预约演示
更新于:2025-01-23
MSCs-derived exosomes(Shanghai Jiao Tong University)
更新于:2025-01-23
概要
基本信息
关联
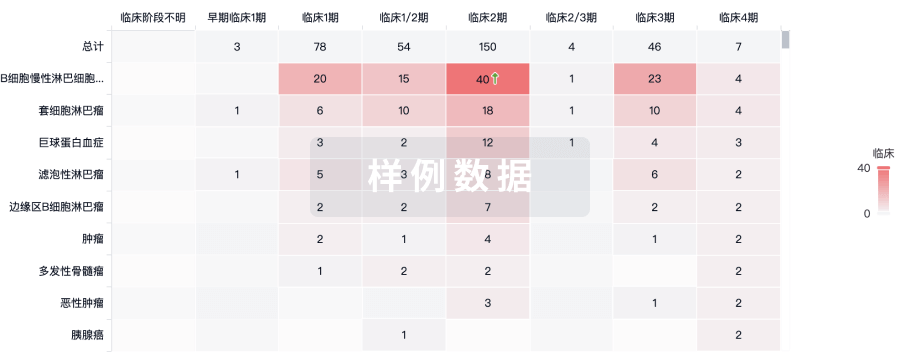
100 项与 MSCs-derived exosomes(Shanghai Jiao Tong University) 相关的临床结果
登录后查看更多信息
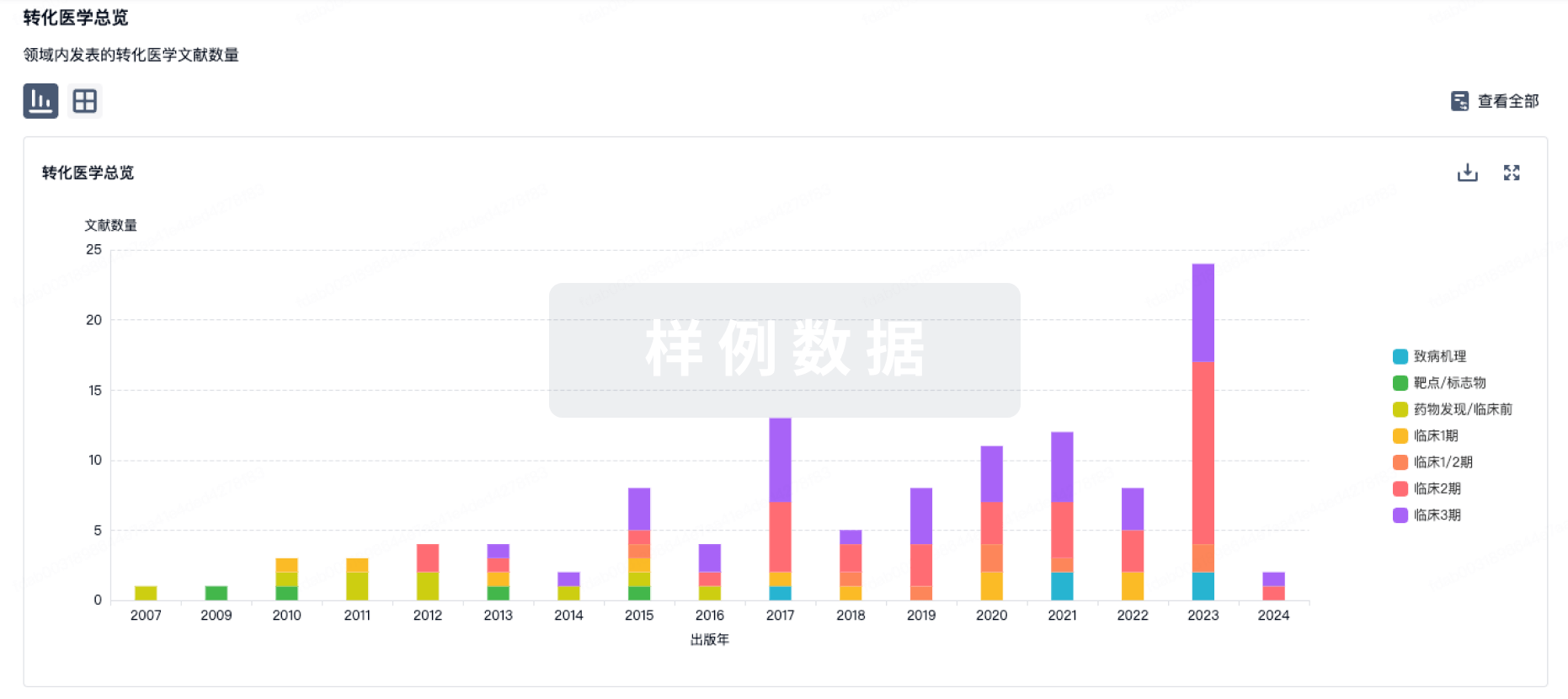
100 项与 MSCs-derived exosomes(Shanghai Jiao Tong University) 相关的转化医学
登录后查看更多信息
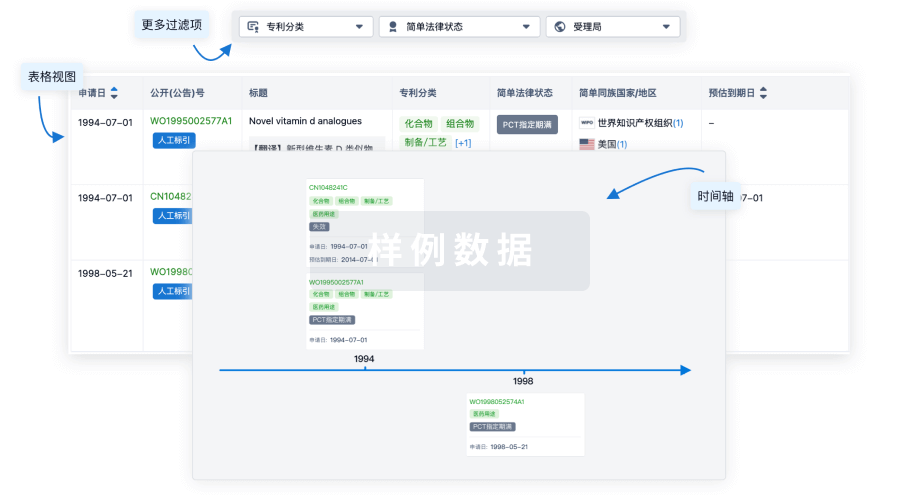
100 项与 MSCs-derived exosomes(Shanghai Jiao Tong University) 相关的专利(医药)
登录后查看更多信息
9
项与 MSCs-derived exosomes(Shanghai Jiao Tong University) 相关的文献(医药)2024-05-01·Biomedicine & Pharmacotherapy
Host-microbiota interactions in collagen-induced arthritis rats treated with human umbilical cord mesenchymal stem cell exosome and ginsenoside Rh2
Article
作者: Zhou, Zhongsheng ; Li, Yang ; Wu, Shuhui ; Jiang, Jinlan ; Liu, Te
2024-02-25·Sheng li xue bao : [Acta physiologica Sinica]
[Effects of human umbilical cord mesenchymal stem cells (MSCs)-derived exosomes on pulmonary vascular remodeling in hypoxic pulmonary hypertension].
Article
作者: Wang, Yu-Xiang ; Liu, Hong ; Zhang, Yu-Wei ; Ma, Lan ; Ge, Ri-Li ; Zhang, Qing-Qing
2023-05-01·Biomedicine & Pharmacotherapy
Depletion of gut microbiota resistance in 5×FAD mice enhances the therapeutic effect of mesenchymal stem cell-derived exosomes
Article
作者: Yan, Jun ; Mu, Xupeng ; Zhao, Jingtong ; Jiang, Hongyu ; Zhang, Xiaowen ; Liu, Te ; Hou, Xuejia ; Jiang, Jinlan ; Zhang, Fuqiang
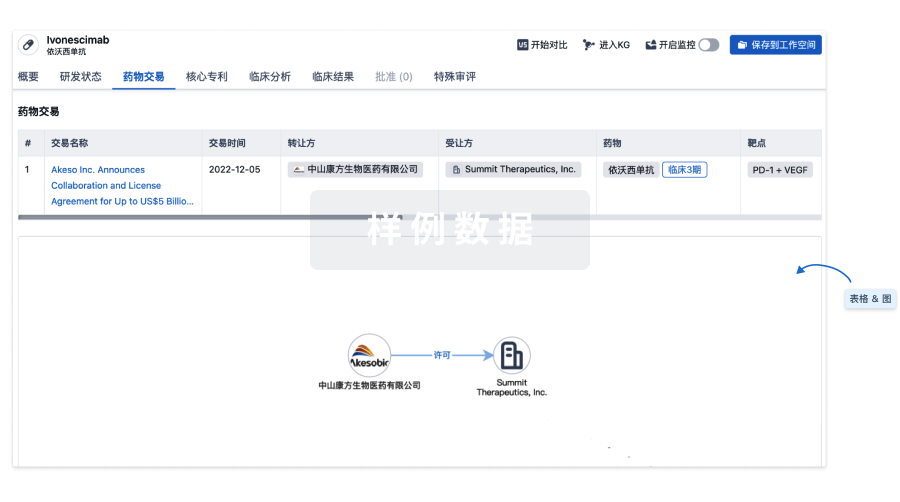
100 项与 MSCs-derived exosomes(Shanghai Jiao Tong University) 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 新型冠状病毒感染 | 临床1期 | - | - |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

来和芽仔聊天吧
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
