预约演示
更新于:2025-01-23

Papua New Guinea Institute of Medical Research
更新于:2025-01-23
概览
标签
其他疾病
小分子化药
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 排名前五的药物类型 | 数量 |
|---|---|
| 小分子化药 | 1 |
| 排名前五的靶点 | 数量 |
|---|---|
| MIF(巨噬细胞移动抑制因子) | 1 |
关联
1
项与 Papua New Guinea Institute of Medical Research 相关的药物靶点 |
作用机制 MIF抑制剂 |
在研机构 |
在研适应症 |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期- |
26
项与 Papua New Guinea Institute of Medical Research 相关的临床试验NCT06148792
A Revised Tafenoquine Dose to Improve Radical Cure for Vivax Malaria - TAfenoquine DOsing REvised
The goal of this clinical trial is to assess the efficacy and safety or a revised weight band tafenoquine dose in vivax malaria patients. The main question[s] it aims to answer are:
* is a revised weight-based TQ regimen (TQRevised: target dose 7.5mg/kg) non-inferior to high dose primaquine (7mg/kg over 7 days)
* is a revised weight-based TQ regimen (TQRevised: target dose 7.5mg/kg) superior to fixed dose tafenoquine (300mg)
* is the tolerability and safety of TQRevised acceptable
* is TQRevised acceptable and feasible Participants will receive a tafenoquine target dose 7.5mg/kg in weight bands. Researchers will compare this to patients receiving a fixed dose tafenoquine and high dose primaquine to see if safe and effective.
* is a revised weight-based TQ regimen (TQRevised: target dose 7.5mg/kg) non-inferior to high dose primaquine (7mg/kg over 7 days)
* is a revised weight-based TQ regimen (TQRevised: target dose 7.5mg/kg) superior to fixed dose tafenoquine (300mg)
* is the tolerability and safety of TQRevised acceptable
* is TQRevised acceptable and feasible Participants will receive a tafenoquine target dose 7.5mg/kg in weight bands. Researchers will compare this to patients receiving a fixed dose tafenoquine and high dose primaquine to see if safe and effective.
开始日期2024-05-10 |
申办/合作机构 |
NCT05874271
Feasibility of High Daily Dose Short Course Primaquine After G6PD Testing for the Radical Cure of Plasmodium Vivax Malaria
Significant gains have been made in reducing the overall burden of malaria worldwide, however these have been far greater for Plasmodium falciparum than P. vivax.
P. vivax remains a major obstacle to malaria control and elimination efforts, largely due to its ability to form dormant liver stages (hypnozoites) that allows it to escape detection and treatment. Importantly, they are susceptible only to 8 aminoquinolines such as primaquine. However, primaquine is associated with risk of haemolysis in individuals with a genetic condition, called glucose-6-phosphate dehydrogenase (G6PD) deficiency. Additionally, the recommended 14-day prolonged treatment regimen is associated with poor treatment adherence, hence ineffective primaquine treatment. Innovative solutions to the radical cure of both the blood and liver stages of P. vivax are urgently required.
The PNG National Department of Health has requested a pragmatic study of the feasibility and cost-effectiveness of implementing point-of-care G6PD testing followed by high-dose, short-course primaquine treatment regimens for patients with P. vivax malaria. This revised case management is to be combined with practicable enhancements to patient education, supervision, malariometric surveillance and pharmacovigilance.
This will be a before-after longitudinal health facility-based study implemented at Napapar and Mugil health centres and Baro and Wirui clinics. A staged approach for the implementation of the revised case management strategy will be used, including patient education and counselling, community-based clinical review, with mixed methods evaluation.
P. vivax remains a major obstacle to malaria control and elimination efforts, largely due to its ability to form dormant liver stages (hypnozoites) that allows it to escape detection and treatment. Importantly, they are susceptible only to 8 aminoquinolines such as primaquine. However, primaquine is associated with risk of haemolysis in individuals with a genetic condition, called glucose-6-phosphate dehydrogenase (G6PD) deficiency. Additionally, the recommended 14-day prolonged treatment regimen is associated with poor treatment adherence, hence ineffective primaquine treatment. Innovative solutions to the radical cure of both the blood and liver stages of P. vivax are urgently required.
The PNG National Department of Health has requested a pragmatic study of the feasibility and cost-effectiveness of implementing point-of-care G6PD testing followed by high-dose, short-course primaquine treatment regimens for patients with P. vivax malaria. This revised case management is to be combined with practicable enhancements to patient education, supervision, malariometric surveillance and pharmacovigilance.
This will be a before-after longitudinal health facility-based study implemented at Napapar and Mugil health centres and Baro and Wirui clinics. A staged approach for the implementation of the revised case management strategy will be used, including patient education and counselling, community-based clinical review, with mixed methods evaluation.
开始日期2023-07-10 |
NCT05426434
Intermittent Preventive Treatment in Pregnancy With Sulfadoxine-pyrimethamine Plus Dihydroartemisinin-piperaquine to Prevent Malaria Infection and Reduce Adverse Pregnancy Outcomes in Papua New Guinea - a Randomised Controlled Trial
This trial tests the hypothesis that intermittent preventive treatment in pregnancy (IPTp) with sulfadoxine-pyrimethamine (SP) plus dihydroartemisinin-piperaquine (DP) significantly reduces the risk of malaria infection (primary outcome) and adverse birth outcomes (key secondary outcome) in an endemic area of Papua New Guinea (PNG), compared to IPTp with SP alone (the current standard of care).
To test this hypothesis a double-blinded, placebo-controlled, phase-III, superiority trial will individually randomize 1,172 HIV-uninfected pregnant women enrolled from 12-26 gestational weeks in equal proportions to one of two IPTp arms: 1) SP given every for weeks, or 2) SP+DP given every 4 weeks. DP placebos will be used to ensure adequate blinding is achieved in the study and follow-up will end 28 days after giving birth.
To test this hypothesis a double-blinded, placebo-controlled, phase-III, superiority trial will individually randomize 1,172 HIV-uninfected pregnant women enrolled from 12-26 gestational weeks in equal proportions to one of two IPTp arms: 1) SP given every for weeks, or 2) SP+DP given every 4 weeks. DP placebos will be used to ensure adequate blinding is achieved in the study and follow-up will end 28 days after giving birth.
开始日期2022-08-31 |
申办/合作机构 |
100 项与 Papua New Guinea Institute of Medical Research 相关的临床结果
登录后查看更多信息
0 项与 Papua New Guinea Institute of Medical Research 相关的专利(医药)
登录后查看更多信息
1,246
项与 Papua New Guinea Institute of Medical Research 相关的文献(医药)2025-03-01·Diagnostic Microbiology and Infectious Disease
Establishing quality assurance for COVID-19 antigen tests in the Indo Pacific Region: A multi-site implementation study
Article
作者: Khamphaphongphane, Bouaphanh ; Markby, Jessica ; Norchaleun, Boualay ; Ridley, Kirsten ; Phoeung, Chan Leakhena ; Toliman, Pamela J ; Ninan, Marilyn ; Williamson, Deborah A ; Prestedge, Jacqueline ; Seang, Kennarey ; Saphonn, Vonthanak ; Cunningham, Philip ; Cabuang, Liza ; Young, Garrett ; Vallely, Andrew
2025-01-01·Social Science & Medicine
Tuberculosis treatment and undernutrition on Daru Island, Papua New Guinea: A qualitative exploration of a local foodscape
Article
作者: Kupul, M ; Jops, P ; Nindil, H ; Majumdar, S S ; Persson, A ; Kelly-Hanku, A ; Marks, G ; Bell, S ; Graham, S M ; Pomat, W ; Islam, S ; Bauri, M ; Nake Trumb, R ; Cowan, J
2024-12-31·Global Public Health
The effects of COVID-19 on maternal, newborn and child health services in Papua New Guinea
Article
作者: Kerry, Zebedee ; Kelly-Hanku, Angela ; Maalsen, Anna ; Trumb, Richard Nake ; Farquhar, Rachael ; Wratten, Melanie ; Newland, Jamee ; Boli-Neo, Ruthy ; Vallely, Lisa M. ; Homer, Caroline SE ; Seymour, Mikaela ; Aeno, Herick ; Mek, Agnes Kupul ; Neuendorf, Nalisa
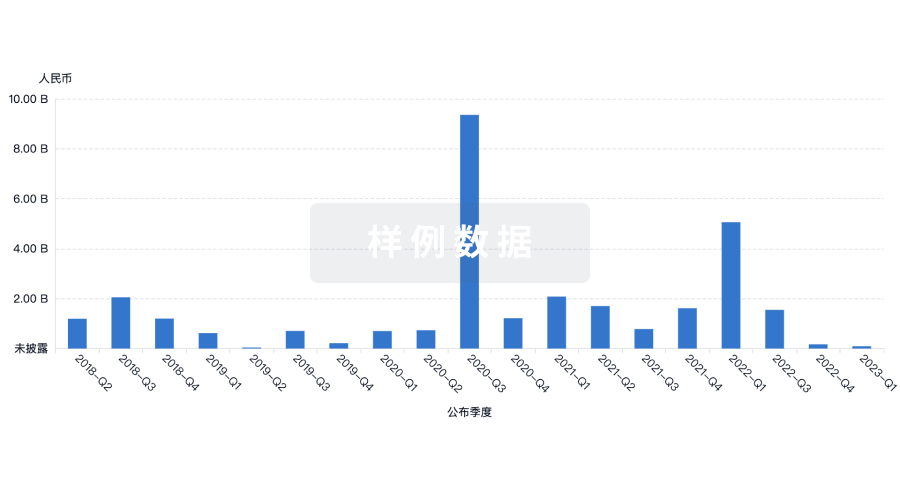
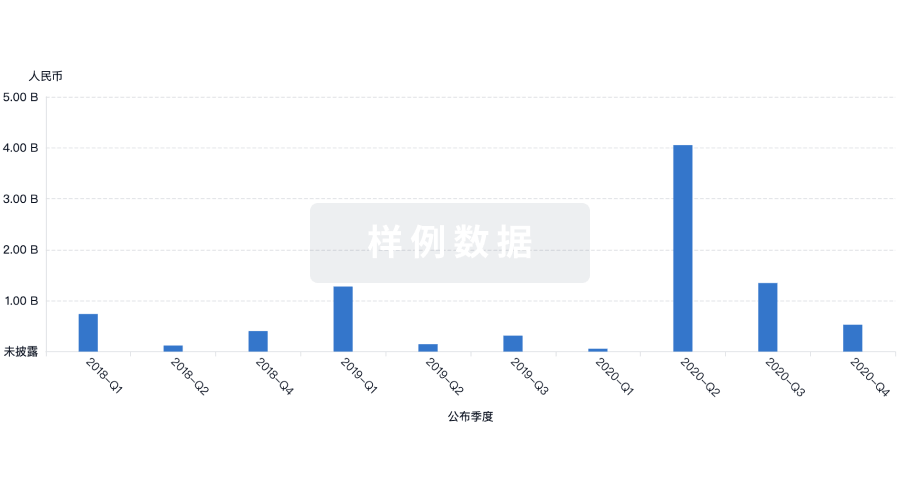
100 项与 Papua New Guinea Institute of Medical Research 相关的药物交易
登录后查看更多信息
100 项与 Papua New Guinea Institute of Medical Research 相关的转化医学
登录后查看更多信息
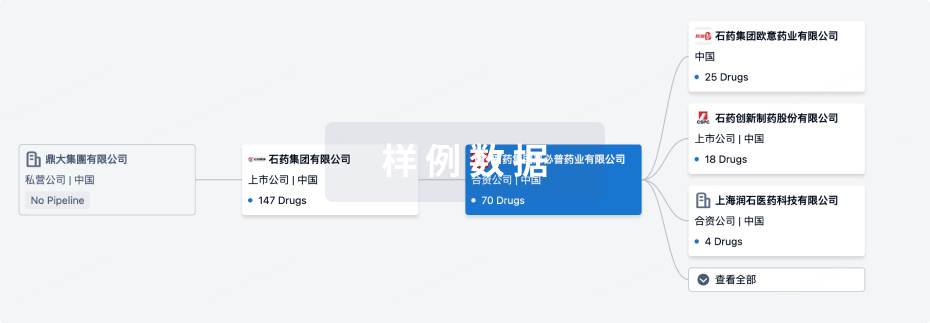
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年04月15日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
临床前
1
登录后查看更多信息
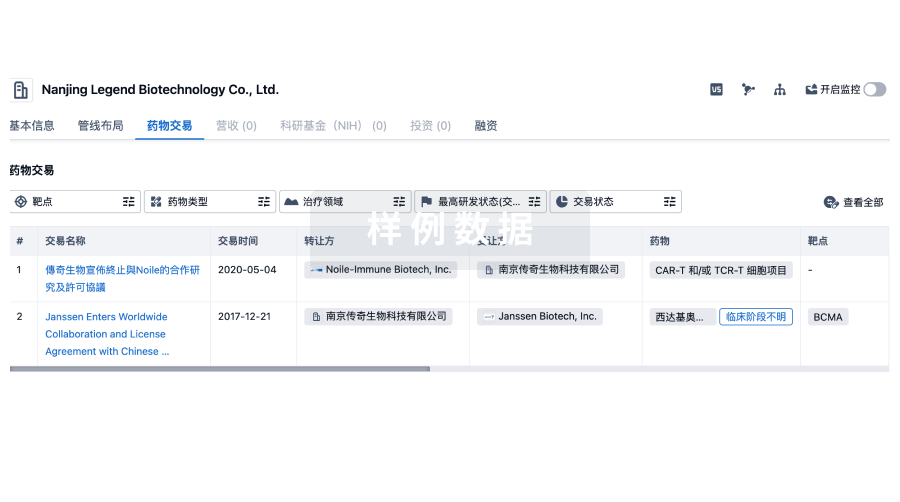
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
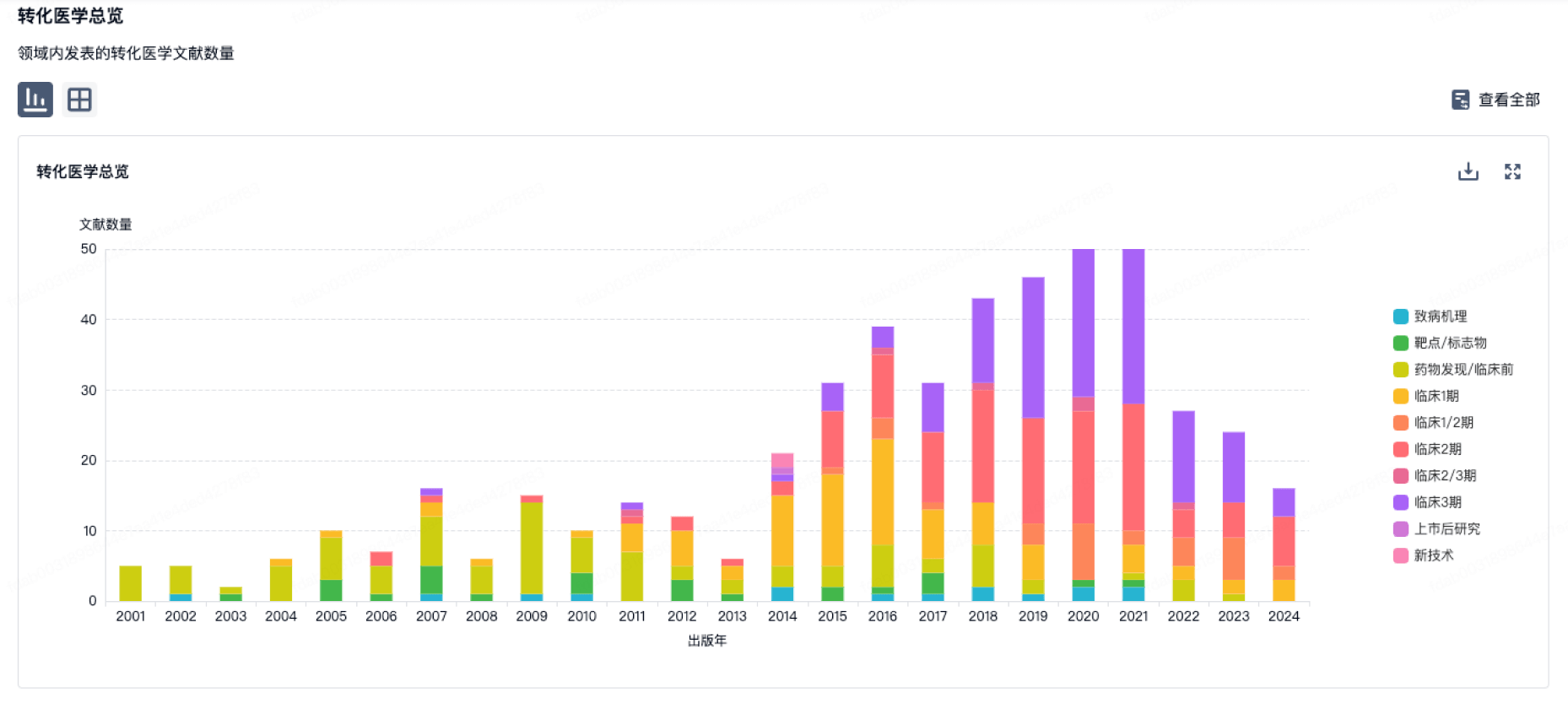
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
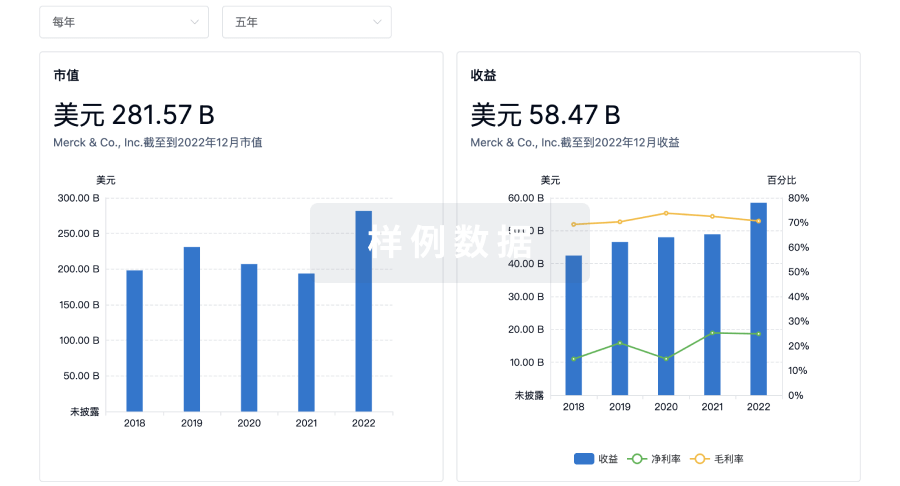
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
来和芽仔聊天吧
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用


