预约演示
更新于:2025-07-05
KL-50
更新于:2025-07-05
概要
基本信息
在研机构 |
非在研机构- |
权益机构- |
最高研发阶段临床前 |
首次获批日期- |
最高研发阶段(中国)- |
特殊审评- |
结构/序列
分子式C7H7FN6O2 |
InChIKeyRXJOSBAVDXNQEY-UHFFFAOYSA-N |
CAS号1161826-19-2 |
关联
100 项与 KL-50 相关的临床结果
登录后查看更多信息
100 项与 KL-50 相关的转化医学
登录后查看更多信息
100 项与 KL-50 相关的专利(医药)
登录后查看更多信息
5
项与 KL-50 相关的文献(医药)2025-03-07·NEURO-ONCOLOGY
KL-50: A novel therapeutic agent targeting MGMT-deficient glioblastoma
Communications
作者: Zhang, Kenan ; Khasraw, Mustafa ; Touat, Mehdi
2025-03-07·NEURO-ONCOLOGY
The novel DNA cross-linking agent KL-50 is active against patient-derived models of new and recurrent post-temozolomide mismatch repair-deficient glioblastoma
Article
作者: Sears, Thomas ; Ruggeri, Bruce ; Chaliparambil, Rahul ; An, Shejuan ; Horbinski, Craig ; Wang, Wenxia ; McCord, Matthew ; James, C David ; Gueble, Susan ; Sarkaria, Jann ; Bindra, Ranjit
Abstract:
Background:
Acquired resistance to temozolomide (TMZ) chemotherapy due to DNA mismatch repair (MMR) enzyme deficiency is a barrier to improving outcomes for isocitrate dehydrogenase (IDH) wild-type glioblastoma (GBM) patients. KL-50 is a new imidazotetrazine-based therapeutic designed to induce DNA interstrand cross-links, and subsequent double-stranded breaks, in an MMR-independent manner in cells with O-6-methylguanine-DNA methyltransferase (MGMT) deficiency. Previous research showed its efficacy against LN229 glioma cells with MMR and MGMT knockdown. Its activity against patient-derived GBM that model post-TMZ recurrent tumors is unclear.
Methods:
We created MMR-deficient GBM patient-derived xenografts through exposure to TMZ, followed by treatment with additional TMZ or KL-50. We also generated isogenic, MSH6 knockout (KO) patient-derived GBM and tested them for sensitivity to TMZ and KL-50.
Results:
KL-50 extended the median survival of mice intracranially engrafted with either patient-derived TMZ-naïve GBM6 or TMZ-naïve GBM12 by 1.75-fold and 2.15-fold, respectively (P < 0.0001). A low dose (4 Gy) of fractionated RT further extended the survival of KL-50-treated GBM12 mice (median survival = 80 days for RT + KL-50 vs. 71 days KL-50 alone, P = 0.018). KL-50 also extended the median survival of mice engrafted with post-TMZ, MMR-deficient GBM6R-m185 (140 days for KL-50 vs. 37 days for vehicle, P < 0.0001). MSH6 KO increased TMZ IC50 for GBM6 and GBM12 cultures by >5-fold and >12-fold for cell death and live cell count outputs, respectively. In contrast, MSH6-KO actually decreased KL-50 IC50 by 10–80%.
Conclusion:
KL-50-based compounds are a promising new strategy for the treatment of MGMT-deficient, MMR-deficient GBM that recurs after frontline TMZ.
2024-07-10·Journal of the American Chemical Society
Mechanism of Action of KL-50, a Candidate Imidazotetrazine for the Treatment of Drug-Resistant Brain Cancers
Article
作者: Huseman, Eric D. ; Rees, Matthew G. ; Pyle, Anna M. ; Batista, Victor S. ; Fedorova, Olga ; Gueble, Susan E. ; Lin, Kingson ; Menges, Fabian ; Lo, Anna ; Roth, Jennifer A. ; Sundaram, Ranjini K. ; Crawford, Jason M. ; Oh, Joonseok ; Liu, Jinchan ; Herzon, Seth B. ; Ronan, Melissa M. ; Bindra, Ranjit S. ; Elia, James L.
Aberrant DNA repair is a hallmark of cancer, and many tumors display reduced DNA repair capacities that sensitize them to genotoxins. Here, we demonstrate that the differential DNA repair capacities of healthy and transformed tissue may be exploited to obtain highly selective chemotherapies. We show that the novel N3-(2-fluoroethyl)imidazotetrazine "KL-50" is a selective toxin toward tumors that lack the DNA repair protein O6-methylguanine-DNA-methyltransferase (MGMT), which reverses the formation of O6-alkylguanine lesions. We establish that KL-50 generates DNA interstrand cross-links (ICLs) by a multistep process comprising DNA alkylation to generate an O6-(2-fluoroethyl)guanine (O6FEtG) lesion, slow unimolecular displacement of fluoride to form an N1,O6-ethanoguanine (N1,O6EtG) intermediate, and ring-opening by the adjacent cytidine. The slow rate of N1,O6EtG formation allows healthy cells expressing MGMT to reverse the initial O6FEtG lesion before it evolves to N1,O6EtG, thereby suppressing the formation of toxic DNA-MGMT cross-links and reducing the amount of DNA ICLs generated in healthy cells. In contrast, O6-(2-chloroethyl)guanine lesions produced by agents such as lomustine and the N3-(2-chloroethyl)imidazotetrazine mitozolomide rapidly evolve to N1,O6EtG, resulting in the formation of DNA-MGMT cross-links and DNA ICLs in healthy tissue. These studies suggest that careful consideration of the rates of chemical DNA modification and biochemical DNA repair may lead to the identification of other tumor-specific genotoxic agents.
3
项与 KL-50 相关的新闻(医药)2024-10-27
前言
AIDD Pro 根据国内外各大网站以及人工智能药物设计主流新闻网站及公众号,从 AIDD会议、AIDD招聘,重大科研进展、行业动态、最新报告发布等角度,分析挖掘了每周人工智能辅助药物设计领域所发生的、对领域技术发展产生重大推动作用的事件,旨在帮助 AIDD领域研究人员和业内人士及时追踪最新科研动态、洞察前沿热点。如果您觉得符合以上要求的内容我们有遗漏或者更好建议,欢迎后台留言。
科研进展2024年10月25日【靶点】Chem. Rev. | 不可及药物靶点大环肽核苷酸编码文库的选择2024年10月25日【蛋白质组学】J. Proteome Res. | 元蛋白质组学蛋白质序列数据库的构建:现有工具和数据库的综述2024年10月25日【SARS-CoV-2】J. Med. Chem. | 从DNA编码的化学文库筛选Hit中合理设计SARS-CoV-2 Mpro大环非共价抑制剂,显示对泛冠状病毒同源物和耐Nirmatrelvir变体的有效抑制2024年10月24日【药物发现】J. Med. Chem. | 小分子药物发现的计算方法现状2024年10月23日【高通量筛选】J. Chem. Inf. Model. | 优化高通量筛选管道的机器学习驱动数据评估2024年10月23日【机器学习】J. Med. Chem. | 通过化学空间互补DEL筛选策略增强机器学习模型的预测能力
具体信息,请滑动下方文字
1.【靶点】
医药领域的技术进步和突破性发展正以越来越强的坚持叩响着“坚不可摧”堡垒的大门。值得注意的是,21世纪出现了大环化合物,其中环肽特别令人感兴趣。这一类新的潜在候选药物占据了经典小分子药物和更大的基于蛋白质的治疗药物(如抗体)之间的巨大化学空间。随着研究朝着长期以来被认为无法达到的临床靶点发展,大环肽非常适合在后5规则制药领域应对这些挑战。促进他们的发现是一个高通量筛选方法的武器库,利用大量随机的基因编码化合物文库。这些技术得益于非天然成分的掺入,如非蛋白质氨基酸或稳定碳氢化合物主要成分。利用这些特征进行大环肽的战略性结构设计,有可能解决蛋白质-蛋白质相互作用等具有挑战性的目标,这些目标长期以来一直抵制研究工作。本文综述了大环肽的主要高通量发现技术的基本原理和最新进展,并重点介绍了它们在靶向不可药空间中的具体应用。一个特别的重点放在新的设计指导方针和原则的环化和结构稳定的环肽的发展和由此产生的成功的故事,实现了众所周知的难以接近的药物目标。
链接网址:https://pubs-acs-org.libproxy1.nus.edu.sg/doi/10.1021/acs.chemrev.4c00422
DOI:https://doi-org.libproxy1.nus.edu.sg/10.1021/acs.chemrev.4c00422
2.【蛋白质组学】
在元蛋白质组学研究中,构建一个既全面又不过大的参考蛋白序列数据库是肽鉴定步骤的关键。因此,精心策划的参考数据库和定制数据库构建工具的可用性对于提高元蛋白质组学分析的性能至关重要。在这篇综述中,我们首先通过简要介绍元蛋白质组学的历史背景,概述了典型的实验和生物信息学工作流程,强调了构建元蛋白质组学蛋白质序列数据库的关键步骤。然后,我们将深入研究当前可用于构建此类数据库的工具,重点介绍它们各自的方法、实用程序以及优点和局限性。接下来,我们检查现有的蛋白质序列数据库,详细说明它们在元蛋白质组学研究中的范围和相关性。然后,我们提供了构建元蛋白质组学蛋白质序列数据库的实用建议,以及该领域当前挑战的概述。最后,我们讨论了元蛋白质组学蛋白质序列数据库建设的预期进展、新趋势和未来方向。
链接网址:https://pubs-acs-org.libproxy1.nus.edu.sg/doi/10.1021/acs.jproteome.4c00665
DOI:https://doi-org.libproxy1.nus.edu.sg/10.1021/acs.jproteome.4c00665
3.【SARS-CoV-2】
最近的全球COVID-19大流行突出表明,治疗冠状病毒感染是一项未满足的医疗需求。主蛋白酶(Mpro)一直是开发SARS-CoV-2直接抗病毒药物的重要靶点。Nirmatrelvir作为共价Mpro抑制剂是第一个被批准的治疗方法。尽管已经报道了各种化学类别的Mpro抑制剂,但它们对耐尼马特瑞韦变异的活性通常较低,泛冠状病毒的潜力有限,在未来爆发时对人类健康构成重大风险。我们提出了一种新的方法,利用DNA编码的化学文库筛选来鉴定非共价Mpro抑制剂5,该抑制剂与Nirmatrelvir具有独特的结合模式。设计用于锁定活性构象的大环化策略导致内酯12具有显着提高的抗病毒活性。进一步优化产生了强效内酰胺26,它对耐尼马特利韦变异以及来自其他冠状病毒的一组病毒主要蛋白酶表现出卓越的效力。
链接网址:https://pubs-acs-org.libproxy1.nus.edu.sg/doi/10.1021/acs.jmedchem.4c02009
DOI:https://doi-org.libproxy1.nus.edu.sg/10.1021/acs.jmedchem.4c02009
4.【药物发现】
对于计算科学来说,2024年是激动人心的一年,“人工神经网络”获得了诺贝尔物理学奖,“蛋白质结构预测与设计”获得了诺贝尔化学奖。鉴于计算机辅助药物设计(CADD)和人工智能在药物发现(AIDD)中的快速发展,总结它们的现状和未来发展方向对《药物化学杂志》的读者来说是及时和相关的。这篇评论旨在强调这些领域之间的最新发展、主要挑战和潜在的协同作用,为文献和科学博客中正在进行的讨论做出贡献。
链接网址:https://pubs-acs-org.libproxy1.nus.edu.sg/doi/10.1021/acs.jmedchem.4c02462
DOI:https://doi-org.libproxy1.nus.edu.sg/10.1021/acs.jmedchem.4c02462
5.【高通量筛选】
在快速发展的药物发现领域,高通量筛选(HTS)是鉴定生物活性化合物的必要手段。本研究引入了一种新的数据评估应用,一种基于影响评估数据点重要性的概念,以增强药物发现管道。我们的方法改进了化合物库筛选的主动学习,鲁棒地识别HTS数据中的真阳性和假阳性,并在不平衡的HTS训练中识别重要的非活性样本,同时考虑到计算效率。我们证明了基于重要性的方法能够更有效地批量筛选,减少了对广泛HTS的需求。机器学习模型准确区分真正的生物活性和分析伪像,简化药物发现过程。此外,重要欠采样有助于HTS数据集平衡,在不遗漏关键非活动样本的情况下提高机器学习性能。这些进步可以显著提高药物开发的效率和准确性。
链接网址:https://pubs-acs-org.libproxy1.nus.edu.sg/doi/10.1021/acs.jcim.4c01547
DOI:https://doi-org.libproxy1.nus.edu.sg/10.1021/acs.jcim.4c01547
6.【机器学习】
DNA编码文库(DNA-encoded library, DEL)技术是一种有效的小分子药物发现方法,可实现针对靶蛋白的高通量筛选。虽然DEL筛选产生广泛的数据,但它可以揭示人类分析不容易识别的复杂模式。从DEL筛选的先导化合物通常具有较高的分子量,这给药物开发带来了挑战。本研究通过整合光交联筛选等替代技术来改进传统的DELs,以增强化学多样性。这些方法的结合提高了小分子识别模型的预测性能。使用这种方法,我们预测了BRD4和p300的活性小分子,实现了26.7%和35.7%的命中率。值得注意的是,与传统的DEL分子相比,所鉴定的化合物具有更小的分子量和更好的修饰潜力。这项研究证明了DEL和AI技术之间的协同作用,促进了药物的发现。
链接网址:https://pubs-acs-org.libproxy1.nus.edu.sg/doi/10.1021/acs.jmedchem.4c01416
DOI:https://doi-org.libproxy1.nus.edu.sg/10.1021/acs.jmedchem.4c01416
上下滚动查看更多
药企动态2024年10月26日【Iterum
Therapeutics】首款!FDA批准创新小分子药物上市2024年10月25日【先声药业】先声药业癌症新药CDH6 ADC申报临床2024年10月24日【百时美施贵宝】全球首创心肌肌球蛋白抑制剂迈凡妥®(玛伐凯泰胶囊)在国内上市2024年10月24日【宜联生物】宜联生物ADC癌症新药拟纳入突破性治疗品种2024年10月23日【默沙东】13亿美元!默沙东收购一家biotech2024年10月23日【首药控股】首药控股肺癌1类新药申报上市各动态具体信息,请滑动下方文字
1.【Iterum Therapeutics】
Iterum
Therapeutics今日宣布,美国FDA已批准其药品Orlynvah(sulopenem etzadroxil & probenecid)用于治疗由指定微生物(大肠杆菌、肺炎克雷伯菌或奇异变形杆菌)引起的无并发症尿路感染(uUTIs)成年女性,这类患者没有或几乎没有可替代口服抗菌治疗方案。根据新闻稿,Orlynvah是FDA批准的首个口服培南类抗生素,也是过去二十年中第二款获得FDA批准的uUTI治疗药物。
链接网址请戳我
2.【先声药业】
10月25日,CDE官网显示,先声药业旗下先祥医药申报的1类新药—注射用SIM0505的临床试验申请获得NMPA受理。据其官网,SIM0505为一款 CDH6 ADC,是先声药业申报的首款ADC新药,也是第2款国产CDH6 ADC。
链接网址请戳我
3.【百时美施贵宝】
10月24日,百时美施贵宝宣布,继获得中国国家药品监督管理局(NMPA)优先审评批准后,创新治疗药物迈凡妥®(通用名:玛伐凯泰胶囊)现已在国内上市,用于治疗纽约心脏协会(NYHA)心功能分级II-III级的梗阻性肥厚型心肌病(HCM)成人患者,以改善运动能力和症状。这是全球首创,也是目前唯一获批用于治疗梗阻性肥厚型心肌病的心肌肌球蛋白抑制剂。
链接网址请戳我
4.【宜联生物】
10月24日,中国国家药监局药品审评中心(CDE)官网最新公示,宜联生物注射用YL201拟纳入突破性治疗品种,拟定适应症为经初始含铂治疗失败的复发性小细胞肺癌。YL201是宜联生物研发的一款靶向B7-H3的抗体偶联药物(ADC)。
链接网址请戳我
5.【默沙东】
10月23日,默沙东表示,公司已斥资高达13亿美元收购Modifi Biosciences,获得其实验性癌症疗法的使用权。作为交易的一部分,Modifi有资格获得高达13亿美元的潜在里程碑付款,默沙东预付了3000万美元,以获得一类新的治疗方法KL-50——正在开发用于治疗难以治疗的脑肿瘤,包括恶性胶质瘤。
链接网址请戳我
6.【首药控股】
今日(10月23日),中国国家药监局药品审评中心(CDE)官网公示,首药控股和双鹭药业共同申报的1类新药康太替尼颗粒上市申请获得受理。根据首药控股公告介绍,这是该公司自主研发的ALK抑制剂(研发代号:CT-707 ),本次申报上市的适应症为单药治疗间变性淋巴瘤激酶(ALK)阳性的局部晚期或转移性非小细胞肺癌(NSCLC)患者。
链接网址请戳我
上下滚动查看更多
会议信息
2024年11月15-16日 中关村科技园区大兴生物医药基地管理委员会举办首届中国药谷 · 未来生物创新药论坛
2025年1月9-10日 举办ICGT第八届细胞与基因治疗深度聚焦峰会
各会议具体详情和参会方式,请滑动下方文字
首届中国药谷 · 未来生物创新药论坛
主办方:中关村科技园区大兴生物医药基地管理委员会
会议时间:2024年11月15-16日
会议地点:北京
会议主旨:本论坛汇聚行业专家及优秀企业家代表,共同探讨行业前沿趋势,促进医药健康产业发展要素深度融合,进一步提升大兴区在创新药领域的影响力。将全球首创的科技成果写在大兴的土地上!让大兴成为全球首创药落地首选地!
链接网址请戳我
ICGT第八届细胞与基因治疗深度聚焦峰会
会议时间:2025年1月9-10日
会议地点:上海
会议主旨:共同探讨CGT产业链上中下游的关键环节,覆盖细胞免疫、眼科、罕见病和CMC热点议题,直面行业痛点,破解发展难点,共迎CGT产业的黄金十年。
链接网址请戳我
上下滚动查看更多
版权信息
本文内容均由小编收集于公开的各个网络平台,发布的目的仅为了方便大家一站式了解AIDD行业信息,并未对发布源头进行真实性验证。如您发现相关信息有任何版权侵扰或者信息错误,请及时联系AIDD Pro(请添加微信号sixiali_fox59)进行删改处理。
原创内容未经授权,禁止转载至其他平台。有问题可发邮件至sixiali@stonewise.cn
关注我,更多资讯早知道↓↓↓
临床研究
2024-10-24
·药研网
10月23日,默沙东表示,公司已斥资高达13亿美元收购Modifi Biosciences,获得其实验性癌症疗法的使用权。
作为交易的一部分,Modifi有资格获得高达13亿美元的潜在里程碑付款,默沙东预付了3000万美元,以获得一类新的治疗方法KL-50——正在开发用于治疗难以治疗的脑肿瘤,包括恶性胶质瘤。
Modifi Biosciences 联合创始人、耶鲁大学医学院治疗放射学教授、耶鲁大学脑肿瘤中心科学主任 Harvey 和 Kate Cushing 医学博士表示,在创立 Modifi Biosciences 时,我们试图从根本上改变胶质母细胞瘤和其他肿瘤癌症患者的肿瘤治疗模式,我们很荣幸默克认识到我们科学的潜力,作为一家肿瘤学公司,他们完全有能力通过临床试验和商业化来推进我们的创新。
Modifi Biosciences 的研究已通过学术创始人于 2022 年在《科学》杂志上发表的初步工作以及随后在许多肿瘤模型中令人信服的临床前数据得到验证,包括神经胶质瘤和其他具有内在 DNA 修复缺陷的癌症的患者来源异种移植模型。
默沙东研究实验室发现肿瘤学副总裁 David Weinstock 博士表示,DNA 修复缺陷是肿瘤细胞的常见标志,也是对癌症治疗产生耐药性的主要原因,优秀的 Modifi Biosciences 团队开发了一种创新方法,我们相信这种方法有可能治疗一些最难治的癌症类型。
Modifi Biosciences 成立于 2021 年是一家临床前阶段的公司,其开发的癌症疗法旨在通过修改癌症DNA来选择性地杀死癌细胞。迄今为止,Modifi已经筹集了1070万美元的种子资金,并得到了包括美国癌症协会投资部门BrightEdge在内的投资者的支持。
End
声明:本公众号所有发文章(包括原创及转载文章)系出于传递更多信息之目的,且注明来源和作者。本公众号欢迎分享朋友圈或大群,谢绝媒体或机构未经授权以任何形式转载至其他平台。
转载/商务/投稿 | 联系微信15618157102(sum_Gmi)
商务合作
稿件征集
点击了解详情
往期回顾
1
8月 | 高达22家药企裁员
2
国产首款四价HPV疫苗拟纳入优先审评
3
3. 7亿美元!今年规模最大的生物医药融资诞生
并购疫苗临床研究
2022-07-28
In 2005, Roger Stupp published an
article in
NEJM
, showing that adding temozolomide to radiotherapy extended brain cancer patients’ survival time by 2 months. For a cancer in which median survival was usually less than a year, that was practice-changing.
Temozolomide would be added to the first line of chemotherapies for glioma patients, and its use alongside radiation would be termed “The Stupp Protocol.”
However, a large number of patients were unresponsive to TMZ, and many who were responsive would go on to develop resistance to TMZ.
In a new study published in
Science
, Yale scientists describe an alternative drug to TMZ that may overcome that resistance problem. Led by Seth Herzon and Ranjit Bindra, they looked specifically at glioblastoma cells that are MGMT-deficient — a biomarker for cells that would respond better to TMZ initially, but develop resistance later on.
MGMT is a DNA repair protein. It works via a “suicide” mechanism, in which it takes away a methyl group from the damaged DNA, thereby fixing it, but inactivates itself as a result. On the other hand, once in the body, TMZ breaks down to become an alkylating agent, which means it adds alkyl groups (of which the simplest is a methyl group) to the DNA, thereby damaging the DNA.
(Last year, scientists discovered that TMZ, once thought to be exceedingly stable, is also
highly explosive
, apparently. It’s tentatively classified as a Class 1 explosive, putting it in the same zone as dynamite.)
In healthy cells where MGMT works as it should, after TMZ is added, the cells’ DNA repair systems readily correct the DNA lesions. But in MGMT-deficient tumors, those lesions build up, which triggers the cell’s mismatch repair system. The MMR system recognizes the DNA is damaged, and causes the tumor cells to die.
However, the problem is that eventually mutations pop up in the MMR pathway itself, and the tumor recurs.
So Herzon and Bindra conceived an approach that would, like TMZ, damage the DNA in glioma cells, but do away with the resistance once mutations happen in the MMR pathway. In their paper, they describe one candidate, KL-50, which is what’s known as an interstrand crosslinking (ICL) agent. Essentially, it slowly creates a link between the two strands of DNA — slow enough that healthy cells can reverse it. But in cancer cells, the link proves to be toxic and causes the cell to die.
Herzon noted that ICL agents “in and of itself [are] not a novel finding — those types of molecules are well known in the literature, and have been used unsuccessfully for decades in the clinic. What’s unique about our compound is that it is, in essence, a cell lines-specific crosslinking agent, so it only forms these interstrand crosslinks in an MGMT-deficient background.”
But to healthy cells, “the molecule is essentially invisible,” Herzon said.
In addition, by using the ICL mechanism, the drug isn’t dependent on the cell’s MMR system.
“We designed it in a way so that it would be impervious to resistance mutations that are common with glioma. One of those is mutations in mismatch repair. With temozolomide, mismatch repair mutations render the drug completely inactive,” Bindra said. “But we specifically made these DNA modifiers in a way that they’re impervious to that mutation. But they’re still dependent on the loss of MGMT, so they still have that therapeutic index.”
“It’s really a new way to approach tumor cell resistance, and also again, to exploit the DNA repair defects,” Bindra said.
However, for gliomas, which have historically been difficult to treat, the jury remains out on whether such a drug will work. “The new treatment looks very good in preclinical studies, especially with regard to overcoming the most common mechanism of resistance to TMZ, but clinical trials will be required to determine whether it is better,” Roger Reddel of the University of Sydney told
Endpoints News
in an email.
“GBM is a difficult tumor for many reasons including the way it infiltrates surrounding brain tissue which means it is difficult to remove completely by surgery, and the extensive heterogeneity within individual tumors and between tumors of the same type. The new approach does not specifically address any of these issues, but has the potential advantage that it seeks to improve one of the few treatments that has proven effective,” Reddel, who wrote an accompanying editorial on the study in
Science
, noted.
Bindra and Herzon, along with co-author Kingson Lin, have spun their discovery into Modifi Bio, which they launched from stealth today.
“As a physician scientist [who has] dedicated my clinical career and the last 10 years treating adult and pediatric brain tumors, I think there’s a lot of room to move on biomarker-directed therapies, that have really been rigorously validated in vitro and in vivo to set them up for the greatest chance of success in the clinic,” Bindra, who directs Yale’s brain tumor center, said.
“We’ve seen so many failures — they say GBM is a graveyard for therapeutics, but I say, if you bring dead drugs to the graveyard, they’re not going to suddenly live,” Bindra said.
Their biotech, Modifi Bio, starts with $6.4 million in seed funding, which it says will support IND-enabling studies and enable it to build out the platform that discovered KL-50, which Bindra terms a ‘DNA modifier.’
Notably, Roger Stupp also sits on Modifi’s advisory board. Modifi, derived from the Spanish word ‘modificado’, hopes to be in Phase I trials by 2024, it said.
“The new approach is also noteworthy because the drug design principle it uses could be extended to other tumor types with different DNA repair deficiencies,” Reddel also noted.
Durham-based
Chimerix
is another biotech taking the biomarker-based approach to gliomas. It bought Oncoceutics last year, and is testing its candidate in recurrent gliomas with an H3 K27M mutation.
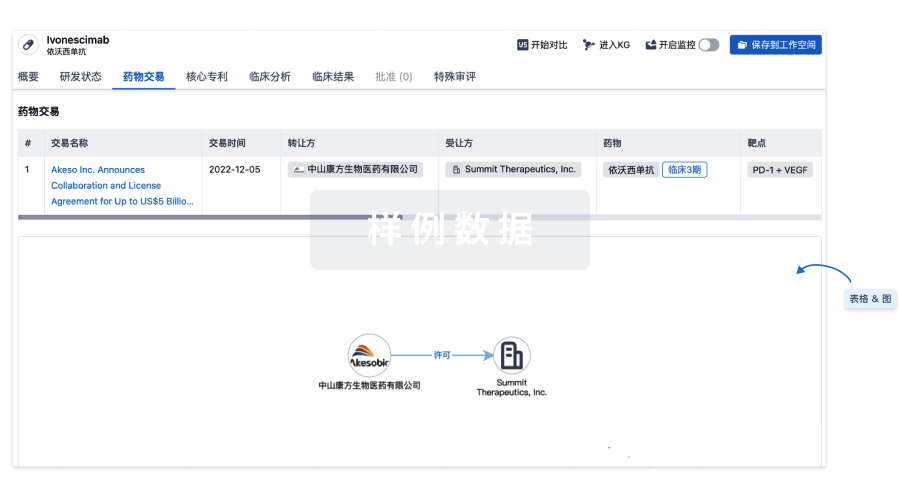
100 项与 KL-50 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 胶质母细胞瘤 | 临床前 | 美国 | 2023-04-17 |
登录后查看更多信息
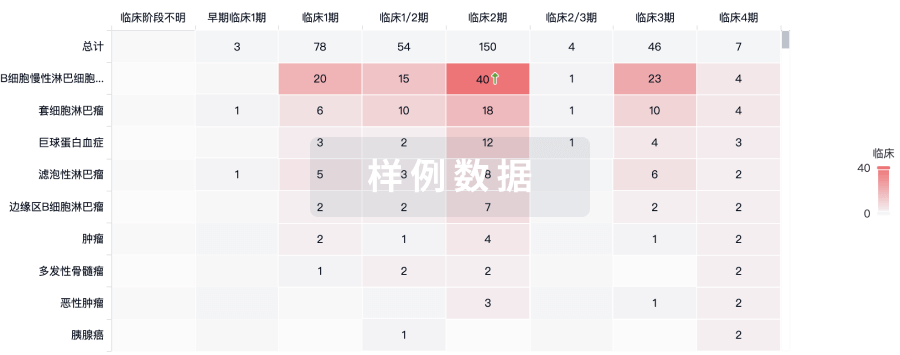
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
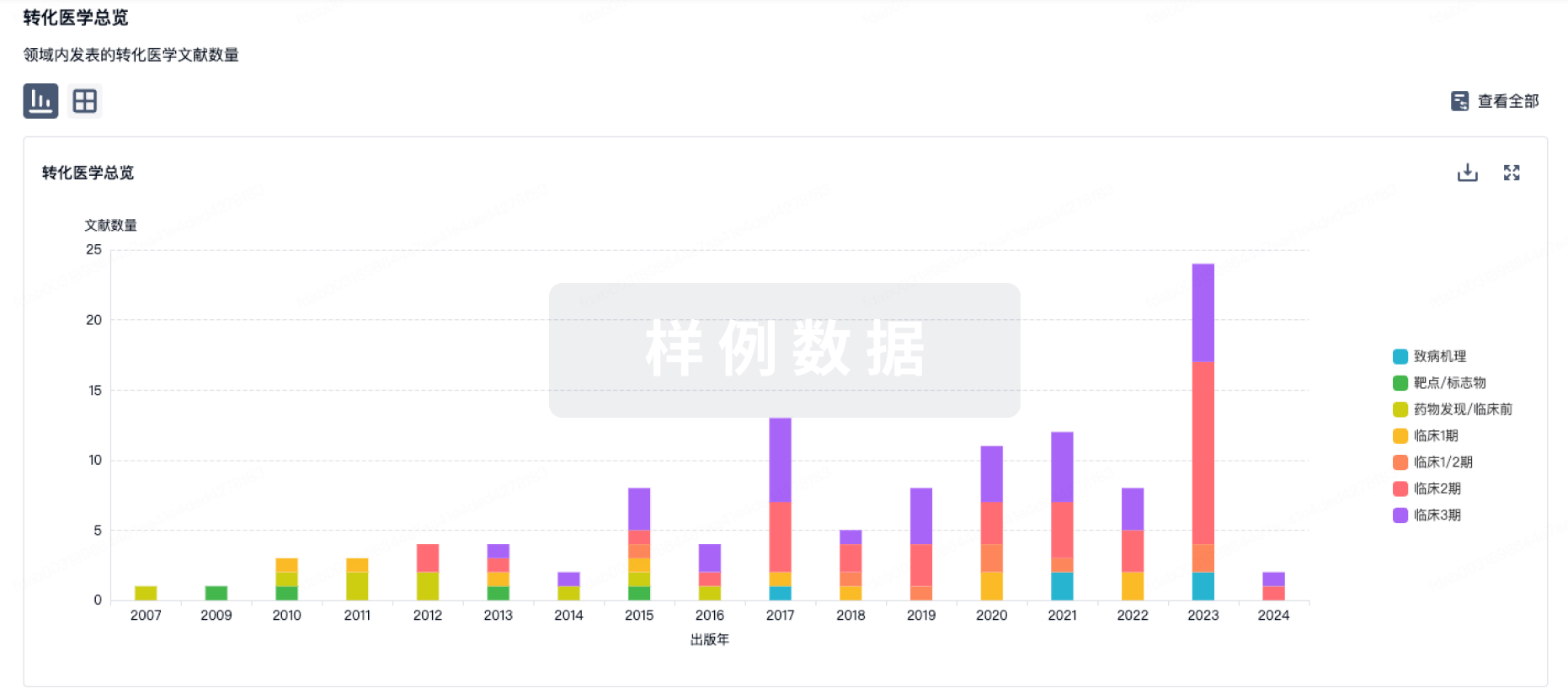
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
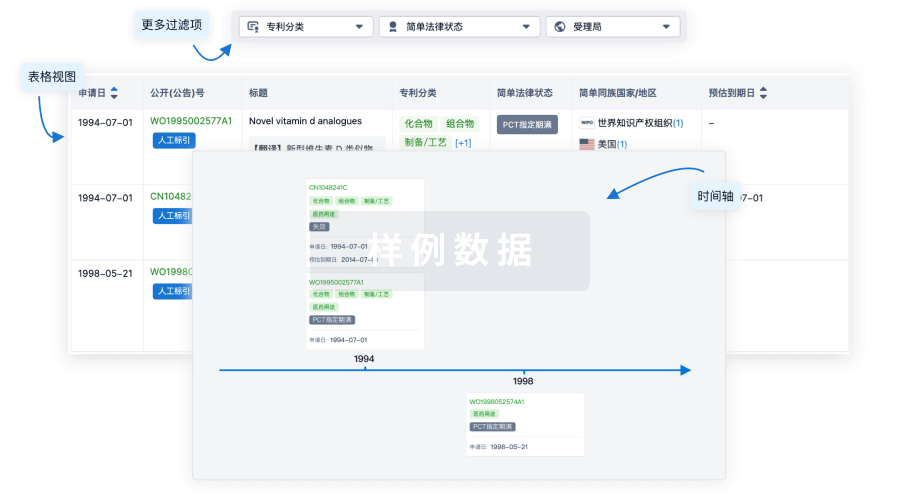
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用

