更新于:2024-11-04

Achilles Therapeutics plc
更新于:2024-11-04
概览
关联
6
项与 Achilles Therapeutics plc 相关的临床试验An Open-Label, Multi-Centre Phase II Study Evaluating the Long-Term Safety and Clinical Activity of Neoantigen Reactive T Cells in Patients Who Have Previously Received ATL001 in a Clinical Trial
This is an Open-Label, Multi-Centre Phase II study to evaluate the long-term safety and clinical activity of ATL001, previously administered intravenously to patients in Study ATX-NS-001 (NCT04032847) or Study ATX-ME-001 (NCT03997474).
开始日期2022-06-01 |
申办/合作机构 |
An Open-Label, Multi-Centre Phase I/IIa Study Evaluating the Safety and Clinical Activity of Neoantigen Reactive T cells in Patients with Advanced Non-Small Cell Lung Cancer - CHIRON
开始日期2022-01-31 |
申办/合作机构 |
An Open-Label, Multi-Centre Phase I/IIa Study Evaluating the Safety and Clinical Activity of Neoantigen Reactive T Cells in Patients With Metastatic or Recurrent Melanoma
This is a first-in-human, open-label, multi-centre, phase I/IIa study to characterize the safety and clinical activity of ATL001, autologous clonal neoantigen reactive T cells (cNeT) administered intravenously in adults with metastatic or recurrent melanoma.
开始日期2019-08-15 |
申办/合作机构 |
100 项与 Achilles Therapeutics plc 相关的临床结果
登录后查看更多信息
0 项与 Achilles Therapeutics plc 相关的专利(医药)
登录后查看更多信息
7
项与 Achilles Therapeutics plc 相关的文献(医药)2019-10-01·Immuno-oncology technology
Adoptive cell therapy with tumour-infiltrating lymphocytes: the emerging importance of clonal neoantigen targets for next-generation products in non-small cell lung cancer
Review
作者: Salm, Max ; Dangl, Markus ; Robertson, Jane
Immune checkpoint blockade has significantly improved clinical outcomes for patients with non-small cell lung cancer (NSCLC) and other solid tumours, but many patients do not respond and acquired resistance is common. Aspects of the tumour microenvironment linked to clinical outcomes include the proportion of tumour-infiltrating lymphocytes (TIL), tumour programmed death ligand 1 ( PD-L1) score and tumour mutation burden. Adoptive cell therapy (ACT), a technique that works by infusing ex vivo expanded T lymphocytes to increase the effector cell pool in tumours, is anticipated to become a viable therapeutic option for patients with solid tumours, akin to chimeric antigen receptor T cell (CAR-T) therapy in haematological malignancies. TIL therapy has shown durable clinical responses in heavily pre-treated patients with melanoma and other solid tumours. We review the experience of ACT with TILs and the recent evidence that clonal neoantigens might be the most relevant immunotherapeutic targets in heterogeneous solid tumours such as NSCLC. Clonal (or truncal) neoantigens arise from the earliest mutagenic events in tumour evolution, and are retained over time in all tumour cells within a patient, making them the ideal target for T cell therapy. NSCLC has one of the highest clonal mutation burdens of all cancers through exposure to carcinogens in tobacco smoke, providing a strong rationale to develop clonal neoantigen reactive T cells (cNeT) for this indication. The first treatment modality to test this concept clinically is ATL001, a cNeT product that is derived from autologous TILs and enriched for T cells specifically recognizing clonal neoantigenic epitopes by selective expansion. Clinical studies of ATL001 will commence in 2019.
Nature communications1区 · 综合性期刊
GATA3 induces mitochondrial biogenesis in primary human CD4+ T cells during DNA damage
1区 · 综合性期刊
ArticleOA
作者: Lavender, Paul ; Callender, Lauren A ; Hendy, Eleanor ; Akbar, Arne N ; Romano, Lisa E L ; Kelly, Audrey ; Garrod-Ketchley, Conor ; Chapple, J Paul ; Henson, Sian M ; Schroth, Johannes ; Carroll, Elizabeth C
Abstract:
GATA3 is as a lineage-specific transcription factor that drives the differentiation of CD4+ T helper 2 (Th2) cells, but is also involved in a variety of processes such as immune regulation, proliferation and maintenance in other T cell and non-T cell lineages. Here we show a mechanism utilised by CD4+ T cells to increase mitochondrial mass in response to DNA damage through the actions of GATA3 and AMPK. Activated AMPK increases expression of PPARG coactivator 1 alpha (PPARGC1A or PGC1α protein) at the level of transcription and GATA3 at the level of translation, while DNA damage enhances expression of nuclear factor erythroid 2-related factor 2 (NFE2L2 or NRF2). PGC1α, GATA3 and NRF2 complex together with the ATR to promote mitochondrial biogenesis. These findings extend the pleotropic interactions of GATA3 and highlight the potential for GATA3-targeted cell manipulation for intervention in CD4+ T cell viability and function after DNA damage.
Nature Cancer
Breaking the performance ceiling for neoantigen immunogenicity prediction
作者: Szukszto, Maciej ; Morton, Laura ; Salm, Max ; O'Brien, Hugh ; Boulton, Charlotte ; Reker Hadrup, Sine ; Swanton, Charles ; Quezada, Sergio A. ; Samuels, Yardena ; Mansour, Marc R. ; Becker, Pablo D. ; O'Farrell, Felix
Neoantigen immunogenicity prediction is a burgeoning field with vast potential; however, the shortage of high-quality data and biases in current datasets limit model generalizability.Here we discuss some of the pitfalls that may underly this limited performance and propose a path forward.The unbiased immunogenicity datasets are beginning to emerge in increasing volumes, addnl. steps are likely to be required to achieve robust neoantigen prediction.In vitro-stimulated T cells from healthy donors provide an abundant, controlled source of functional T cells, avoiding the patient-specific confounders seen in cancer patient.
71
项与 Achilles Therapeutics plc 相关的新闻(医药)2024-09-26
DUBLIN--(
BUSINESS WIRE
)--The
"Cancer Immunotherapy Markets. The Race for the Cures. Market Forecasts for Immuno-Oncology Therapeutics by Therapy, by Cancer and by Customer including Executive and Consultant Guides. 2023 to 2027"
report has been added to
ResearchAndMarkets.com's
offering.
A revolution in cancer therapy is underway. New therapy based on using the body's natural immune defenses is having unprecedented success.
CAR-T Cells? Checkpoint Inhibitors? Cytokines? Find out about the technology in readily understood terms that explain the jargon. Already worth billions the global market is poised for dramatic growth. The impact on the health care industry is enormous. The report forecasts the market size out to 2027.
Find the opportunities and the pitfalls. Understand growth expectations and the ultimate potential market size. Make investment decisions and valuations with confidence using the latest data.
This report explores the opportunity in this market and what companies are poised to benefit.
Key Topics Covered:
1 Market Guides
1.1 Situation Analysis
1.2 Guide for Executives and Marketing Staff
1.3 Guide for Investment Analysts and Management Consultants
2 Introduction and Market Definition
2.1 What is Cancer Immunotherapy?
2.2 Immunotherapy - the looming cures
2.3 Market Definition
2.4 Methodology
2.5 U.S. Medical Market and Pharmaceutical Spending - Perspective
2.5.1 Global Expenditures for Medicines
3 Immunotherapy - Guide to Immune Technologies
3.1 The Immune System
3.1.1 Innate immune system
3.1.2 Adaptive immune system
3.1.3 Tumor immunology - the immune surveillance system
3.2 Immuno Oncology Technologies
3.2.1 Monoclonal Antibodies
3.2.2 Cancer vaccines
3.2.3 Cytokines
3.2.4 Cell Based Therapies
3.2.5 Inhibitors/Agonists
3.2.6 Antibody Drug Conjugates
3.2.7 Others
4 Industry Overview
4.1 Market Players - Roles & Impacts
4.1.1 Drug manufacturers - Larger/pharmaceutical
4.1.2 Drug manufacturers - Generic
4.1.3 Contract Research and Manufacturing
4.1.4 In Vitro Diagnostics Industry
4.1.5 Drug Marketing Companies
4.1.6 Biotechnology Companies
4.1.7 Regulatory Bodies
5 Market Trends
5.1 Factors Driving Growth
5.1.1 Outcome potential
5.1.2 Fast tracking
5.1.3 Funding
5.1.4 Technology Environment
5.1.5 Target Solutions
5.2 Factors Limiting Growth
5.2.1 Cost of Treatment
5.2.2 Clinical Trials Role
5.2.3 Combinations
5.2.4 Protocols
5.3 Therapeutic Technology Development
5.3.1 Combinations - Issues and Complexity
5.3.2 Preference for a drug
5.3.3 Problems of Immunity Engineering
5.3.4 The Role of Cost
5.3.5 The Disruption Dynamic
5.3.6 CAR-T Cell Therapy
5.3.7 The Next Five Years
6 Cancer Immunotherapy Recent Developments
6.1 Recent Developments - Importance and How to Use This Section
6.2 Continued Success with Immunotherapy in Melanoma
6.3 AC Immune Receives FDA Fast Track Designation
6.4 LTZ Announces Financing
6.5 Immunotherapy for Cancer Overview
6.6 Implantable device shrinks pancreatic tumors
6.7 mRNA Vaccine And Immunotherapy Reduce Melanoma Recurrence
6.8 Towards a Universal Cancer Immunotherapy
6.9 New Strategy May Improve T-Cell Therapy in Solid Tumors
6.10 Immunotherapy linked to increase in Medicare spending
6.11 Immunotherapy Effective with Ovarian Cancer
6.12 Cancer Immunotherapy Granted Fast Track
7 Profiles of Key Immunotherapy Companies
AbbVie
Achilles Therapeutics
Acumen Pharmaceuticals
Adagene
Adaptimmune Therapeutics
Adicet Bio
ALX Oncology Holdings
Ambrx Biopharma
Amgen
Apexigen
Arcus Biosciences
argenx
AstraZeneca
Atreca
Avalo Therapeutics
Avid Bioservices
Bavarian Nordic
BioAtla
Biogen Inc.
BioNTech
Bolt Biotherapeutics
Bristol-Myers Squibb
Candel Therapeutics
Caribou Biosciences
Celldex Therapeutics
Checkpoint Therapeutics
Chinook Therapeutics
Corvus Pharmaceuticals
Cullinan Oncology
Eli Lilly
EOM Pharmaceuticals
Evaxion Biotech
Genenta Science
Gilead Sciences
Gracell Biotechnologies
Greenwich LifeSciences
Gritstone bio
Harpoon Therapeutics
ImmunityBio
Immunocore Holdings
Immunome
IMV Inc
Incyte
Indaptus Therapeutics
Instil Bio
Iovance Biotherapeutics
Johnson & Johnson
Marker Therapeutics
Medicenna Therapeutics
Merck & Co.
Merus
Moderna
Mustang Bio
Nanobiotix
Neoleukin Therapeutics
Novartis
Novavax
Oncorus
PDS Biotechnology
Pfizer
Regeneron Pharmaceuticals
Roche
Sanofi
Sensei Biotherapeutics
Senti Biosciences
Surface Oncology
Takeda Pharmaceutical
TC Biopharm
ThermoGenesis Holdings
UroGen Pharma
Werewolf Therapeutics
Xilio Therapeutics
Zymeworks
8 The Global Market for Immuno-Oncology Therapeutics
8.1 Global Market Overview by Country
8.2 Global Market by Therapy
8.3 Global Market by Cancer
8.4 Global Market by Customer
9 Global Immuno-Oncology Therapy Markets - By Therapy
9.1 MAB
9.2 Cytokine
9.3 Vaccine
9.4 Cell Based
9.5 Inhibitor/Agonist
9.6 Other IO Therapy
10 Global Immuno-Oncology Therapeutic Markets - By Cancer
10.1 Breast
10.2 ColoRectal
10.3 Cervical
10.4 Lung
10.5 Precancer
10.6 Prostate
10.7 Melanoma
10.8 Blood
10.9 Other Cancer
11 Global Immuno-Oncology Therapeutic Markets - By Customer
11.1 Pharma
11.2 Clinic
11.3 Other Customer
For more information about this report visit
https://www.researchandmarkets.com/r/8355qg
About ResearchAndMarkets.com
ResearchAndMarkets.com is the world's leading source for international market research reports and market data. We provide you with the latest data on international and regional markets, key industries, the top companies, new products and the latest trends.
免疫疗法快速通道ASCO会议
2024-09-19
Achilles Therapeutics has engaged BofA Securities to explore and review “value-maximizing strategies.”
Achilles Therapeutics has torn up its strategy. The British biotech is stopping work on its clinical-phase cell therapy, looking into deals with groups working on other modalities and preparing to lay off staff.London-based Achilles sounded committed to its tumor-infiltrating lymphocyte (TIL)-based therapy when it published updated phase 1/2 data one month ago. While there were no new objective responses, the biotech said the results showed the potential of its platform and identified the release of updated data with enhanced host conditioning as a milestone for the second half of 2024.Weeks later, Achilles has decided to stop development of its TIL-based therapy and close two phase 1/2a trials. CEO Iraj Ali, Ph.D., said the “studies in lung cancer and melanoma have not met our goals for commercial viability.”The biotech is planning to lay off people in conjunction with the R&D rethink. Achilles ended last year with 204 full-time employees plus 11 part-time staffers. A workforce reduction and other cost-cutting measures are in the works, but the details are still taking shape as part of an employee consultation process that Achilles is conducting in line with U.K. legislation. The future of the biotech is similarly uncertain. Achilles said it will “refocus its strategy to explore further engagement with third parties who are developing alternative modalities to target clonal neoantigens for the treatment of cancers, such as neoantigen vaccines, ADCs and TCR-T therapies.” The biotech has also engaged BofA Securities to explore and review “value-maximizing strategies.”Closing the two phase 1/2a trials eliminates Achilles’ clinical-phase pipeline, but the company still has assets that could be of interest to other drug developers. Arcturus Therapeutics entered into a research pact with Achilles in May. The mRNA specialist is developing vaccines that target clonal neoantigens, protein markers that Achilles can identify using its PELEUS bioinformatics platform.The biotech also has a Nasdaq listing and, as of the end of June, $95.1 million, assets that could support a reverse merger with a company that wants to list its shares and strengthen its bank balance without taking the IPO route. Achilles said a range of options, including a reverse merger, are on the table.

疫苗细胞疗法免疫疗法
2024-09-19
Plus, news about GSK, Novo Nordisk, Tanai Therapeutics, Nomic Bio, Brenus Pharma, Xspray, Achilles Therapeutics, BioXcel Therapeutics and Nuvalent:
Ascendis’ $300M offering:
The Danish company
announced
the proposed share sale a few days after
disclosing
pivotal trial data for its dwarfism drug.
— Kyle LaHucik
Basilea secures anti-infectives deal with BARDA:
The Swiss drugmaker will get $29 million in initial funding from the federal agency to advance development of two antifungal drugs, fosmanogepix and BAL2062. Basilea is eligible for up to $268 million in support under the terms of the multi-year
agreement
.
— Ayisha Sharma
GSK chips in with cash for antibiotic resistance organization:
The $66 million in new
funds
will help the Global Antibiotic Research and Development Partnership speed up research into treatments for antibiotic-resistant infections. The UK drugmaker contributed €4.5 million, while the European Commission pledged €20 million.
— Ayisha Sharma
Novo Nordisk backs Belgian obesity startup:
The Wegovy maker and BioGeneration Ventures
are among
the investors in Tanai Therapeutics’ €6 million seed round.
— Kyle LaHucik
Nomic Bio’s $42M Series B:
The “protein profiling company”
raised
the money from Amplitude Ventures, AVANT BIO, Lux Capital, Real Ventures, and SR One.
— Kyle LaHucik
Brenus Pharma’s $25M round:
Angelor, Noshaq and Investsud, among others, invested in the French startup’s
Series A
to support development of its cancer vaccine.
— Kyle LaHucik
Xspray Pharma to refile cancer drug with the FDA
: The Stockholm-based biotech plans to
resubmit
Dasynoc for the second time in the fourth quarter, with an eye to a potential launch early next year. Xspray’s original NDA was hit with a CRL last year, and the FDA had requested more information related to dosing and a third-party manufacturer.
— Ayisha Sharma
Achilles Therapeutics undergoes strategic review:
The company
is stopping work
on its TIL-based cNeT program. It is also planning a workforce reduction and other cost-cutting as it explores “new opportunities” for its assets. Its stock
$ACHL
was up about 30% on Thursday morning.
— Jaimy Lee
BioXcel Therapeutics
is “
deprioritizing
sales efforts” for Igalmi, its agitation treatment. —
Jaimy Lee
Nuvalent
ended up
raising
a total of $575 million in its offering.
— Jaimy Lee
疫苗
100 项与 Achilles Therapeutics plc 相关的药物交易
登录后查看更多信息
100 项与 Achilles Therapeutics plc 相关的转化医学
登录后查看更多信息
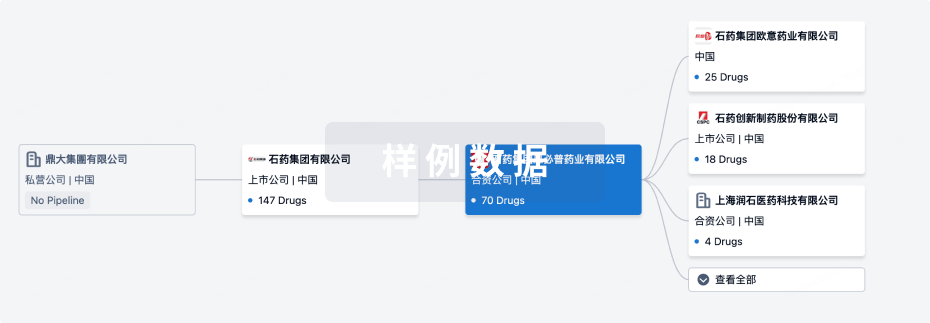
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2024年12月30日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
其他
1
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
克隆性新抗原反应性T细胞(Achilles Therapeutics) | 局部晚期非小细胞肺癌 更多 | 终止 |
登录后查看更多信息
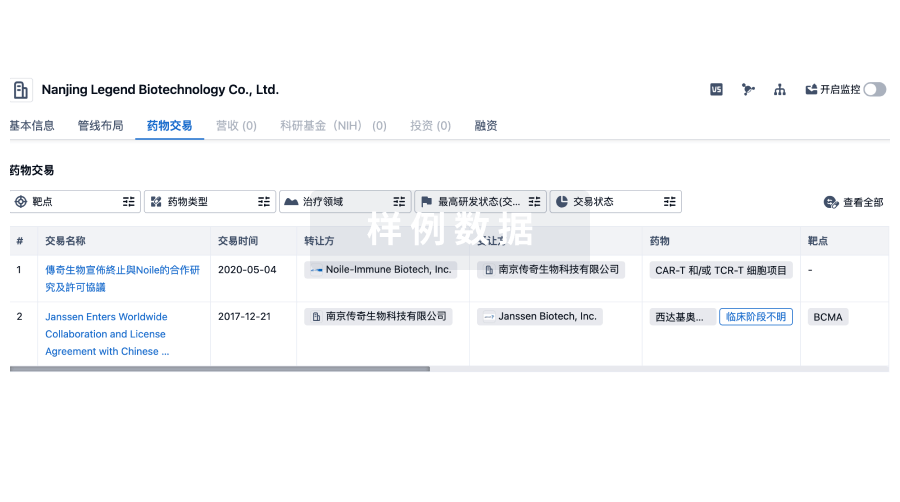
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
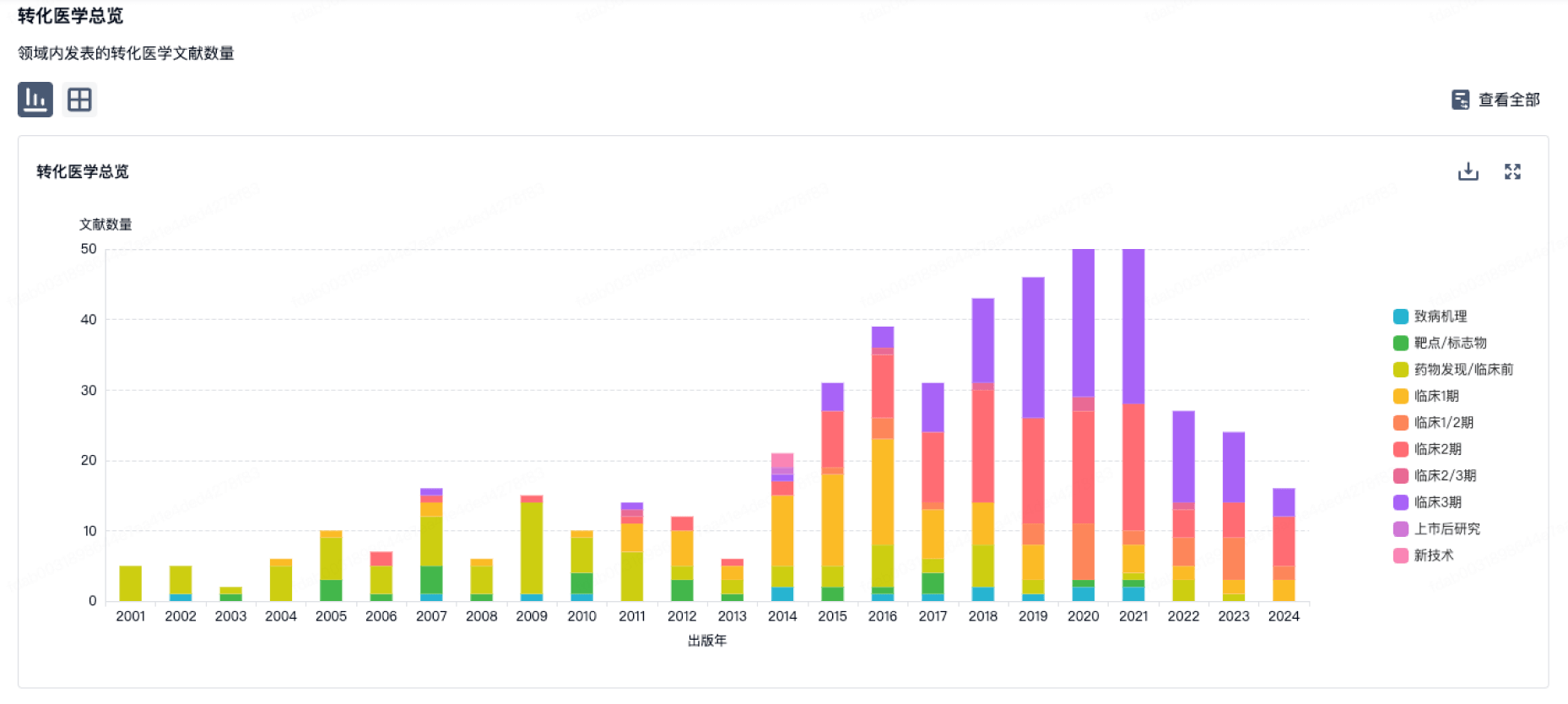
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
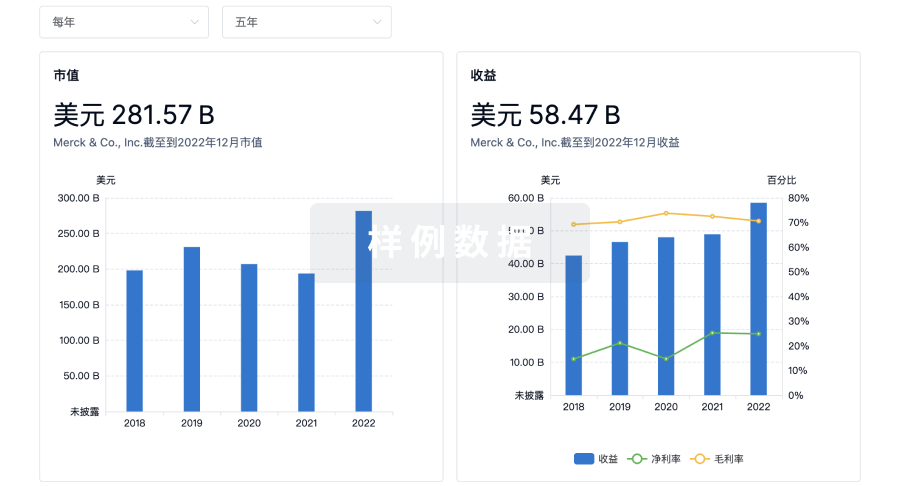
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
标准版
¥16800
元/账号/年
新药情报库 | 省钱又好用!
立即使用
来和芽仔聊天吧
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
