向进化知识产权达成了许可协议,我担任了公司的创始科学顾问。 2000年,我当选美国国家工程院院士,与我父亲当选时的年龄相同,都是四十三岁。在华盛顿特区的就职典礼上,当我走上台时,我父亲站起来,对着台下他众多的朋友大声喊道:“那是我女儿!”我相信,我们仍然是美国国家工程院唯一的一对父女院士。052003-2004年:环球休假 我的大儿子詹姆斯十一岁那年,我的第一任丈夫杰伊因结肠癌去世,享年58岁。安德鲁患有严重的抑郁症,家庭生活愈发紧张。我认为,环球旅行能让我们所有人学到很多知识,也能让我们更加团结;我和四个绅士可以分享冒险经历,就像我年轻时那样,也可以享受安静的时光。值得称道的是,安德鲁同意了这个计划。我选择了两个休假目的地,澳大利亚和南非,在那里我有朋友但没有实际的工作要做。安德鲁选择了卡迪夫,那里有他真正的合作伙伴,也有机会完成一些科学研究。 图5.2003年,小儿子Joseph与澳大利亚朋友 2003年,我们抵达了爱丽丝泉,开始我们的第一次探险之旅,在红土中心与原住民接触。我们的儿子们一到那儿就变得野性十足。在澳洲的第三个晚上,我们入住了一家“五星级”酒店,睡在红色的土地上,四周是设计精良的睡袋,可以有效防止蛇和蜘蛛入侵。在休假的头两周里,我们头顶南十字星,鼻子里满是篝火的气味,头脑里充满了原住民关于流浪生活的传说和故事。我的两个小儿子挖寻蜜蚁和幼虫,和当地的孩子一起玩,加入他们的家庭团体,爬进在沙漠地面上铺开的旧床垫里。我们在墨尔本的斯温伯恩科技学院安顿下来,住了八周,小儿子和哥哥威廉分别在霍桑公立学校上了幼儿园和一年级。我为大儿子詹姆斯在附近的苏格兰学院安排了一个为期两个月的住宿学习。每到周末,我们全家都会去参观金矿和农场。 图 6.2004 年,一家人骑着骆驼穿越西奈沙漠五天图7. William和骆驼我们再次回到加州理工学院短暂停留时,又到了冬季,随后便启程前往非洲,开始我们旅程的下一阶段。这一阶段的旅程包括埃及、南非、纳米比亚和马达加斯加,最后到达英国。这是一次梦幻般的休假,也是我生命中最美好的一年。我们都快乐、健康,也很高兴看到我们的儿子们全身心地投入到冒险之中。 图 8. 2004年,两个小儿子和朋友在纳米比亚图9. 2004年,Joseph与纳米比亚的希姆巴族朋友在一起。 这段时间,我的研究团队表现得异常出色。我意识到他们可以更加独立地工作,并且已经具备了真正的领导能力。从那时起,我尽量给予团队成员更多的自由,让他们能够追求自己的想法并指导其他人。 062005-2010年:黑暗时期 2004年底,我从这段神奇的一年中回来,发现自己患上了乳腺癌,癌细胞已经扩散到淋巴结。我接受了两次手术以及一年半的化疗和放疗,身体日渐衰弱。我开始练习瑜伽,以改善身心健康,并且每天都设法工作,从中找到乐趣和目的。 我们的科学研究开始关注我一直感兴趣的问题——替代能源。石油价格稳步攀升。自2000年以来,我们一直在研究细胞色素P450,使其能够氧化烷烃,其中一个目标就是制造出能够将气态烷烃转化为液态燃料的重组生物体。2005年,在马特·彼得斯(Matt Peters)和彼得·梅因霍尔德(Peter Meinhold)的协助下,在一位著名风险投资家的资助下,我们创建了杰沃公司,这很快成为“合成生物学”领域首批生物燃料初创公司之一。然而,由于我正在接受乳腺癌的密集治疗,身体状况不佳,无法在该项目上投入太多时间,因此马特和彼得负责运营。杰沃公司至今仍在运营,利用工程酵母和化学方法,从生物质开始生产可再生喷气燃料。 2010年1月22日,我的丈夫安德鲁·兰格自杀身亡,这一事件震惊了世界,给他的家人、朋友、学生和同事留下了无尽的悲痛。虽然我们已经分开生活超过两年,但现在我不得不重新拼凑起我们这个家庭的碎片,为三个年龄分别为17岁、13岁和11岁的伤心欲绝的儿子找到出路。那一年对我来说,记忆都是模糊不清的。我的研究团队成员们继续相互扶持,他们和加州理工学院成了我的坚强后盾。我的朋友们也始终陪伴在我身边,给予我帮助。我不断提醒自己,没有人能够确保一生顺利,但我们可以让别人的生活变得更容易。072011年至今:新阶段 2011年之后,我的身体恢复健康,或许比从前更加明智,我下定决心再次冒险,无论是在职业生涯还是个人生活中。我带着儿子们四处旅行,鼓励他们踏上远方的冒险之旅,并在日常圈子之外结识了许多新朋友。我继续从事我钟爱的活动,比如潜水,还有徒步前往圣加布里埃尔山脉的历史性单室小屋。我首次接受邀请,向广大观众发表科学演讲。我发现,无论是科学界还是普通大众,他们都会以热情的态度回应故事讲述和对整体图景的阐述;他们渴望回想起我们所见的万物之奇迹和力量,并相信科学可以引领我们走向更美好的未来。在演讲结尾时,我喜欢描述一个开放且令人兴奋的未来,其中充满了待解答的问题,而不是将问题锁进盒子里。 图10. Frances在她位于洛杉矶以外的圣加布里埃尔山脉的小屋中 或许最重要的是,我感到自由,甚至受到驱使,去用我的科学知识探索新的、更具挑战性的问题。我一直想使酶进行新的化学反应,催化生物界中未知的反应。我向我的团队中的几位优秀化学家提出了一个具体的问题:你能让细胞色素P450使用氮而不是氧来催化反应吗?他们欣然接受挑战,于是我们在2012年成功设计出了首个“氮烯转移酶”和“卡宾转移酶”。基于自然界已准备好接纳各种新能力的这一认识,我们一直在探索一个全新的酶化学世界。 图11. 2016年,William,James,Frances,Joseph在秘鲁亚马逊 如今,我的实验室感觉与上世纪90年代那些激动人心的日子十分相似:氛围紧张,充满强烈的探索感,深知我们正在为未来的分子制造奠定基础,使用包括酶在内的基因编码生物系统,这些酶被改造用于执行人类首次发明的化学反应。我非常感谢能够第二次体验到这种兴奋和专注,再次与一群极具天赋的年轻人共同分享这份喜悦。 图12. 2016年,我和William,James and Joseph在秘鲁品尝玉米酿酒 我在定向酶进化方面所做的研究工作在2011年获得了查尔斯·斯塔克·德雷珀奖,这是美国工程师能获得的最高荣誉。我是首位也是至今唯一一位获得该奖项的女性,该奖项自1989年起由美国国家工程学院颁发。2013年,我在白宫从奥巴马(Barack Obama)总统手中接过了美国国家技术与创新奖章,当时我的两个儿子也随我一同出席。(詹姆斯当时正在阿富汗的美国军队服役,无法与我们一同前往。)2016年,我荣获了千年技术奖,再次成为首位(也是唯一一位)获此殊荣的女性。我并非刻意要成为首位涉足这一领域的女性工程师,但我是首批获得机会展示自己能力的女性之一。作为加州理工学院聘用的第九位女性教师,我是那里的首位女性诺贝尔奖得主。在我的一生中,许多才华横溢的女性加入了科学和工程学的教师队伍,我预测将有越来越多的女性因其科学贡献而获得最高荣誉。08结语我相信读者会注意到,我并没有直接评论与我一起工作并从中汲取灵感的许多学生、博士后和同事们的贡献。有些人在我的诺贝尔演讲中得到了特别提及,但我无法向所有为定向酶进化的构想和广泛应用做出贡献的人表示感谢。现在,我想感谢我的导师和那些我试图指导的人,因为从你们身上我学到了很多东西。我也想感谢本杰明·M·罗森(Benjamin M. Rosen)和唐娜(Donna)为加州理工学院所做和继续做的所有事情;在过去的六年里,我有幸担任唐娜和本杰明生物工程中心的主任,这对我来说是一份莫大的荣幸。 我的父亲于2015年去世,我非常想念他。他要是还在世的话,一定会感到非常自豪,并且会特别喜欢斯德哥尔摩的庆祝活动。我亲爱的次子威廉在2016年以20岁的年纪去世;他的生命虽然短暂,但却因照顾南非的猴子、肯尼亚和印度的孩子以及他的朋友而丰富多彩。两位威廉都永远活在我的心中。我想安德鲁也会为我感到高兴。我的小儿子约瑟夫、我的大儿子詹姆斯和他的妻子阿兰娜(Alanna),以及我的继子肖恩·贝利(Sean Bailey),与近六十位朋友、家人和前学生一同来到斯德哥尔摩,共同庆祝我获奖。我非常感谢我所拥有的一切,以及所有丰富了我生活的人和动物。 原文资料:https://www.nobelprize.org/prizes/chemistry/2018/arnold/biographical/识别微信二维码,添加生物制品圈小编,符合条件者即可加入生物制品微信群!请注明:姓名+研究方向!版权声明本公众号所有转载文章系出于传递更多信息之目的,且明确注明来源和作者,不希望被转载的媒体或个人可与我们联系(cbplib@163.com),我们将立即进行删除处理。所有文章仅代表作者观点,不代表本站立场。
高管变更疫苗
2023-12-14
OWINGS MILLS, Md., Dec. 14, 2023 /PRNewswire/ -- Prominently featured in The Inner Circle, Wale Charles Abolarin is acknowledged as a Distinguished Healthcare Professional for his contributions to the field of Clinical Informatics Technology.
Dr. Abolarin received his Doctorate of Medicine specializing in Anesthesiology from the Ladoke Akintola University of Technology in 2009. He furthered his education in the United States at the University of South Florida, obtaining a graduate certificate in Health Informatics in 2016 and a Master's degree in Health informatics in 2017. In addition, Dr. Abolarin boasts an impressive array of prestigious certifications in Leadership and Health Information Technology, among them the notable Physician IT Architect Certificate.
Touting more than 14 years in the Healthcare, Dr. Abolarin stands at the forefront as the CEO and Chief Medical Informatics Officer of Helix Healthcare Inc. This esteemed institution is not just a provider but a beacon of hope for those with developmental disabilities in Maryland and beyond. Championing the cause of local communities, Dr. Abolarin passionately avers that the mission of Helix Healthcare goes beyond medical care. It's about sculpting an ecosystem where patients and their families can effortlessly avail themselves of equitable healthcare, find promising employment opportunities, access top-notch job training, community development, and harness the power of education through technology. Helix Healthcare is a lifeline, providing indispensable services like Alternative living units and remote support services.
Before stepping into his current role, Dr. Abolarin accumulated an expansive range of experiences across various capacities in the medical field. He has held esteemed roles such as Physician Champion, Physician Executive, Physician Advisor, and Physician Informatics Architect. His association with significant institutions includes the McLaren Health Care Corporation, Atos Digital Health Solutions, Midland Memorial Hospital, Texas Scottish Rite Hospital for Children, Our Lady of Lourdes's Memorial Hospital, MedStar Good Samaritan Hospital, and a number of hospitals in Nigeria. Beyond these roles, Dr. Abolarin has provided consultation services to several US hospitals, pioneering multiple informatics projects. These projects, powered by technology, have been meticulously designed to mitigate physician burnout and amplify productivity. In his relentless pursuit of excellence, he is a member of the American College of Healthcare Executives, the American Society of Anesthesiology, and the Nigerian Medical Association.
With an unwavering and formidable passion for serving others, Dr. Abolarin has not only achieved immense success but has also set himself apart in the realm of informatics. One of his crowning achievements is his role as the architect behind the sepsis advisor at McLaren Health Care Corporation, an algorithmic powerhouse designed to swiftly diagnose sepsis, thus acting as a bulwark against potential fatalities. As we gaze into the horizon, let it be known that Dr. Abolarin's legacy as a leader isn't just rooted in his unmatched expertise in healthcare or informatics alone. It's his unparalleled versatility and prowess across diverse fields, from healthcare to entrepreneurship, that truly sets him apart from the crowd.
Contact:
Katherine Green
516-825-5634
[email protected]
SOURCE The Inner Circle
高管变更
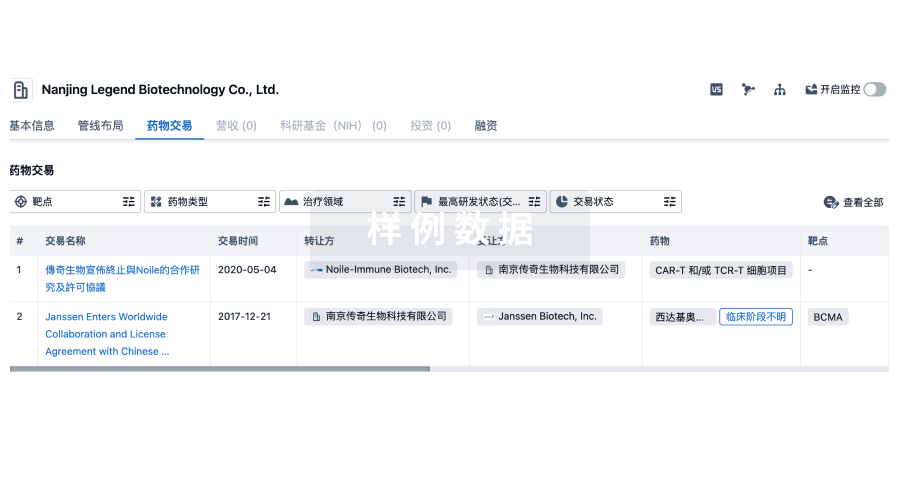
100 项与 Texas Scottish Rite Hospital for Children 相关的药物交易
登录后查看更多信息
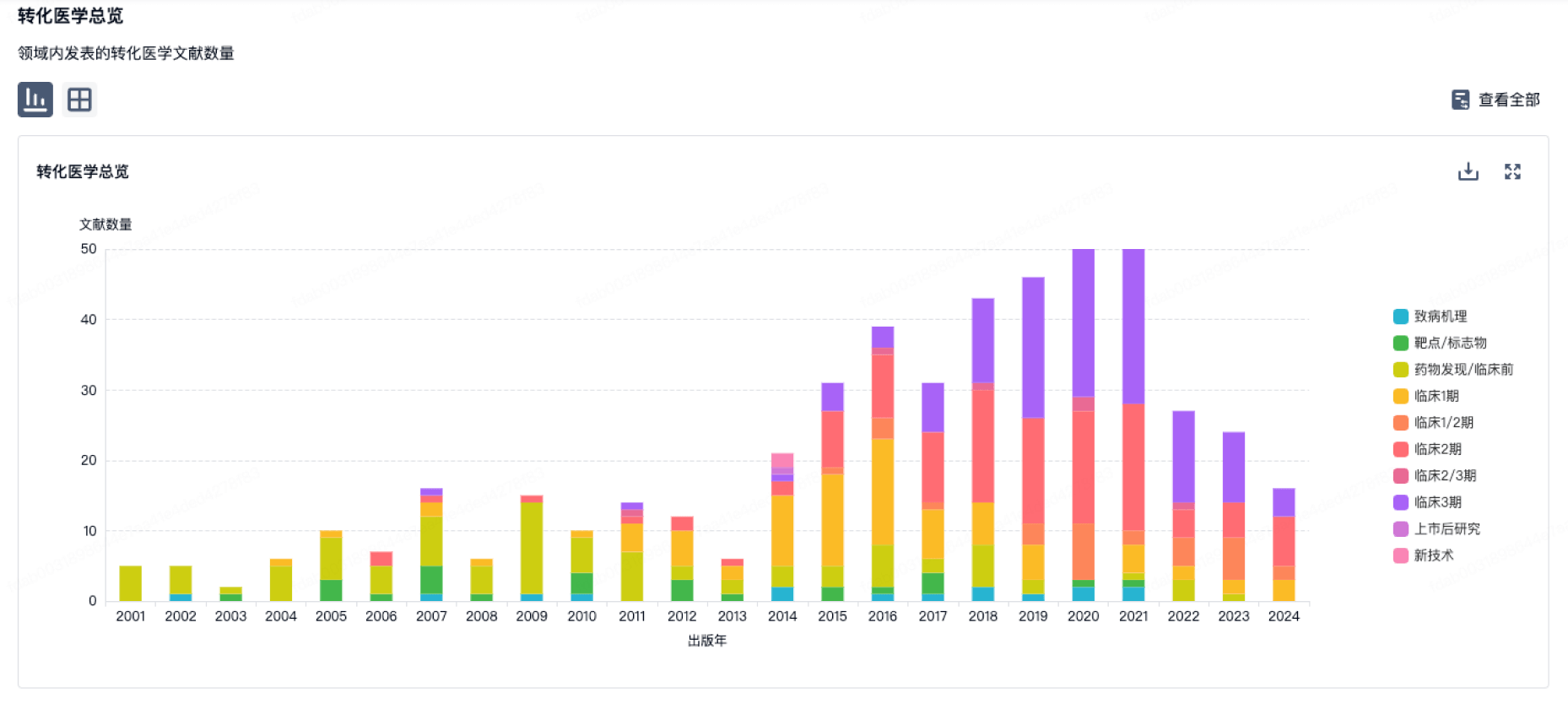
100 项与 Texas Scottish Rite Hospital for Children 相关的转化医学
登录后查看更多信息
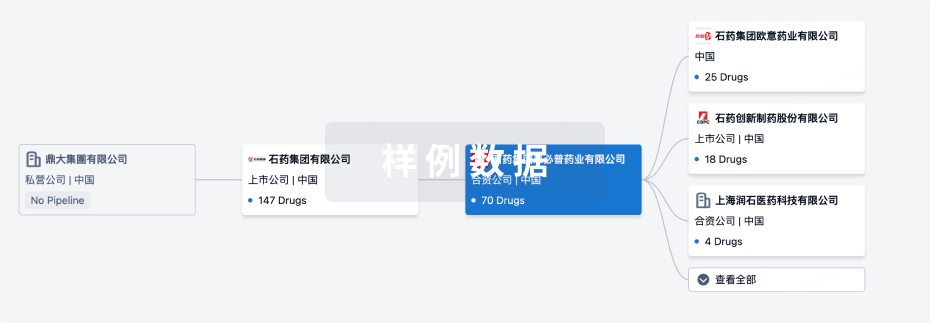
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年07月14日管线快照
无数据报导
登录后保持更新
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
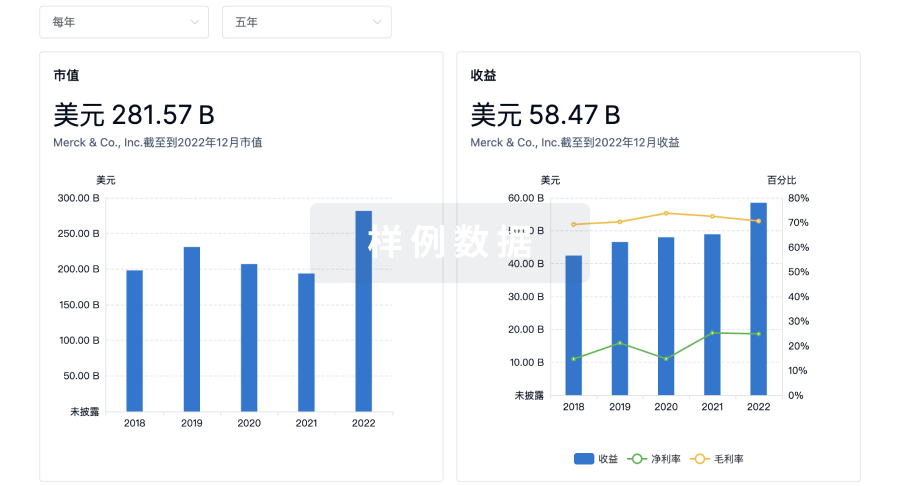
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用