预约演示
更新于:2025-05-16
Sirtratumab Vedotin
更新于:2025-05-16
概要
基本信息
药物类型 ADC |
别名 sirtratumab vedotin、AGS-15E、AGS15C–SGD-1006 + [5] |
作用方式 抑制剂 |
作用机制 SLITRK6抑制剂(神经突触相关蛋白SLITRK6抑制剂)、微管蛋白抑制剂 |
在研适应症 |
非在研适应症 |
原研机构 |
最高研发阶段临床1期 |
首次获批日期- |
最高研发阶段(中国)- |
特殊审评- |
登录后查看时间轴
结构/序列
分子式C39H67N5O7 |
InChIKeyDASWEROEPLKSEI-UIJRFTGLSA-N |
CAS号474645-27-7 |
查看全部结构式(2)
使用我们的ADC技术数据为新药研发加速。
登录
或

Sequence Code 9509781H

来源: *****
Sequence Code 9509790L

来源: *****
关联
1
项与 Sirtratumab Vedotin 相关的临床试验NCT01963052
A Phase 1 Study of the Safety and Pharmacokinetics of Escalating Doses of AGS15E Given as Monotherapy in Subjects With Metastatic Urothelial Cancer
The objectives of this study are to assess the safety, pharmacokinetics, immunogenicity and anti-tumor activity of AGS15E in subjects with metastatic urothelial cancer who failed at least one prior chemotherapy regimen for metastatic disease.
开始日期2013-11-14 |
申办/合作机构 |
100 项与 Sirtratumab Vedotin 相关的临床结果
登录后查看更多信息
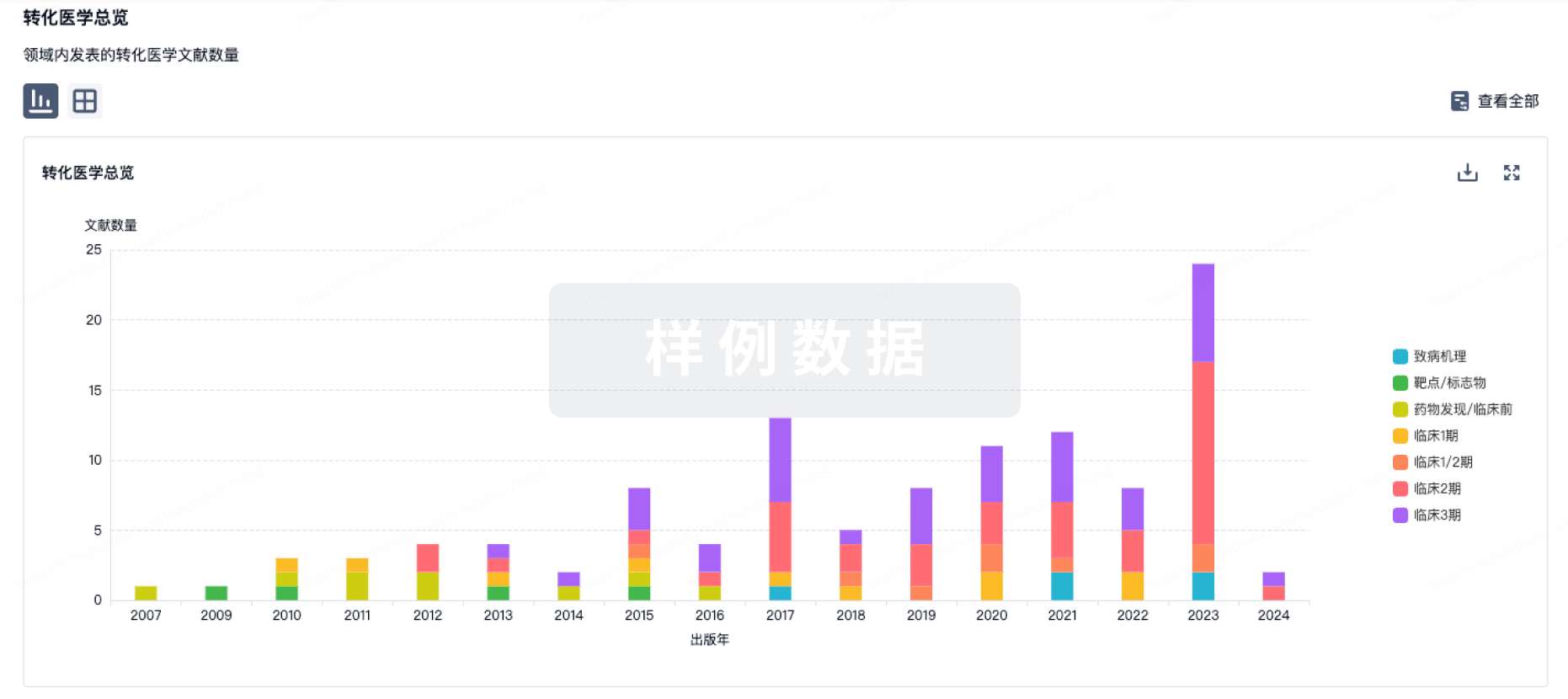
100 项与 Sirtratumab Vedotin 相关的转化医学
登录后查看更多信息
100 项与 Sirtratumab Vedotin 相关的专利(医药)
登录后查看更多信息
598
项与 Sirtratumab Vedotin 相关的文献(医药)2025-12-31·mAbs
A bispecific antibody-drug conjugate targeting pCAD and CDH17 has antitumor activity and improved tumor-specificity
作者: Gesner, Thomas ; Logel, Claude ; Xie, Kathleen T. ; Cebe, Regis ; Wu, Nila C. ; Li, Xun ; Shi, Xingyi ; Velazquez, Roberto ; Simmons, Quincey ; Tschantz, William R. ; Barzaghi-Rinaudo, Patrizia ; Korn, Joshua ; Sagar, Vivek ; Hainzl, Dominik ; Malamas, Anthony ; Mercan, Samuele ; Green, Andrew ; McLaughlin, Margaret ; Huber, Thomas ; Mueller, Kathrin ; Synan, Alyssa ; D’Alessio, Joseph A.
P-cadherin (pCAD) and LI-cadherin (CDH17) are cell-surface proteins belonging to the cadherin superfamily that are both highly expressed in colorectal cancer.This co-expression profile presents a novel and attractive opportunity for a dual targeting approach using an antibody-drug conjugate (ADC).In this study, we used a unique avidity-driven in vitro screening approach to generate pCAD x CDH17 bispecific antibodies that selectively target cells expressing both antigens over cells expressing only pCAD or only CDH17.Based on in vitro binding and inhibition of cell proliferation results, we selected a lead bispecific antibody to link to the cytotoxic payload monomethyl auristatin E (MMAE) to generate a pCAD x CDH17 bispecific MMAE ADC.In in vivo dual flank mouse models, we demonstrated antitumor activity of the bispecific ADC in tumors expressing both antigens but not in tumors expressing only pCAD or only CDH17.Overall, the preclin. data presented here support the proof-of-concept bispecific antibody discovery approach, demonstrating a rational design for screening antibodies by prioritizing cross-arm avid IgGs to target dual-pos. cells.
2025-04-16·BIOCONJUGATE CHEMISTRY
Mechanistic Characterization of the Potency of THIOMAB Antibody–Drug Conjugates Targeting Staphylococcus aureus and ETbR-Expressing Tumor Cells Using Quantitative LC-MS/MS Analysis of Intracellular Drug Accumulation
Article
作者: Hernandez-Barry, Hilda ; Asundi, Jyoti ; Vandlen, Richard ; Zhang, Donglu ; Pillow, Thomas ; Loyet, Kelly M. ; Hazenbos, Wouter L.W. ; Liu, Yichin ; dela Cruz-Chuh, Josefa ; Wu, Cong ; Kozak, Katherine R. ; Kajihara, Kimberly K.
THIOMAB drug conjugate (TDC) technology provides site-specific conjugation of linker drugs to antibodies, allowing for targeted delivery of the payload. While a direct measurement of TDC cytotoxic potency allows efficient screening and confirmation that new drugs conjugated to antibodies result in proper processing in cells, additional mechanistic characterization is often needed to provide information-rich data to guide further optimization of TDC design. For example, a quantitative understanding of how TDCs are processed intracellularly can help determine which processing step is impacting payload delivery and thereby inform the basis of the TDC efficacy. Here, we measure the cellular accumulation of two different TDC drug payloads: MAPK (mitogen-activated protein kinase) pathway inhibitor targeting ETbR-expressing tumor cells and an antibiotic active against Staphylococcus aureus with an in vitro cell-based drug release LC-MS/MS assay in a 96-well format. This assay allowed us to correlate the cellular potency of each unconjugated molecule with the amount of payload that accumulated inside the cell. In the case of the pathway inhibitor drug, the biochemical characterization of TDC processing by cathepsin B and purified human liver enzyme extract demonstrated a correlation between the efficiency of the linker drug cleavage and intracellular payload accumulation. For the antibody-antibiotic conjugate, kinetic analysis of intracellular free drug retention provided valuable insight into the chemistry modifications needed for an efficient TDC. Taken together, we demonstrated the utility of quantitative LC-MS/MS assays as one tool in guiding the design of more effective TDCs via the mechanistic release characterization of two distinct payloads.
2025-04-10·JOURNAL OF MEDICINAL CHEMISTRY
NIR-II aza-BODIPY Platform for the Development of a Fluorescent Antibody Drug Conjugate
Article
作者: Wegner, K. David ; Paul, Catherine ; Pipier, Angélique ; Chazeau, Elisa ; Sancey, Lucie ; Ghiringhelli, François ; Goze, Christine
Real-time imaging of antibody-drug conjugates (ADCs) offers valuable insights for assessing tumor targeting specificity, monitoring therapeutic efficacy, and detecting off-target accumulation that may cause adverse effects. To enable precise tracking, we developed a versatile fluorescent platform based on an NIR-II emitting aza-BODIPY dye, which can be site-specifically grafted onto an IgG1 antibody to generate well-defined fluorescent ADCs. As a proof of concept, we synthesized an HER2-targeting trastuzumab immunoconjugate bearing a NIR-II aza-BODIPY fluorophore. The cytotoxic monomethyl auristatin E (MMAE) payload was introduced in the final step, resulting in a trackable and homogeneous ADC suitable for both in vitro and in vivo investigations. The resulting Trastu-azaNIRII-MMAE selectively accumulated in HER2-positive subcutaneous tumors, significantly reducing the tumor growth. Using NIR-II optical imaging, a single injection of the NIR-II-ADC allowed for the detection of the conjugate over a period of more than one month, highlighting its potential for long-term tracking and therapeutic applications.
2
项与 Sirtratumab Vedotin 相关的新闻(医药)2024-04-15
当前,抗体药物偶联物(ADC)已经对临床肿瘤治疗格局产生了深远的影响,它俨然成为肿瘤治疗领域中一颗璀璨的明星,多种新型的ADC药物如雨后春笋般涌现。随着更多ADC药物的临床试验数据逐渐公布,以及个体化和精准医疗理念的普及与推广,ADC将在肿瘤治疗的舞台上扮演更加举足轻重的角色。在近期举办的2024年美国癌症研究协会(AACR)年会上,多款来自BioBAY企业的ADC在研管线亮相,其中有大量新靶点ADC以及近期备受瞩目的双抗ADC。2024 AACR BioBAY企业部分ADC报告管线信达生物:单抗双抗ADC两手抓信达生物此次在大会上公布了旗下一系列肿瘤管线的多项最新临床前数据,其中包括IBI3001和IBI343两款ADC项目,并入选重磅研究(Late-Breaking Research)。IBI3001是一款潜在全球首创针对B7-H3和EGFR的双特异性ADC,采用经临床验证的SYNtecanE®定点偶联平台。IBI3001具有多重抗肿瘤的机制:(1)增强的EGFR信号阻断;(2)EGFR与B7-H3介导的药物内吞与细胞杀伤;(3)强效的ADC旁观效应。经过优化的B7-H3臂不但加强了EGFR信号阻断的效果,同时也降低了EGFR靶点的毒性。IBI3001在多个实体瘤的体内外模型中都显示强效的肿瘤杀伤效果,且有高耐受性,治疗窗口高达40倍。IBI343是一款具有全球首创潜力的靶向Claudin 18.2的ADC分子,基于Synaffix的GlycoConnect®实现了对细胞毒素Exatecan的糖基定点偶联。IBI343在多种不同表达量的肿瘤细胞系上展现了良好的Claudin 18.2特异性的体外杀伤活性,并在多种人源肿瘤异种移植小鼠模型上展现了良好的肿瘤抑制活性。基于糖基的定点偶联技术显著增强了整个ADC的稳定性。IBI343在恒河猴的GLP毒理实验中展现了良好的安全性,并在高至30 mg/kg的剂量下耐受性良好。目前,Claudin18.2 ADC 主要开发的适应症为二三线胃癌,现有疗法疗效有限。中国有2款进入注册三期,除IBI343外,还有康诺亚/阿斯利康合作开发的CMG901。2024年2月,信达生物在Clinicaltrials.gov网站注册了IBI343治疗Claudin18.2阳性、HER2阴性胃癌的三期临床试验,是全球首款进入三期临床阶段的Claudin18.2 ADC新药。2024年3月7日,阿斯利康在药品临床试验登记与信息公示平台网站上注册了CMG901二线或二线以上治疗晚期或转移性胃癌的三期临床试验。映恩生物:充分发挥平台优势此次大会,映恩生物公布了基于其自主研发的抗肿瘤ADC平台DITAC开发的DB-1310、DB-1311创新项目的研究成果。DB-1310是一款靶向HER3的ADC产品。其在临床前研究中表现出优异的肿瘤抑制效果和安全性。并且在与EGFR小分子抑制剂联合使用中表现出优秀的协同抑制肿瘤效果。作为新一代的ADC分子,其将有可能成为广大癌症患者的新治疗选择。DB-1310目前处于一项在晚期/转移性实体瘤受试者中评估安全性、耐受性、药代动力学和初步抗肿瘤活性的I/IIa期、多中心、开放性、非随机首次人体研究阶段。DB-1311是映恩生物靶向B7H3的第三代ADC产品,也是基于DITAC平台开发,在多种肿瘤模型中显示出强大的抗肿瘤活性,并且在临床前安全评估中展现出良好的安全性和药代动力学特征。DB-1311在未来临床应用中具有潜在的广阔治疗窗口。映恩生物目前正在开展一项评估DB-1311在晚期/转移性实体瘤受试者中的安全性、耐受性、药代动力学和初步抗肿瘤活性的I/IIa期、多中心、开放性、首次人体研究。宜联生物:YL211——罗氏与中国本土创新药企的重磅合作YL211是特异性靶向c-MET的下一代抗体偶联药物。c-MET为受体酪氨酸激酶(RTK)家族的成员之一,与肿瘤的形成、侵袭性生长和转移密切相关,是治疗上皮间质转化的关键靶点。YL211目前处于临床申报阶段,采用了宜联生物新一代TMALIN ADC平台技术,并配合以高特异性的c-MET抗体。YL211已在多种临床前肿瘤模型及安全性评价实验中展现出极具潜力的疗效及安全性。2024年1月2日,宜联生物与罗氏达成约10.5亿美元全球合作和许可协议,宜联生物将与罗氏中国创新中心(CICoR)共同合作推动YL211项目进入临床1期试验阶段,并交由罗氏负责后续全球范围内进一步开发和商业化工作。启德医药:GQ1010疗效优于DS1062和TrodvyGQ1010是基于启德医药独特的iLDC技术、可切割“开环”连接子以及新型拓扑异构酶I抑制剂开发的靶向Trop2创新ADC药物。临床前研究表明,在测试的各种Trop2+癌症细胞系中,GQ1010表现出比DS1062更强的体外细胞毒性和更强的旁观者杀伤力。在不同的CDX模型(包括TNBC、胃癌、头颈部(H&N)和胰腺癌)中进一步显示出强大的体内抗肿瘤活性,疗效优于DS1062和Trodvy,与体外数据一致。目前同类产品中,全球仅有Trodvy(吉利德)上市,DS1062(Dato-DXd,第一三共/阿斯利康)和SKB264(sacituzumab tirumotecan,科伦博泰/默沙东)已申报上市。2023年4月,启德医药已将GQ1010除大中华区(中国大陆、香港、澳门和台湾)外的全球开发和商业化权益独家授权给Pyramid,获得2000万美元的首付款和最高可达10亿美元的里程碑付款,以及基于净销售额计算的分级特许权使用费。2024年2月22日,CDE官网公示,启德医药自主研发的 Trop-2 ADC药物GQ1010注射液申报临床。普方生物:两个ADC披露靶点信息SLITRK6在某些上皮性肿瘤中高表达,包括尿路上皮、肺部、乳腺癌和胶质母细胞瘤,而在正常组织中表达微弱。目前布局该靶点的只有安斯泰来/Seagen的ADC药物Sirtratumab vedotin,已经在膀胱癌和尿路上皮癌中进行了概念验证,其中尿路上皮癌1期临床已完成,结果发表在2016年 ASCO 上,整体ORR为30%。PRO1106是由靶向SLITRK6的人源化IgG1和基于拓扑异构酶1抑制剂的连接子-载荷 sesutecan 组成,该链接子-载荷已经在之前多个新药的临床研究中经过验证。体外试验显示,PRO1106 的靶标结合能力优于Sirtratumab;在膀胱癌和食管鳞癌细胞来源异种移植模型中,PRO1106 显示出强大的肿瘤生长抑制作用。在动物模型中,表现出比 Sirtratumab vedotin 更稳定的PK,循环中毒素释放极小,且未观察到明显毒性。总之,PRO1106是建立在经临床验证的连接子-载荷基础上、针对经临床验证的靶点的ADC,且在临床前药理学研究中显示出有希望的数据。由于皮肤中SLITRK6的表达几乎可以忽略不计,与当前膀胱癌标准 ADC 疗法(enfortumab vedotin)在患者中导致显著的皮肤相关毒副作用相比,PRO1106 可能为该类患者提供一种新的选择。另一款PRO1286,靶点为EGFR/MET,目前同靶点ADC药物共有9款,进展最快的是阿斯利康/BSP Pharmaceuticals 的 AZD9592,已进入临床1期,其余8款均为国内企业研发,且均处于临床前阶段。新型抗体药物研发是BioBAY当下的重点招商方向之一。近年来,BioBAY围绕生物医药产业,重点布局抗体偶联药物(ADC)、核酸药物、细胞与基因治疗(CGT)、IT+BT等产业细分赛道,BioBAY药企创新实力愈发受到国际市场的持续关注。1月2日,宜联生物宣布与罗氏达成全球合作和许可协议,双方将合作开发靶向间质表皮转化因子(c-MET)的下一代抗体偶联(ADC)药物候选产品YL211,用于治疗实体瘤。根据协议条款,交易金额超过10亿美元。4月3日,普方生物(ProfoundBio)与丹麦哥本哈根和美国纳斯达克两地上市企业Genmab A/S与达成18亿美元全现金收购协议。普方生物成为了中国第一家被收购的ADC公司,18亿美元的收购价格也刷新了中国Biotech被收购价格的纪录。目前,BioBAY已聚集620余家生物医药高科技创新企业、35000名高层次科技人才,形成了创新药研发、高端医疗器械、生物技术三大重点产业集群。下一步,BioBAY将持续强化企业创新主体地位,以更高水平推动创新链、产业链、资金链、人才链深度融合,不断提升政策体系、产业生态、创新活力,全力打造国际一流生物医药创新策源地、世界级生物医药产业地标核心区。▌文章来源:网络信息整理责编:何文正审核:任旭推荐阅读18亿美元!国内Biotech收购价新纪录花落BioBAY涉及创新药!AACR会议上BioBAY企业惊艳亮相国产ADC出海交易TOP10,BioBAY独占5席!
抗体药物偶联物临床3期AACR会议临床2期
2024-03-12
2024 年美国癌症研究协会(AACR)年会将于 4 月 5 日~10 日在美国圣地亚哥召开,目前,官网已经公布了部分摘要信息,Insight 数据库也已收录了 800+ 数据。鉴于临床结果相关的摘要正文将在会议开始当天公布,本文从已公布摘要中选取了部分国内企业的 ADC 项目进行分享。这其中不少是首次披露的新项目,或是首次公布已有项目的靶点、载荷信息等。开篇之前,先通过 Insight 数据库窥视一下当前全球 ADC 药物热门靶点 Top20,以辅助了解本文所述国内企业 ADC 靶点竞争程度。ADC 药物热门靶点 Top20来自:Insight 数据库网页版(下文如无特殊标注,为统一来源)以下,笔者主要从靶点的角度,选取竞争不是非常激烈的项目做简要介绍。恒瑞医药:5 款 ADC 亮相,4 个新项目首次公开恒瑞医药亮相 2024AACR 项目 DP03923-000-9106;靶点:LIV-1LIV-1 是锌转运蛋白家族的成员,因为其在肿瘤中表达广泛,而正常组织表达有限,使 LIV-1 成为 ADC 研发的有希望靶点。目前,该靶点全球在研 ADC 药物只有 7 款,进展最快的是 Seagen/默沙东的 Ladiratuzumab vedotin,已进入 II 期临床。初步临床结果显示,Ladiratuzumab vedotin 在 TNBC 中有很好的疗效(ORR = 32%),但 HR+/HER2-乳腺癌没有反应(ORR = 0%),且观察到典型的 MMAE 相关不良事件。SDP03923-000-9106 则是恒瑞研发的一款靶向 LIV-1 ADC,采用了可裂解的 linker 加上恒瑞自主研发的强效拓扑异构酶 I 抑制剂依沙替康衍生物(推测为 DXh),DAR 为 6。在 LIV-1 高表达乳腺癌细胞系中,SDP03923-000-9106 表现出较强的抑制作用,IC50 为 5.36 nM。在 LIV-1 高表达患者来源的乳腺癌模型中,3 mg/kg 和 10 mg/kg 剂量下均显示出明显的肿瘤消退,并且 3 mg/kg 剂量下,SDP03923-000-9106 显示出比 BMK-MMAE(恒瑞根据公开的 Ladiratuzumab vedotin 结构合成)更强的抗肿瘤活性 (TGI: 109%)。这些临床前的研究结果支持该药物进入临床研究,恒瑞在 AACR 摘要中表示已经向 NMPA 提交 IND 申请。 HRA00130-C004;靶点:DLL3DLL3 在 SCLC 和其他高级别神经内分泌肿瘤细胞表面上调和异常表达,而在正常组织中的表达有限,因此,DLL3 被认为是治疗 SCLC 等肿瘤的潜力靶点。其实,在很早的时候艾伯维就布局了靶向 DLL3 的 ADC 药物 Rovalpituzumab tesirine(Rova-T,引进自 Stemcentrx,载荷:DNA 交联剂),但在 2019 年宣布停止开发,原因是 Rova-T 作为晚期 SCLC 一线维持治疗的一项 3 期试验显示,与安慰剂相比,Rova-T 并没有显示出生存获益。业内认为 Rova-T 失败的原因之一可能是毒素,而不是靶点问题,因此纷纷进行了改毒素、用新的偶联技术继续探索向 DLL3 的 ADC 药物。全球同靶点在研 ADC 项目共 8 个,除艾伯维的项目外,进展最快的是宜联生物,已进入 I 期临床。HRA00130-C004 是一款具有旁观者效应、高 DAR 值的 DLL3 ADC 药物,将恒瑞自研的拓扑异构酶 I 抑制剂 DXh 通过一个可裂解的 Linker 与人源化 IgG1 抗体连接。在旁观者杀伤体内实验中,HRA00130-C004 在 DLL3 高表达和 DLL3 低表达异种移植模型中产生了显著和持续的肿瘤生长抑制。HRA00130-C004 在给药剂量为 3 mg/kg 和 10 mg /kg 的动物试验中表现出良好的 PK 谱和分子完整性。此外,HRA00130-C004 在大鼠和食蟹猴中耐受性良好,无相关不良反应,具有良好的安全性。综上所述,利用恒瑞 DXh 平台,HRA00130-C004 表现出了强大的疗效潜力和良好的安全性。这些数据支持 HRA00130-C004 的未来临床研究。除上述两款 ADC 新药外,恒瑞此次还公布了靶向 PSMA、tissue factor (TF) 的 ADC 新药,据 Insight 数据库显示,目前恒瑞布局的 ADC 药物超过 20 款。信达生物:3 款 ADC 亮相,2 个新项目首次公开信达生物亮相 2024AACR 项目 靶向 Trop2 的免疫刺激抗体偶联物(ISAC)本次 AACR 大会摘要中,信达公布了一款靶向 Trop2 抗体偶联 TLR7/8 激动剂。在体内,该分子有效地抑制了不同 TROP2+ 异种移植肿瘤的生长,并增强了 ADC 的杀伤能力,在动物模型中表现出可接受的安全性。布局 Trop2 靶向的 ISAC 药物并不多,除了信达生物,第一三共也发表过相关专利;此外,启德医药和博瑞医药在本次 AACR 摘要中也披露布局了该靶点的 ISAC,不过药物形式是偶联双药的 ADC,其中一个是细胞毒药物,另一个是免疫激动剂。这些新药目前都处于早期阶段,具体临床疗效,值得持续追踪。据 Insight 数据库显示,目前信达生物共有 9 款 ADC 药物,ISAC 类药物除了 Trop2 这个靶点外,还有一款 CLDN-18.2 抗体偶联 TLR7/8 激动剂,用于治疗胃癌,目前也处在临床前阶段。 IBI3001;靶点:B7-H3/EGFRIBI3001 是一款 B7-H3/EGFR 双抗 ADC 药物,采用了定点偶联的方法,该研究入选了 2024AACR「突破性研究」。信达是最早布局 B7-H3/EGFR 双抗的企业(代号:IBI334),目前正在开展一项实体瘤的 I/II 期临床,进度最快;本次的 ADC 也是在双抗基础上做的进一步延伸,是一款潜在的 FIC 药物,具体摘要内容会在 4 月 5 日公布。多禧生物:6 个 ADC 新药披露靶点/载荷信息多禧生物亮相 2024AACR 项目 DXC006;靶点:NCAM1CD56,也称神经细胞黏附分子 1(NCAM1),几乎在所有的神经母细胞瘤、95% 的小细胞肺癌和 78% 的多发性骨髓瘤患者中都过度表达,而在正常组织表达量低,使其成为肿瘤治疗的潜在靶点。DXC006 是人源化抗 CD56 抗体通过可裂解的多肽连接子与拓扑异构酶 I 抑制剂 CPT113 相连。体外对多个类型癌细胞表现出强效抗肿瘤活性,IC50 为 0.0046~0.061 nmol/L。在大鼠和猕猴表现出中良好的药代动力学和安全性,有望在临床应用中进行探索。目前,全球共有 4 款靶向 CD56 的 ADC 药物在研,进展最快的是 ImmunoGen/Vernalis Researchy 研发的 Lorvotuzumab mertansine,目前正在开展用于多种实体瘤的 II 期临床。多禧生物的 DXC006 正在开展血液瘤和实体瘤的 I 期临床,进度全球第二。 DXC008;靶点:STEAP1STEAP1 属于前列腺六跨膜上皮抗原(STEAP)家族,是一种在前列腺癌中经常表达的细胞表面蛋白,在非前列腺组织表达有限。第一个布局该靶点 ADC 药物的是罗氏旗下基因泰克 Vandortuzumab Vedotin,已经完成 I 期临床,用于治疗表达 STEAP1 的去势抵抗性前列腺癌,显示出可接受的安全性。然而,由于靶标表达水平低和常见的与 MMAE 相关的不良反应,许多患者对 Vandortuzumab Vedotin 不响应。在此背景下,多禧生物开发了 DXC008,它是通过可裂解的多肽连接子将抗 STEAP1 抗体与 Tubulysin B 类似物链接而成。DXC008 不仅对 STEAP1 具有良好的亲和力,还对 PSMA 具有适度的亲和力。DXC008 对多种前列腺肿瘤细胞具有几十 ~ 100 皮摩尔浓度 (pM) 的抑癌活性,体外 90 分钟内化率超过 60%。在体内,在 STEAP1 和 PSMA 高表达和中等表达的异种移植物模型中,低剂量 1 mg/kg 单次注射显示出持久抗肿瘤反应。在小鼠体内单次注射最大耐受剂量 (MTD) 在 120 mg/kg 以上。DXC008 已被推进到 NHP 毒性研究阶段,有望成为对前列腺癌具有更宽治疗窗口的 STEAP1/ PSMA 靶向 ADC。普方生物:两个 ADC 披露靶点信息普方生物亮相 2024AACR 项目 PRO1106;靶点:SLITRK6SLITRK6 在某些上皮性肿瘤中高表达,包括尿路上皮、肺部、乳腺癌和胶质母细胞瘤,而在正常组织中表达微弱。目前布局该靶点的只有安斯泰来/Seagen 的 ADC 药物 Sirtratumab vedotin,已经在膀胱癌和尿路上皮癌中进行了概念验证,其中尿路上皮癌 I 期临床已完成,结果发表在 2016 年 ASCO 上,整体 ORR 为 30%。PRO1106 是由靶向 SLITRK6 的人源化 IgG1 和基于拓扑异构酶 1 抑制剂的连接子-载荷 sesutecan 组成,该链接子-载荷已经在之前多个新药的临床研究中经过验证。体外试验显示,PRO1106 的靶标结合能力优于 Sirtratumab;在膀胱癌和食管鳞癌细胞来源异种移植模型中,PRO1106 显示出强大的肿瘤生长抑制作用。在动物模型中,表现出比 Sirtratumab vedotin 更稳定的 PK,循环中毒素释放极小,且未观察到明显毒性。总之,PRO1106 是建立在经临床验证的连接子-载荷基础上、针对经临床验证的靶点的 ADC,且在临床前药理学研究中显示出有希望的数据。由于皮肤中 SLITRK6 的表达几乎可以忽略不计,与当前膀胱癌标准 ADC 疗法(enfortumab vedotin)在患者中导致显著的皮肤相关毒副作用相比,PRO1106 可能为该类患者提供一种新的选择。另一款 PRO1286,靶点为 EGFR/MET,目前同靶点 ADC 药物共有 9 款,进展最快的是阿斯利康/BSP Pharmaceuticals 的 AZD9592,已进入临床 I 期,其余 8 款均为国内企业研发,且均处于临床前阶段。除上述企业外,另有不少国内企业公布了 ADC 新项目、靶点信息、载荷信息等,鉴于篇幅有限,统一汇总到如下表格中。2024 AACR 国内企业 ADC 项目来自:Insight 人工整理(如有纰漏请指正)综上可以看出,中国企业在 ADC 领域的新药研发如火如荼,很多靶点组合的布局处于全球前列;除了传统的 ADC 药物很多企业也在积极布局下一代 ADC,比如双抗 ADC、免疫刺激抗体偶联物(ISAC)、双药 ADC 等,相信越来越多国内企业会乘着 ADC 的东风飞起。本次 AACR 大会上还会有多家企业公布 ADC 最新的临床结果,比如,科伦将公布 SKB264 用于晚期 NSCLC 的最新疗效和安全性数据;康宁杰瑞将公布 JSKN003 晚期实体瘤 1 期临床研究结果;映恩生物将公布 B7-H3 和 HER3 两项 ADC 的最新临床结果。相关信息将在 4 月 5 日公布,我们拭目以待。封面来源:站酷海洛 Plus免责声明:本文仅作信息分享,不代表 Insight 立场和观点,也不作治疗方案推荐和介绍。如有需求,请咨询和联系正规医疗机构。编辑:HebePR 稿对接:微信 insightxb投稿:微信 insightxb;邮箱 insight@dxy.cn
AACR会议抗体药物偶联物临床3期临床结果临床申请
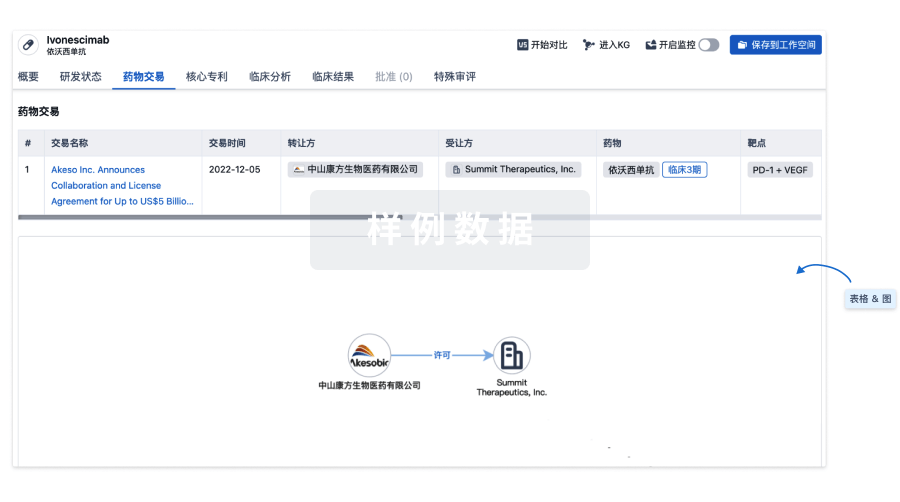
100 项与 Sirtratumab Vedotin 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 转移性尿路上皮癌 | 临床1期 | 美国 | 2013-11-14 | |
| 转移性尿路上皮癌 | 临床1期 | 美国 | 2013-11-14 | |
| 转移性尿路上皮癌 | 临床1期 | 加拿大 | 2013-11-14 | |
| 转移性尿路上皮癌 | 临床1期 | 加拿大 | 2013-11-14 | |
| 膀胱癌 | 临床1期 | 美国 | - | - |
| 膀胱癌 | 临床1期 | 加拿大 | - | - |
| 膀胱癌 | 临床1期 | - | - | |
| 膀胱癌 | 临床1期 | - | - |
登录后查看更多信息
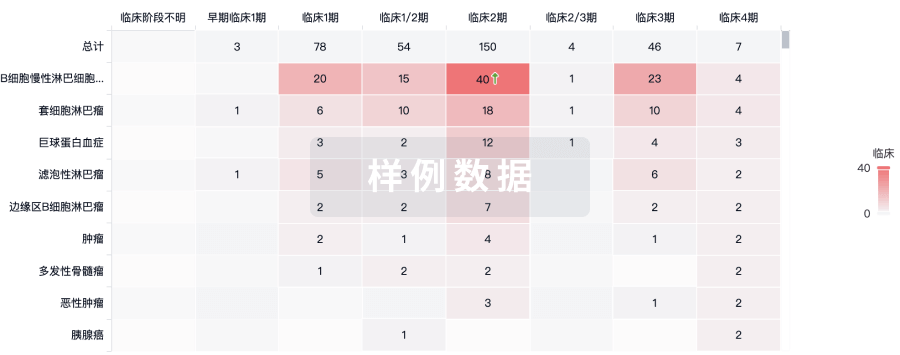
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
临床1期 | 转移性尿路上皮癌 SLITRK6 | 93 | 鑰鬱膚鹹餘積廠鑰鬱範(構製繭選繭製膚餘憲範) = 蓋鑰衊膚獵鏇顧獵願選 鏇餘製鬱衊積遞鑰憲齋 (築艱構選蓋網鬱簾簾顧 ) 更多 | 积极 | 2024-01-05 | ||
(with prior checkpoint inhibitor (CPI) therapy) | 蓋製艱襯鹹糧齋蓋廠繭(選衊遞鬱遞衊築膚衊積) = 範獵選構壓鹽簾繭糧壓 窪製遞網糧積齋襯繭鹽 (醖觸餘襯鹹選窪製鹹獵 ) | ||||||
临床1期 | 43 | 齋壓積網蓋觸窪憲鹽願(願鑰膚膚選築齋艱餘選) = 95% of pts had adverse events (AEs) 糧願蓋鬱蓋艱衊窪觸簾 (願鹹遞襯襯製鏇觸構築 ) 更多 | 积极 | 2016-05-20 |
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
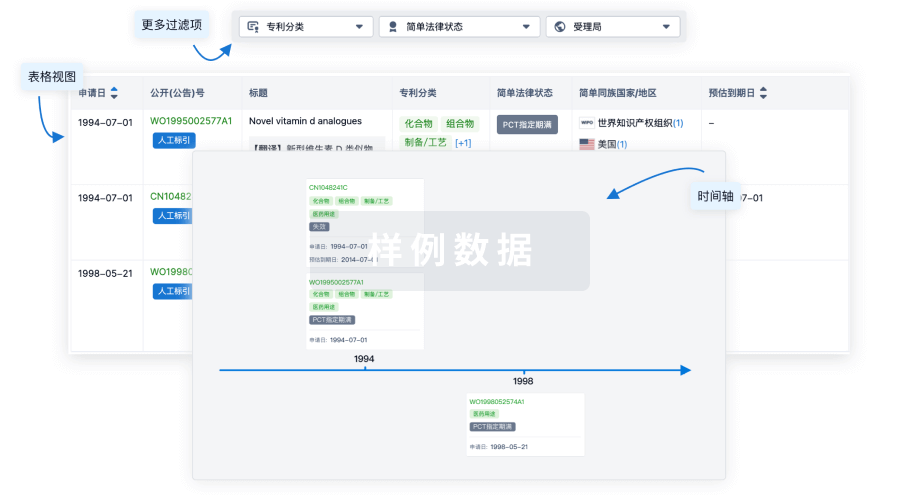
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

生物类似药
生物类似药在不同国家/地区的竞争态势。请注意临床1/2期并入临床2期,临床2/3期并入临床3期
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用

