预约演示
更新于:2025-05-31
Mesothelin targeted CAR-T cells(Fapon Biotherapy)
更新于:2025-05-31
概要
基本信息
药物类型 CAR-T |
别名- |
作用方式 调节剂、抑制剂 |
作用机制 MSLN调节剂(间皮素调节剂)、PD-1抑制剂(细胞程序性死亡-1抑制剂)、免疫细胞毒性 |
在研适应症 |
非在研适应症- |
原研机构 |
在研机构 |
非在研机构- |
权益机构- |
最高研发阶段临床1期 |
首次获批日期- |
最高研发阶段(中国)临床1期 |
特殊审评- |
登录后查看时间轴
关联
1
项与 Mesothelin targeted CAR-T cells(Fapon Biotherapy) 相关的临床试验NCT05779917
Mesothelin/GPC3/GUCY2C Targeted CAR-T for Immunotherapy of Pancreatic Cancer: Phase I Clinical Trial
The second generation of mesothelin targeted CAR-T cells that secret a fusion protein of IL21 and scfv against PD1 have been constructed and their anti-cancer function has been verified by multiple in vitro and in vivo studies. Clinical studies will be performed to test anti-cancer function of the CAR-T cells for immunotherapy of human cancer patients with Mesothelin expressions. In this phase I study, the safety, tolerance, and preliminary efficacy of the Mesothelin-CAR-T cell immunotherapy on human cancers will firstly be evaluated.
开始日期2023-03-10 |
申办/合作机构  广州医科大学附属第二医院 广州医科大学附属第二医院 [+1] |
100 项与 Mesothelin targeted CAR-T cells(Fapon Biotherapy) 相关的临床结果
登录后查看更多信息
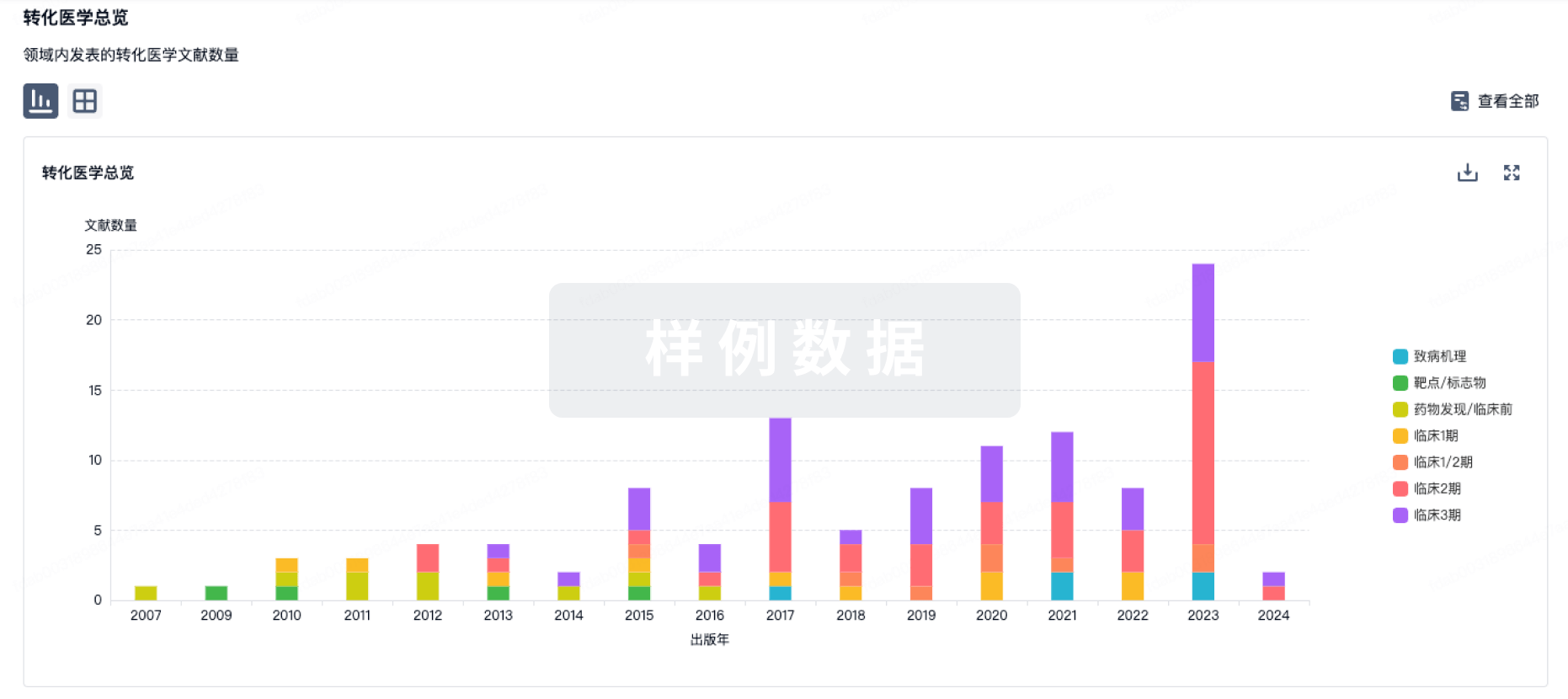
100 项与 Mesothelin targeted CAR-T cells(Fapon Biotherapy) 相关的转化医学
登录后查看更多信息
100 项与 Mesothelin targeted CAR-T cells(Fapon Biotherapy) 相关的专利(医药)
登录后查看更多信息
5
项与 Mesothelin targeted CAR-T cells(Fapon Biotherapy) 相关的文献(医药)2023-10-04·Cancer immunology research
Tumor-Targeted Nonablative Radiation Promotes Solid Tumor CAR T-cell Therapy Efficacy.
Article
作者: Bai, Yang ; Byun, Alexander J ; De Biasi, Andreas ; Quach, Hue Tu ; Mittal, Vivek ; Chintala, Navin K ; Skovgard, Matthew S ; Vista, William-Ray ; Amador-Molina, Alfredo ; Jones, David R ; Morello, Aurore ; Banerjee, Srijita ; Zeltsman, Masha ; Gomez, Daniel R ; Xiong, Yuquan ; Mayor, Marissa ; Bellis, Rebecca Y ; Saini, Jasmeen ; Rimner, Andreas ; Adusumilli, Prasad S ; Villena-Vargas, Jonathan
Infiltration of tumor by T cells is a prerequisite for successful immunotherapy of solid tumors. In this study, we investigate the influence of tumor-targeted radiation on chimeric antigen receptor (CAR) T-cell therapy tumor infiltration, accumulation, and efficacy in clinically relevant models of pleural mesothelioma and non-small cell lung cancers. We use a nonablative dose of tumor-targeted radiation prior to systemic administration of mesothelin-targeted CAR T cells to assess infiltration, proliferation, antitumor efficacy, and functional persistence of CAR T cells at primary and distant sites of tumor. A tumor-targeted, nonablative dose of radiation promotes early and high infiltration, proliferation, and functional persistence of CAR T cells. Tumor-targeted radiation promotes tumor-chemokine expression and chemokine-receptor expression in infiltrating T cells and results in a subpopulation of higher-intensity CAR-expressing T cells with high coexpression of chemokine receptors that further infiltrate distant sites of disease, enhancing CAR T-cell antitumor efficacy. Enhanced CAR T-cell efficacy is evident in models of both high-mesothelin-expressing mesothelioma and mixed-mesothelin-expressing lung cancer-two thoracic cancers for which radiotherapy is part of the standard of care. Our results strongly suggest that the use of tumor-targeted radiation prior to systemic administration of CAR T cells may substantially improve CAR T-cell therapy efficacy for solid tumors. Building on our observations, we describe a translational strategy of "sandwich" cell therapy for solid tumors that combines sequential metastatic site-targeted radiation and CAR T cells-a regional solution to overcome barriers to systemic delivery of CAR T cells.
2021-02-01·Human immunology4区 · 医学
PD-1 silencing improves anti-tumor activities of human mesothelin-targeted CAR T cells
4区 · 医学
Article
作者: Zhang, Linsong ; Yang, Mu ; Tian, Xiaoli ; Liu, Guodi ; Cui, Xingbing ; Li, Dehua ; Gu, Zhangjie ; Liu, Guoping ; Zhang, Qian ; Liu, Jibin ; Pan, Yingjiao ; Gu, Jinwei
Chimeric antigen receptor T (CAR T) cell therapy is a new pillar in cancer therapeutics, and has been successfully used for the treatment of cancers, including acute lymphoblastic leukemia and solid cancers. Following immune attack, many tumors upregulate inhibitory ligands which bind to inhibitory receptors on T cells. For example, the interaction between programmed cell death protein 1 (PD-1) on activated T cells and its ligands (widely known as PD-L1) on a target tumor limits the efficacy of CAR T cells therapy against poorly responding tumors. Here, we use mesothelin (MSLN)-expressing human ovarian cancer cells (SKOV3) and human colon cancer cells (HCT116) to investigate whether PD-1-mediated T cell exhaustion affects the anti-tumor activity of MSLN-targeted CAR T cells. We utilized cell-intrinsic PD-1-targeting shRNA overexpression strategy, resulting in a significant PD-1 silencing in CAR T cells. The reduction of PD-1 expression on T cell surface strongly augmented CAR T cell cytokine production and cytotoxicity towards PD-L1-expressing cancer cells in vitro. This study indicates the enhanced anti-tumor efficacy of PD-1-silencing MSLN-targeted CAR T cells against several cancers and suggests the potential of other specific gene silencing on the immune checkpoints to enhance the CAR T cell therapies against human tumors.
2019-05-08·Archives of medical science : AMS4区 · 医学
Mesothelin-targeted CAR-T cells for adoptive cell therapy of solid tumors
4区 · 医学
ArticleOA
作者: Zhang, Gui-Zhen ; Li, Tian-Fang ; Han, Shuang-Yin
Significant progresses have been made in adoptive cell therapy with CAR-T cells for cancers, especially for hematological malignancies. However, the treatment of solid tumors still poses a tremendous challenge and remains an unmet medical need. Several factors are held responsible for the inadequate responses: tumor heterogeneity, inefficient homing of T cells to tumor tissues, immunosuppressive microenvironment and the shortage of specific antigens shortage. Mesothelin is a cell-surface glycoprotein highly expressed in many types of solid tumors. As such, it has attracted much attention as a molecular target in cancer immunotherapy. Here, we delineate the barriers imposed by solid tumors on CARs, outline the rationale of mesothelin as a target for immunotherapy, summarize the preclinical and clinical results of mesothelin-targeted therapies, and extrapolate the expected results of CAR-T cells directed against mesothelin for solid tumors.
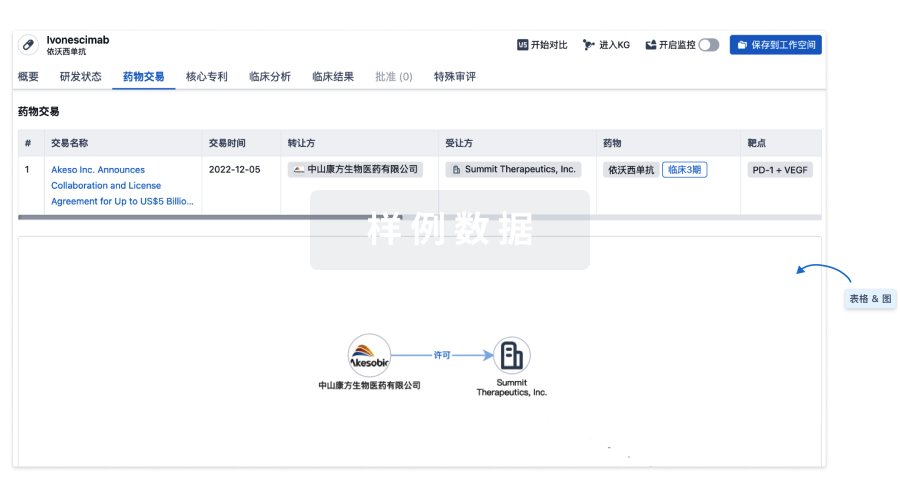
100 项与 Mesothelin targeted CAR-T cells(Fapon Biotherapy) 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 胰腺癌 | 临床1期 | 中国 | 2023-03-10 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
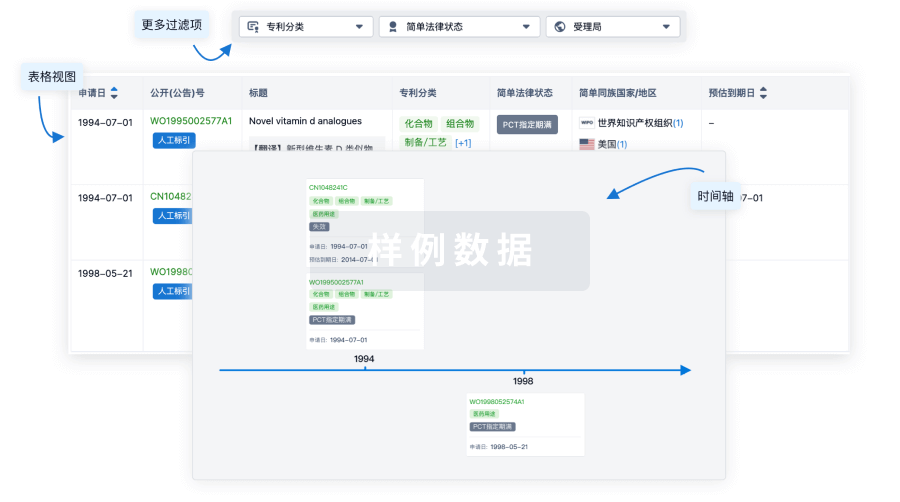
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或

批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用