预约演示
更新于:2025-05-07
Huaiqihuang Granule
槐杞黄颗粒
更新于:2025-05-07
概要
基本信息
原研机构 |
在研机构 |
非在研机构- |
权益机构- |
最高研发阶段批准上市 |
最高研发阶段(中国)批准上市 |
特殊审评- |
登录后查看时间轴
关联
5
项与 槐杞黄颗粒 相关的临床试验NCT05772871
Compare the Efficacy and Safety of Prednisone Combined With Huaiqihuang Granule Versus Combined With Levamisole for Primary Nephrotic Syndrome in Children: A Prospective, Multi-center, Randomized, Double-blind, Non-inferiority Study
This non-inferiority study aims to compare the efficacy of Prednisone combined with Huaiqihuang Granule against Prednisone combined with Levamisole in the treatment of primary nephrotic syndrome (PNS) in children.
开始日期2023-04-26 |
NCT04623866
A Single Center Randomized Controlled Clinical Study on the Treatment of Children With Purpura Nephritis With Huaiqihuang Granules
About 20% children with allergic purpura develop nephritis syndrome or nephrotic syndrome, 1% to 7% to kidney failure or end-stage renal disease. Children with serious damage to health, significantly reduced quality of life and caused heavy economic burden to the family . As the pathogenesis of HSPN is complex, it is difficult to formulate an exact individualized treatment plan.
开始日期2020-11-01 |
申办/合作机构 |
NCT04263922
Huaiqihuang Granules in the Treatment of Primary Glomerulonephritis of Stage CKD3: a Randomized, Double-blind, Double-simulation, Positive Parallel Control Multi-center Clinical Study
This is a multicentre prospective, randomized, double-blind and imitation, positive-drug parallel controlled clinical trail. The objective of this study is to evaluate the efficacy and safety of Huaiqihuang Granule in patients with CKD stage 3 primary glomerulonephritis.
开始日期2020-06-30 |
申办/合作机构  大连医科大学附属第一医院 大连医科大学附属第一医院 [+2] |
100 项与 槐杞黄颗粒 相关的临床结果
登录后查看更多信息
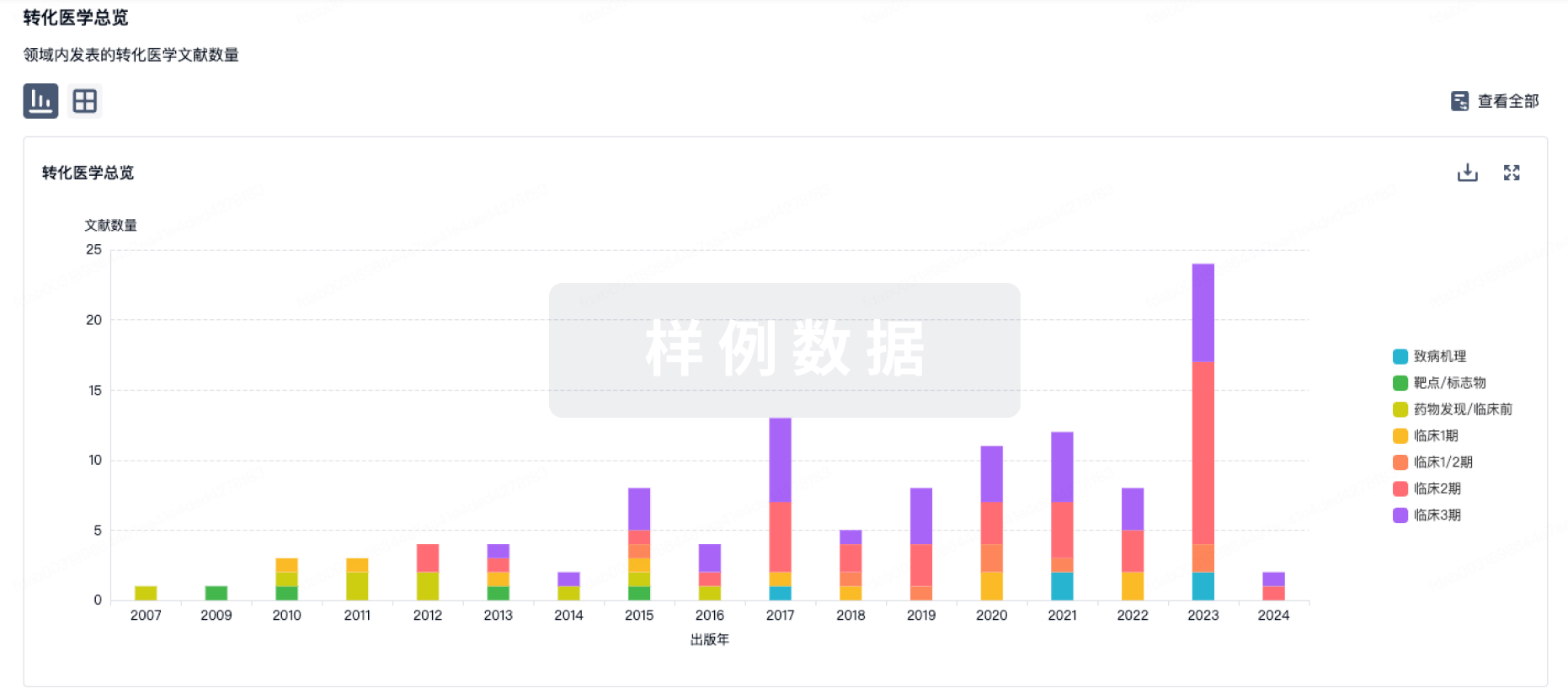
100 项与 槐杞黄颗粒 相关的转化医学
登录后查看更多信息
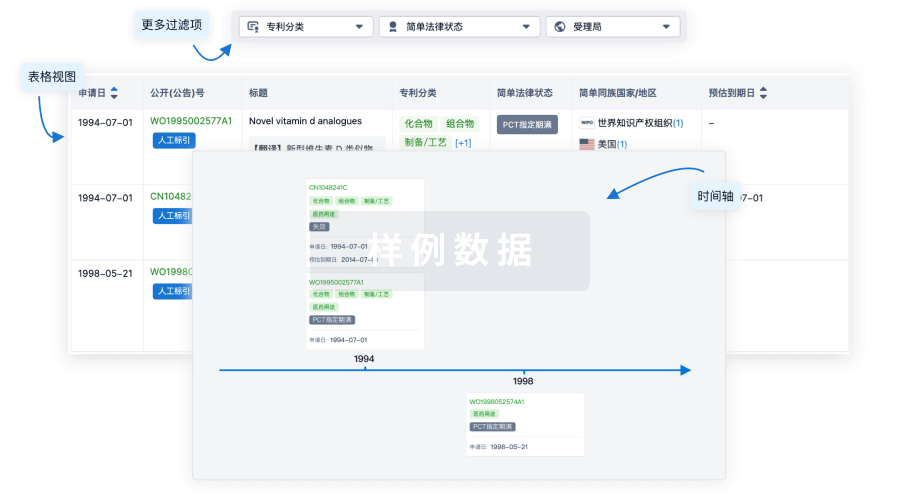
100 项与 槐杞黄颗粒 相关的专利(医药)
登录后查看更多信息
16
项与 槐杞黄颗粒 相关的文献(医药)2023-12-15·Medicine
Mechanism of Huaiqihuang in treatment of diabetic kidney disease based on network pharmacology, molecular docking and in vitro experiment
Article
作者: Wang, Junwei ; Ma, Guiqiao ; Ma, Chaojing ; Zhang, Peipei ; Shao, Jing ; Ma, Chanjuan ; Wang, Liping
2023-05-01·Pakistan journal of pharmaceutical sciences
Clinical efficacy and safety of fluticasone/salmeterol inhalation powder combined with huaiqihuang granules in the treatment of children with cough variant asthma.
Article
作者: Guo, Run ; Yang, Jing ; Guo, Yuanyuan ; Du, Shiyu ; Chen, Chao ; Xi, Ruiqian ; Gao, Chao ; Liu, Junting
2023-01-01·BioMed Research International
Investigation of the Active Compounds and Important Pathways of Huaiqihuang Granule for the Treatment of Immune Thrombocytopenia Using Network Pharmacology and Molecular Docking
Article
作者: Chen, Wenwen ; Kan, Hongtao ; Tao, Wanjun ; Yang, Jia ; Qin, Min ; XiaoYang
7
项与 槐杞黄颗粒 相关的新闻(医药)2024-01-21
·赛柏蓝
作者 | 白羽来源 | 米内网数据显示,补气补血类中成药近年在中国公立医疗机构终端市场规模保持快速增长,2022年首次突破50亿元大关,2023年上半年同比增长30%。01大涨30%幸福制药、红珊瑚、国药领跑近年中国公立医疗机构终端补气补血类中成药销售情况(单位:亿元)近年来在中医药政策利好推动下,相关用药市场规模持续扩容。数据显示,补气补血类中成药近年中国公立医疗机构终端市场规模快速增长,2022年首次突破50亿元大关,2023年上半年同比增长30.06%。从细分渠道来看,城市公立医院的市场份额最大,城市社区中心的市场份额快速扩容,且呈逐年上升趋势。从亚类来看,补血用药和补气用药是两大主力,合计市场份额占比超过90%;补气用药和自汗用药销售额增速均超过40%。厂家TOP20中,清华德人西安幸福制药、广东红珊瑚药业、国药广东环球制药位居前三,鲁南厚普制药凭借强劲增速上升至第四位,同时也是前五厂家中增速最快。0216个独家产品火了10亿大品种有望再创新高2023年上半年中国公立医疗机构终端补气补血类中成药产品TOP20(单位:亿元)注:销售额低于1亿元用*表示产品TOP20中,有16个独家品种,其中,生血宝合剂(清华德人西安幸福制药)、玉屏风颗粒(国药集团广东环球制药)、生血宁片(武汉联合药业)、益气维血胶囊和益气维血片(广东红珊瑚药业)、补中益气颗粒(北京汉典制药)等7个销售额均超过1亿元。从亚类来看,补血用药最多,有11个,补气用药有8个,玉屏风颗粒是唯一上榜的自汗用药。从增速来看,仅1个产品负增长;16个产品有双位数及以上增速,包括生脉饮、复方阿胶浆、生血宝合剂、玉屏风颗粒、归脾合剂、生血宁片、益气维血胶囊、益气维血片、生脉饮(党参方)、养心定悸胶囊、槐杞黄颗粒、归脾胶囊、十一味参芪片等。近年中国公立医疗机构终端生血宝合剂销售情况(单位:亿元)生血宝合剂是清华德人西安幸福制药的独家产品,拥有国家医保甲类、国家基药、中药保护品种等光环。近年在中国公立医疗机构终端生血宝合剂市场规模稳步攀升,2021-2022年销售额均超过10亿元,2023年上半年同比增长13.61%,全年有望再创新高。2023年8月,其官网发布消息,生血宝合剂入选《缺铁性贫血(萎黄病)中西医诊疗专家共识》,并获得首选推荐,该产品目前已入选10多个专家共识、指南、临床医学教材;同年11月,国家药监局发布公告,对清华德人西安幸福制药的生血宝合剂继续给予中药保护品种2级保护,期限为2023年11月27日-2030年7月20日,将进一步增强产品的市场竞争力。038个过亿品牌全线上扬鲁南跻身TOP3,健民、正大青春宝上榜2023年上半年中国公立医疗机构终端补气补血类中成药品牌TOP20(单位:亿元)注:销售额低于1亿元用*表示品牌TOP20中,8个销售额超1亿元,且均为正增长,清华德人西安幸福制药的生血宝合剂多年来占据“销冠”宝座,鲁南厚普制药的归脾合剂则挺进TOP3。从数量来看,广东红珊瑚药业、健民药业集团、正大青春宝药业等4家企业各有2个品牌上榜。从增速来看,黑龙江瑞格制药的生脉饮、东阿阿胶的复方阿胶浆等3个品牌翻倍,国药广东环球制药的玉屏风颗粒、鲁南厚普制药的归脾合剂、广东红珊瑚药业的益气维血片、河北永丰药业的养心定悸胶囊、启东盖天力药业的槐杞黄颗粒、正大青春宝药业的生脉胶囊6个品牌增速均超过30%。2023年上半年中国公立医疗机构终端归脾合剂TOP3品牌格局归脾合剂在近年中国公立医疗机构终端市场规模快速增长,2022年销售额突破3亿元大关,2023年上半年销售额已超过2021年全年。目前,归脾合剂有9家企业拥有生产批文,鲁南厚普制药的市场份额最大,2023年上半年销售额同比增长88.81%,挺进补气补血类中成药TOP3品牌。2023年12月,鲁南厚普制药的归脾合剂、川蛭通络胶囊、安神补脑液3款产品被认定为2023年山东知名品牌,为鲁南制药集团中成药大品种培育夯实基础的同时,也为临床应用指明方向。资料来源:米内网数据库、公司公告END医药代表交流群扫描下方二维码加入医药代理商转型交流群扫描下方二维码加入
上市批准医药出海
2024-01-17
·米内网
精彩内容米内网数据显示,补气补血类中成药近年在中国公立医疗机构终端市场规模保持快速增长,2022年首次突破50亿元大关,2023年上半年同比增长30%。产品TOP20中,16个独家品种“霸屏”,其中7个销售额超1亿元,生血宝合剂有望全年创新高。品牌TOP20中,鲁南厚普制药的归脾合剂跻身前三,国药、健民、正大青春宝等上榜。大涨30%!幸福制药、红珊瑚、国药领跑近年中国公立医疗机构终端补气补血类中成药销售情况(单位:亿元)来源:米内网中国公立医疗机构药品终端竞争格局近年来在中医药政策利好推动下,相关用药市场规模持续扩容。米内网数据显示,补气补血类中成药近年在中国城市公立医院、县级公立医院、城市社区中心以及乡镇卫生院(简称中国公立医疗机构)终端市场规模快速增长,2022年首次突破50亿元大关,2023年上半年同比增长30.06%。从细分渠道来看,城市公立医院的市场份额最大,城市社区中心的市场份额快速扩容,且呈逐年上升趋势。从亚类来看,补血用药和补气用药是两大主力,合计市场份额占比超过90%;补气用药和自汗用药销售额增速均超过40%。厂家TOP20中,清华德人西安幸福制药、广东红珊瑚药业、国药广东环球制药位居前三,鲁南厚普制药凭借强劲增速上升至第四位,同时也是前五厂家中增速最快。16个独家产品火了,10亿大品种有望再创新高2023年上半年中国公立医疗机构终端补气补血类中成药产品TOP20(单位:亿元)来源:米内网中国公立医疗机构药品终端竞争格局注:销售额低于1亿元用*表示产品TOP20中,有16个独家品种,其中,生血宝合剂(清华德人西安幸福制药)、玉屏风颗粒(国药集团广东环球制药)、生血宁片(武汉联合药业)、益气维血胶囊和益气维血片(广东红珊瑚药业)、补中益气颗粒(北京汉典制药)等7个销售额均超过1亿元。从亚类来看,补血用药最多,有11个,补气用药有8个,玉屏风颗粒是唯一上榜的自汗用药。从增速来看,仅1个产品负增长;16个产品有双位数及以上增速,包括生脉饮、复方阿胶浆、生血宝合剂、玉屏风颗粒、归脾合剂、生血宁片、益气维血胶囊、益气维血片、生脉饮(党参方)、养心定悸胶囊、槐杞黄颗粒、归脾胶囊、十一味参芪片等。近年中国公立医疗机构终端生血宝合剂销售情况(单位:亿元)来源:米内网中国公立医疗机构药品终端竞争格局生血宝合剂是清华德人西安幸福制药的独家产品,拥有国家医保甲类、国家基药、中药保护品种等光环。近年在中国公立医疗机构终端生血宝合剂市场规模稳步攀升,2021-2022年销售额均超过10亿元,2023年上半年同比增长13.61%,全年有望再创新高。2023年8月,公司官网发布消息,生血宝合剂入选《缺铁性贫血(萎黄病)中西医诊疗专家共识》,并获得首选推荐,该产品目前已入选10多个专家共识、指南、临床医学教材;同年11月,国家药监局发布公告,对清华德人西安幸福制药的生血宝合剂继续给予中药保护品种2级保护,期限为2023年11月27日-2030年7月20日,将进一步增强产品的市场竞争力。8个过亿品牌全线上扬!鲁南跻身TOP3,健民、正大青春宝上榜2023年上半年中国公立医疗机构终端补气补血类中成药品牌TOP20(单位:亿元)来源:米内网中国公立医疗机构药品终端竞争格局注:销售额低于1亿元用*表示品牌TOP20中,8个销售额超1亿元,且均为正增长,清华德人西安幸福制药的生血宝合剂多年来占据“销冠”宝座,鲁南厚普制药的归脾合剂则挺进TOP3。从数量来看,广东红珊瑚药业、健民药业集团、正大青春宝药业等4家企业各有2个品牌上榜。从增速来看,黑龙江瑞格制药的生脉饮、东阿阿胶的复方阿胶浆等3个品牌翻倍,国药广东环球制药的玉屏风颗粒、鲁南厚普制药的归脾合剂、广东红珊瑚药业的益气维血片、河北永丰药业的养心定悸胶囊、启东盖天力药业的槐杞黄颗粒、正大青春宝药业的生脉胶囊6个品牌增速均超过30%。2023年上半年中国公立医疗机构终端归脾合剂TOP3品牌格局来源:米内网中国公立医疗机构药品终端竞争格局归脾合剂在近年中国公立医疗机构终端市场规模快速增长,2022年销售额突破3亿元大关,2023年上半年销售额已超过2021年全年。目前,归脾合剂有9家企业拥有生产批文,鲁南厚普制药的市场份额最大,2023年上半年销售额同比增长88.81%,挺进补气补血类中成药TOP3品牌。2023年12月,鲁南厚普制药的归脾合剂、川蛭通络胶囊、安神补脑液3款产品被认定为2023年山东知名品牌,为鲁南制药集团中成药大品种培育夯实基础的同时,也为临床应用指明方向。资料来源:米内网数据库、公司公告注:米内网《中国公立医疗机构药品终端竞争格局》,统计范围是:中国城市公立医院、县级公立医院、城市社区中心以及乡镇卫生院,不含民营医院、私人诊所、村卫生室;上述销售额以产品在终端的平均零售价计算。如有疏漏,欢迎指正!本文为原创稿件,转载请注明来源和作者,否则将追究侵权责任。投稿及报料请发邮件到872470254@qq.com稿件要求详询米内微信首页菜单栏商务及内容合作可联系QQ:412539092【分享、点赞、在看】点一点不失联哦
医药出海
2023-12-21
·赛柏蓝
近年来,补气补血类中成药在中国零售药店终端的市场规模稳步攀升,2022年销售额超过120亿元,2023年上半年同比增长超过25%。从TOP20来看,实体药店6个产品销售超过1亿元,超20亿大品种继续领跑,黄芪精晋身前三,东阿阿胶、宏济堂、扬子江等上榜;网上药店增速迅猛,5个产品暴涨翻倍,同仁堂6大品牌霸屏。近年中国零售药店终端补气补血类中成药销售情况(单位:亿元)从亚类来看,补血用药和补气用药仍然是两大销售额主力,增速均超过20%,而自汗用药则是增速最快的亚类,超过50%。01实体药店:超20亿大品种领跑独家产品暴涨1124%近年中国城市实体药店补气补血类中成药市场规模稳步攀升,2023年上半年销售额超过50亿元。从厂家格局来看,东阿阿胶、山东福牌阿胶、山东宏济堂制药集团位居前三。产品TOP20中,6个销售额超过1亿元,阿胶以超20亿元继续领跑,黄芪精凭借超过60%的增速晋身TOP3。从亚类来看,补气用药多达11个,其次是补血用药有5个,自汗用药和补气补血类其它用药各有2个。2023年上半年中国城市实体药店补气补血类中成药产品TOP20(单位:亿元)注:销售额低于1亿元用*表示6个独家产品,分别是复方阿胶浆(东阿阿胶)、益安宁丸(同溢堂药业)、玉屏风颗粒(国药广东环球制药)、当归补血口服液(郑州协和制药)、潞党参口服液(山西正来制药)、气血固本口服液(深圳市长寿药业),其中,复方阿胶浆(东阿阿胶)和益安宁丸(同溢堂药业)销售额均超过1亿元,潞党参口服液(山西正来制药)是产品TOP20中增速最快的产品,同比增长达1124.05%。品牌TOP20中,8个销售额超过1亿元, 东阿阿胶的阿胶是唯一超10亿元品牌。此外,4个品牌新上榜,分别是山西正来制药的潞党参口服液、九芝堂的阿胶、湖南东健药业的阿胶、雷允上药业集团的健延龄胶囊,同比增长分别为1124.05%、311.12%、239.38%、84.90%。2023年上半年中国城市实体药店补气补血类中成药品牌TOP20(单位:亿元)注:销售额低于1亿元用*表示02网上药店大涨超50%同仁堂6大品牌霸屏TOP20补气补血类中成药近年在中国网上药店市场规模快速增长,2023年上半年增速超过50%,销售额接近10亿元。从厂家格局来看,东阿阿胶、北京同仁堂、同溢堂药业位居前三。产品TOP20合计市场份额占比超过80%,阿胶、复方阿胶浆、益安宁丸位居前三。从增速来看,涨多跌少,复方阿胶浆、黄芪精、生脉饮(党参方)、生脉饮、槐杞黄颗粒暴涨翻倍,其中黄芪精增速最快,达181.63%。从亚类来看,补气用药多达12个,其次是补血用药有6个,自汗用药有2个。2023年上半年中国网上药店补气补血类中成药产品TOP20(单位:亿元)注:销售额低于1亿元用*表示品牌TOP20中,东阿阿胶的复方阿胶浆和阿胶、扬子江江苏龙凤堂中药的黄芪精、北京同仁堂科技制药的生脉饮(党参方)和生脉饮、通药制药集团的益气养血口服液、启东盖天力药业的槐杞黄颗粒7个品牌暴涨翻倍,国药广东环球制药的玉屏风颗粒、河南济世药业的参苓白术丸、北京同仁堂制药的参苓白术丸、九芝堂的归脾丸(浓缩丸)4个品牌增速均超过50%。从数量来看,北京同仁堂最多,有6个品牌上榜,分别是生脉饮(党参方)、参苓白术散、生脉饮、参苓白术丸、阿胶、人参归脾丸。2023年上半年中国网上药店补气补血类中成药品牌TOP20(单位:亿元)注:销售额低于1亿元用*表示资料来源:米内网数据库、公司公告注:统计范围是:全国地级及以上城市实体药店,不含县乡村药店;《中国网上药店药品终端竞争格局》,统计范围是:全国网上药店所有药品数据,包括天猫、京东等第三方平台及私域平台上所有网上药店药品数据;上述销售额以产品在终端的平均零售价计算。如有疏漏,欢迎指正。END作者 | 白羽来源 | 米内网赛柏蓝药械交流群扫描下方二维码加入医药代理商转型交流群扫描下方二维码加入
医药出海核酸药物
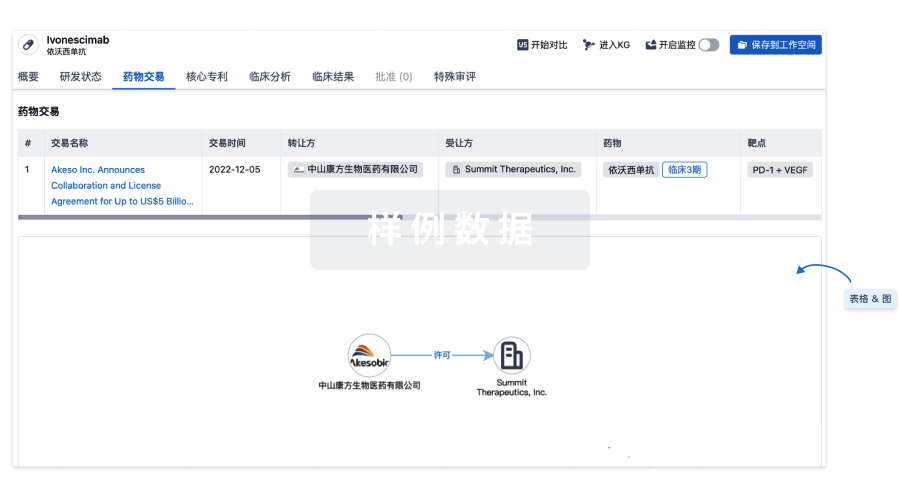
100 项与 槐杞黄颗粒 相关的药物交易
登录后查看更多信息
研发状态
10 条最早获批的记录, 后查看更多信息
登录
| 适应症 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|
| 普通感冒 | 中国 | 2020-06-24 | |
| 便秘 | 中国 | 2020-06-24 |
登录后查看更多信息
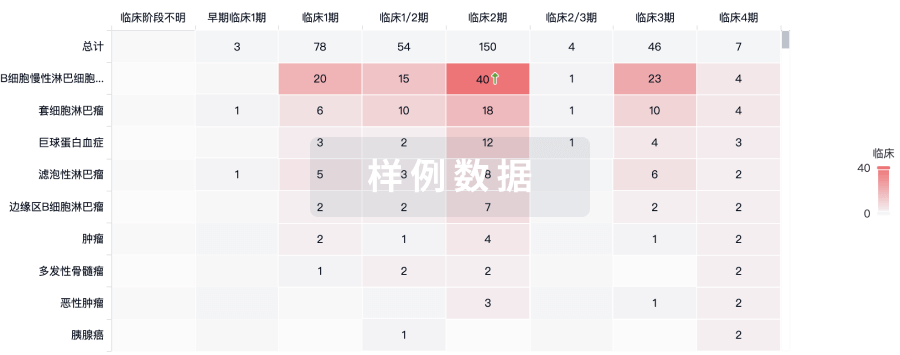
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用

