预约演示
更新于:2025-10-25
Recombinant human thyrotropin(Suzhou Zelgen Biopharmaceuticals Co., Ltd.)
重组人促甲状腺激素 (苏州泽璟生物制药)
更新于:2025-10-25
概要
基本信息
原研机构 |
在研机构 |
非在研机构- |
最高研发阶段申请上市 |
首次获批日期- |
最高研发阶段(中国)申请上市 |
特殊审评- |
登录后查看时间轴
关联
4
项与 重组人促甲状腺激素 (苏州泽璟生物制药) 相关的临床试验NCT04964284
A Randomized, Open-label, Multi-center, Controlled Phase Ⅲ Study to Evaluate the Safety and Efficacy of Recombinant Human Thryoid Stimulating Hormone(rhTSH) for Adjuvant Radioiodine Ablation Therapy in Postoperative Patients With Differentiated Thyroid Cancer
This study was conducted in patients with differentiated thyroid cancer who had undergone total/near-total thyroidectomy. After surgery patients were randomized to one of two methods of performing thyroid remnant ablation. One group of patients who took thyroid hormone medicine and were euthyroid [i.e. their thyroid stimulating hormone (TSH) levels are normal], and received injections of rhTSH (0.9 mg daily on two consecutive days) followed by oral radioiodine. The second group of patients did not take thyroid hormone medicine so that they were hypothyroid (i.e. their TSH levels were high), and were given oral radioiodine.
开始日期2021-10-06 |
申办/合作机构 |
NCT04971473
An Open, Single-arm, Self-controlled, Multi-center Phase 3 Study to Compare the Efficacy and Safety of rhTSH as An Adjunctive Diagnostic Tool in Differentiated Thyroid Cancer Patients Who Had Been Thyroidectomized Vs. Patients Who After Thyroid Hormone Withdrawal
This is A non-blinded trial. Oral radioiodine was given 24 hours after the second injection of rhTSH, and scanning was done 48 hours after the radioiodine administration. Each patient was scanned first following rhTSH and then scanned after thyroid hormone withdrawal.
开始日期2021-09-10 |
申办/合作机构 |
NCT04447183
A Phase II Study of the Safety and Effectiveness of rhTSH in Radioiodine Treatment for Patients With Differentiated Thyroid Cancer.
This is a randomized, open, parallel controlled, multi-center clinical trial; 120 subjects were randomly assigned to the test group and the control group according to 3:1.
开始日期2020-11-23 |
申办/合作机构 |
100 项与 重组人促甲状腺激素 (苏州泽璟生物制药) 相关的临床结果
登录后查看更多信息
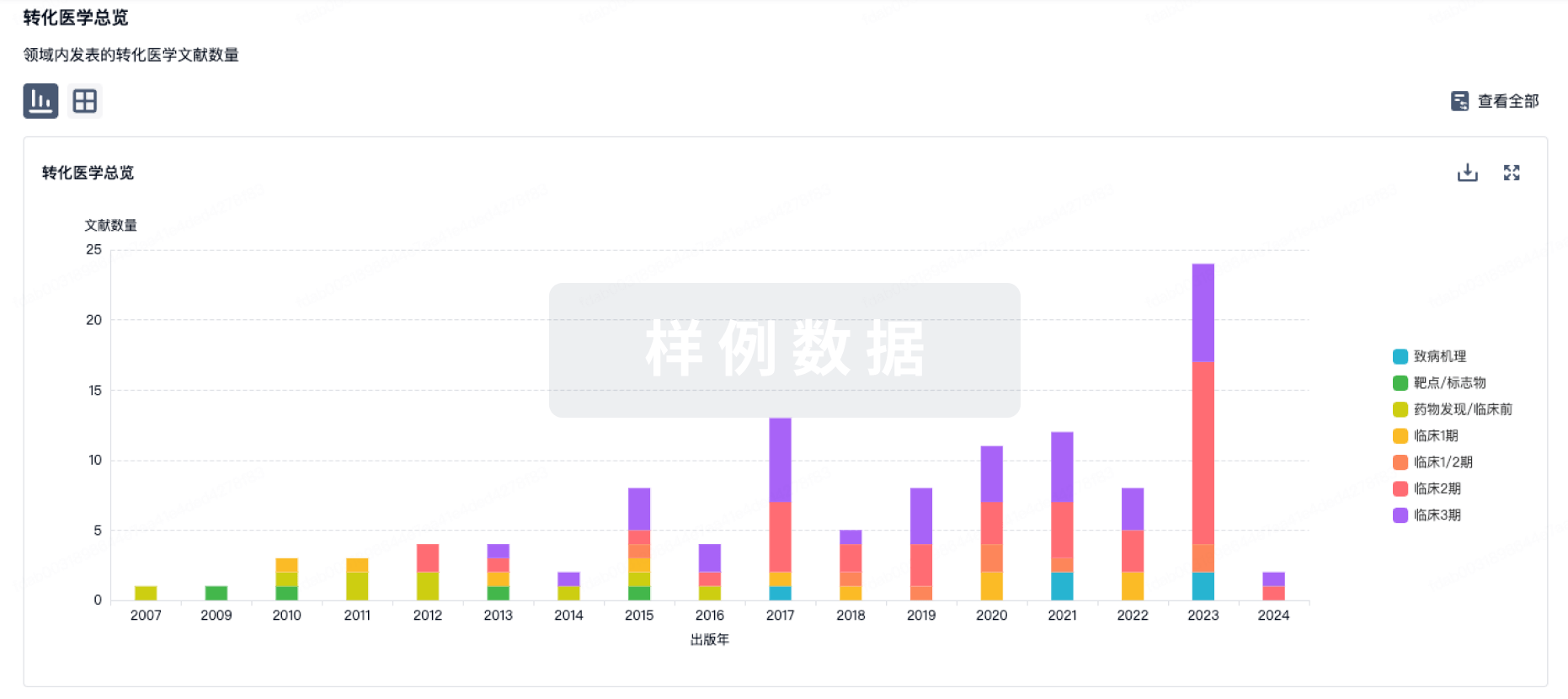
100 项与 重组人促甲状腺激素 (苏州泽璟生物制药) 相关的转化医学
登录后查看更多信息
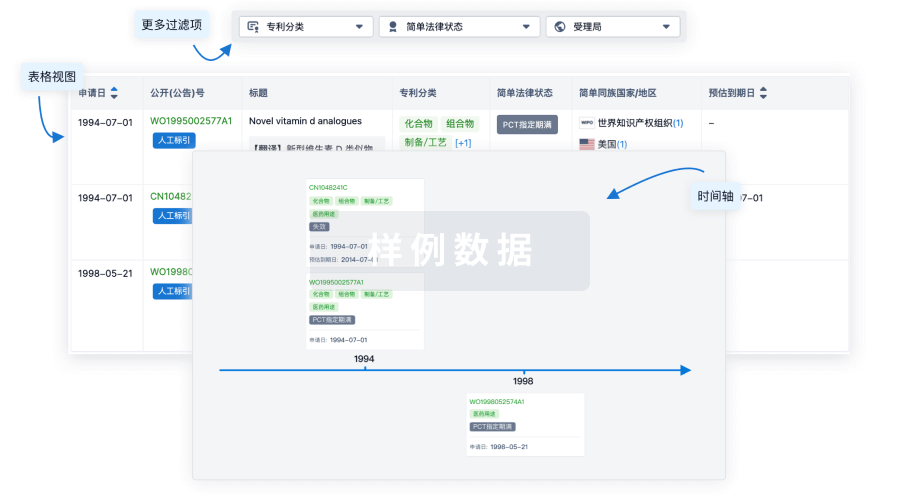
100 项与 重组人促甲状腺激素 (苏州泽璟生物制药) 相关的专利(医药)
登录后查看更多信息
76
项与 重组人促甲状腺激素 (苏州泽璟生物制药) 相关的文献(医药)2025-07-01·AACE Endocrinology and Diabetes
Use of Radioactive Iodine in Type 2 Amiodarone-Induced Thyrotoxicosis
Article
作者: Rodrigues, Sonia ; Yu, Run
Background/Objective:
Amiodarone-induced thyrotoxicosis (AIT) is a well-recognized etiology of hyperthyroidism. A case is reported here which demonstrates that radioactive iodine ablation therapy (RAI) can be used to treat type 2 AIT, even at lower radioactive iodine uptake (RAIU) levels than what conventional teaching would recommend for RAI.
Case Presentation:
An 80-year-old male with atrial fibrillation and cardiomyopathy was found to have type 2 AIT. He was refractory to other treatments for atrial fibrillation and therefore dependent on amiodarone. He was started on prednisone to treat AIT but developed fluid overload. As he was deemed a poor surgical candidate for thyroidectomy, recombinant human thyroid-stimulating hormone-stimulated RAI was administered with 29.5-mCi I-131; he subsequently developed subclinical hypothyroidism despite pre-RAI RAIU of 3%. He remained on amiodarone until he received a heart valve replacement, which temporarily relieved the atrial fibrillation and allowed for amiodarone discontinuation. After atrial fibrillation recurred and in anticipation of resuming amiodarone, he received a second dose of recombinant human thyroid-stimulating hormone-stimulated RAI at 26.5 mCi I-131, which rendered him clinically hypothyroid.
Discussion:
RAI therapy can be considered as a potential treatment strategy for type 2 AIT if the RAIU is at least 3%.
Conclusion:
This case demonstrates that RAI is an effective treatment strategy for type 2 AIT if the patient cannot tolerate steroids and is not a candidate for thyroidectomy. This case also illustrates how RAI can be used to prevent AIT.
2025-04-01·AMERICAN JOURNAL OF VETERINARY RESEARCH
Commercially available recombinant human thyroid-stimulating hormone effectively stimulates total and free thyroxine concentrations in Quaker parrots (Myopsitta monachus), including at low doses and after freezing
Article
作者: Thielen, Lauren E. ; Hoppes, Sharman ; Di Girolamo, Nicola
Abstract:
Objective:
To develop a protocol for thyroid-stimulating hormone (TSH) stimulation testing in psittacine birds using thyrotropin alfa (Thyrogen; Sanofi).
Methods:
Quaker parrots (Myopsitta monachus) were randomized to receive an IM injection of freshly reconstituted high-dose recombinant human TSH (rhTSH; 8 parrots), frozen high-dose rhTSH (8), frozen low-dose rhTSH (8), or saline (8). Total T4 (TT4), free T4 (FT4), T3, and TSH were measured pre- and 4 hours postinjection.
Results:
TSH stimulation testing was completed in 31 of the 32 birds. Thyroid-stimulating hormone measurement confirmed proper administration of rhTSH. Median TT4 at baseline in the population was 0.14 μg/dL (range, 0.03 to 0.33 µg/dL). Poststimulation, the median TT4 in rhTSH-treated parrots was 1.31 µg/dL (0.29 to 1.98 µg/dL) versus 0.09 µg/dL (0.04 to 0.14 µg/dL) in control parrots. All parrots administered rhTSH had an increase in TT4 (minimum, 3.5-fold) and FT4 (minimum, 2.2-fold) from baseline but not in T3. Parrots administered saline had no increase in TT4, FT4, or T3. Postinjection concentrations of TT4, but not of FT4 or T3, showed no overlap between controls and rhTSH-treated parrots.
Conclusions:
TSH stimulation testing performed with fresh and frozen rhTSH for 3 months is feasible and safe and results in a significant increase in TT4 in Quaker parrots. Total T4 should be the preferred outcome measure for TSH stimulation testing in parrots.
Clinical Relevance:
Thyrogen can be used at doses as low as 0.01 mL (73 µg/kg) for TSH stimulation tests in Quaker parrots and can be frozen in aliquots to perform more tests per vial.
2024-03-01·Clinical nuclear medicine
Comparison of Recombinant Human Thyroid-Stimulating Hormone and Thyroid Hormone Withdrawal for 131I Therapy in Patients With Intermediate- to High-Risk Thyroid Cancer
Review
作者: Bang, Ji-In ; Kim, Keunyoung ; Seo, Youngduk ; Choi, Miyoung ; Chong, Ari ; Hong, Chae Moon ; Park, Sohyun ; Oh, So Won ; Lee, Dong-Eun ; Lee, Sang-Woo
Background:
This meta-analysis and systematic review aimed to evaluate the therapeutic efficacy and advantages associated with the use of recombinant human thyroid-stimulating hormone (rhTSH) for radioactive iodine (RAI) therapy in patients with intermediate- to high-risk differentiated thyroid cancer.
Patients and Methods:
MEDLINE, EMBASE, and Cochrane databases were searched to identify relevant articles reporting clinical outcomes of rhTSH compared with thyroid hormone withdrawal (THW) in patients with intermediate- to high-risk differentiated thyroid cancer published between January 2012 and June 2023. Meta-analyses were performed (PROSPERO registration number: CRD42022340915) to assess the success rate of radioiodine remnant ablation (RRA) in patients with intermediate to high risk and determine the disease control rate among patients with distant metastases, evaluated using the RECIST criteria.
Results:
Thirteen studies involving 1858 patients were included in the meta-analysis. Pooled analyses revealed significantly higher overall RRA success rate in the rhTSH group compared with the THW group, with a risk ratio (RR) of 1.12 (95% confidence interval [CI], 1.01–1.25). However, in the subgroup analysis of high-risk patients, pooled analyses showed no significant differences in RRA success rate between the rhTSH group compared with the THW group with a pooled RR of 1.05 (95% CI, 0.88–1.24). In patients with distant metastases, there were no significant differences in the disease control rate between groups, with a pooled RR of 1.06 (95% CI, 0.78–1.44).
Conclusions:
rhTSH for RAI therapy is a practical option for RAI therapy in patients with intermediate- to high-risk thyroid cancer, including those with distant metastases.
32
项与 重组人促甲状腺激素 (苏州泽璟生物制药) 相关的新闻(医药)2025-10-24
·新浪看点
10月24日,泽璟制药涨1.54%,成交额1.83亿元,换手率0.69%,总市值269.47亿元。异动分析重组蛋白+创新药+细胞免疫治疗1、2022年12月20日互动易:公司目前已按照GMP标准建成重组蛋白药物生产车间及其配套设施,近期已经顺利通过了药监部门的生产现场核查,能满足重组人凝血酶商业化生产需要。同时,公司拟进一步扩建重组人凝血酶生产车间及相关配套设施,以进一步扩大产能,满足长期市场增长需求。2、公司正在开展 13 个主要创新药物的 39 项在研项目,其中甲苯磺酸多纳非尼片、外用重组人凝血酶、盐酸杰克替尼片和注射用重组人促甲状腺激素取得了重要的阶段性成果。其余产品处于研究开发的不同阶段。3、2023年6月9日公告,苏州泽璟生物制药股份有限公司(以下简称“公司”)在研产品注射用 ZGGS15 临床试验申请获得美国食品药品监督管理局(以下简称“FDA”)批准, 用于治疗晚期实体瘤。ZGGS15 是一个人源化抗淋巴细胞激活基因-3(LAG-3)和抗具有 Ig 和 ITIM 结构域的 T 细胞免疫受体(TIGIT)的双特异性抗体,为创新型肿瘤免疫治疗生物制品,注册分类为 1 类,有望用于治疗多种晚期实体瘤。(免责声明:分析内容来源于互联网,不构成投资建议,请投资者根据不同行情独立判断)资金分析今日主力净流入-173.53万,占比0.01%,行业排名72/158,连续2日被主力资金减仓;所属行业主力净流入-14.58亿,连续2日被主力资金减仓。区间今日近3日近5日近10日近20日主力净流入-173.53万-1844.76万-2092.50万-1.08亿-1.20亿主力持仓主力没有控盘,筹码分布非常分散,主力成交额7297.91万,占总成交额的6.48%。技术面:筹码平均交易成本为106.73元该股筹码平均交易成本为106.73元,近期该股获筹码青睐,且集中度渐增;目前股价在压力位109.00和支撑位96.77之间,可以做区间波段。公司简介资料显示,苏州泽璟生物制药股份有限公司位于江苏省昆山市玉山镇晨丰路262号,成立日期2009年3月18日,上市日期2020年1月23日,公司主营业务涉及化学新药及生物新药的研发、生产及销售。主营业务收入构成为:药品99.97%,医药中间体及原辅料0.02%,资产租赁0.00%。泽璟制药所属申万行业为:医药生物-化学制药-化学制剂。所属概念板块包括:抗癌治癌、抗癌药物、AI医药、生物医药、创新药等。截至6月30日,泽璟制药股东户数8795.00,较上期增加16.75%;人均流通股30097股,较上期减少14.35%。2025年1月-6月,泽璟制药实现营业收入3.76亿元,同比增长56.07%;归母净利润-7280.35万元,同比减少9.42%。机构持仓方面,截止2025年6月30日,泽璟制药十大流通股东中,中欧医疗健康混合A(003095)位居第五大流通股东,持股816.63万股,相比上期增加268.75万股。广发医疗保健股票A(004851)位居第六大流通股东,持股527.45万股,相比上期减少117.14万股。工银前沿医疗股票A(001717)位居第七大流通股东,持股470.00万股,相比上期减少30.53万股。汇添富创新医药混合A(006113)位居第八大流通股东,持股426.89万股,为新进股东。富国精准医疗灵活配置混合A(005176)位居第十大流通股东,持股342.45万股,为新进股东。广发多因子混合(002943)退出十大流通股东之列。风险提示:市场有风险,投资需谨慎。本文为AI大模型自动发布,任何在本文出现的信息(包括但不限于个股、评论、预测、图表、指标、理论、任何形式的表述等)均只作为参考,不构成个人投资建议。
免疫疗法
2025-10-22
·新浪看点
10月22日,泽璟制药跌1.31%,成交额3.12亿元,换手率1.10%,总市值274.77亿元。异动分析重组蛋白+创新药+细胞免疫治疗1、2022年12月20日互动易:公司目前已按照GMP标准建成重组蛋白药物生产车间及其配套设施,近期已经顺利通过了药监部门的生产现场核查,能满足重组人凝血酶商业化生产需要。同时,公司拟进一步扩建重组人凝血酶生产车间及相关配套设施,以进一步扩大产能,满足长期市场增长需求。2、公司正在开展 13 个主要创新药物的 39 项在研项目,其中甲苯磺酸多纳非尼片、外用重组人凝血酶、盐酸杰克替尼片和注射用重组人促甲状腺激素取得了重要的阶段性成果。其余产品处于研究开发的不同阶段。3、2023年6月9日公告,苏州泽璟生物制药股份有限公司(以下简称“公司”)在研产品注射用 ZGGS15 临床试验申请获得美国食品药品监督管理局(以下简称“FDA”)批准, 用于治疗晚期实体瘤。ZGGS15 是一个人源化抗淋巴细胞激活基因-3(LAG-3)和抗具有 Ig 和 ITIM 结构域的 T 细胞免疫受体(TIGIT)的双特异性抗体,为创新型肿瘤免疫治疗生物制品,注册分类为 1 类,有望用于治疗多种晚期实体瘤。(免责声明:分析内容来源于互联网,不构成投资建议,请投资者根据不同行情独立判断)资金分析今日主力净流入1024.88万,占比0.03%,行业排名27/158,连续2日被主力资金增仓;所属行业主力净流入2.59亿,当前无连续增减仓现象,主力趋势不明显。区间今日近3日近5日近10日近20日主力净流入1024.88万777.14万-788.90万-7283.30万-8641.04万主力持仓主力没有控盘,筹码分布非常分散,主力成交额8701.27万,占总成交额的6.78%。技术面:筹码平均交易成本为106.81元该股筹码平均交易成本为106.81元,近期该股快速吸筹,短线操作建议关注;目前股价靠近支撑位102.62,注意支撑位处反弹,若跌破支撑位则可能会开启一波下跌行情。公司简介资料显示,苏州泽璟生物制药股份有限公司位于江苏省昆山市玉山镇晨丰路262号,成立日期2009年3月18日,上市日期2020年1月23日,公司主营业务涉及化学新药及生物新药的研发、生产及销售。主营业务收入构成为:药品99.97%,医药中间体及原辅料0.02%,资产租赁0.00%。泽璟制药所属申万行业为:医药生物-化学制药-化学制剂。所属概念板块包括:抗癌治癌、抗癌药物、AI医药、生物医药、创新药等。截至6月30日,泽璟制药股东户数8795.00,较上期增加16.75%;人均流通股30097股,较上期减少14.35%。2025年1月-6月,泽璟制药实现营业收入3.76亿元,同比增长56.07%;归母净利润-7280.35万元,同比减少9.42%。机构持仓方面,截止2025年6月30日,泽璟制药十大流通股东中,中欧医疗健康混合A(003095)位居第五大流通股东,持股816.63万股,相比上期增加268.75万股。广发医疗保健股票A(004851)位居第六大流通股东,持股527.45万股,相比上期减少117.14万股。工银前沿医疗股票A(001717)位居第七大流通股东,持股470.00万股,相比上期减少30.53万股。汇添富创新医药混合A(006113)位居第八大流通股东,持股426.89万股,为新进股东。富国精准医疗灵活配置混合A(005176)位居第十大流通股东,持股342.45万股,为新进股东。广发多因子混合(002943)退出十大流通股东之列。风险提示:市场有风险,投资需谨慎。本文为AI大模型自动发布,任何在本文出现的信息(包括但不限于个股、评论、预测、图表、指标、理论、任何形式的表述等)均只作为参考,不构成个人投资建议。
免疫疗法IPO
2025-10-21
·新浪看点
10月21日,泽璟制药涨2.17%,成交额2.92亿元,换手率1.06%,总市值278.42亿元。异动分析重组蛋白+创新药+细胞免疫治疗1、2022年12月20日互动易:公司目前已按照GMP标准建成重组蛋白药物生产车间及其配套设施,近期已经顺利通过了药监部门的生产现场核查,能满足重组人凝血酶商业化生产需要。同时,公司拟进一步扩建重组人凝血酶生产车间及相关配套设施,以进一步扩大产能,满足长期市场增长需求。2、公司正在开展 13 个主要创新药物的 39 项在研项目,其中甲苯磺酸多纳非尼片、外用重组人凝血酶、盐酸杰克替尼片和注射用重组人促甲状腺激素取得了重要的阶段性成果。其余产品处于研究开发的不同阶段。3、2023年6月9日公告,苏州泽璟生物制药股份有限公司(以下简称“公司”)在研产品注射用 ZGGS15 临床试验申请获得美国食品药品监督管理局(以下简称“FDA”)批准, 用于治疗晚期实体瘤。ZGGS15 是一个人源化抗淋巴细胞激活基因-3(LAG-3)和抗具有 Ig 和 ITIM 结构域的 T 细胞免疫受体(TIGIT)的双特异性抗体,为创新型肿瘤免疫治疗生物制品,注册分类为 1 类,有望用于治疗多种晚期实体瘤。(免责声明:分析内容来源于互联网,不构成投资建议,请投资者根据不同行情独立判断)资金分析今日主力净流入28.67万,占比0%,行业排名60/158,该股当前无连续增减仓现象,主力趋势不明显;所属行业主力净流入-3.50亿,连续3日被主力资金减仓。区间今日近3日近5日近10日近20日主力净流入28.67万-3180.66万-1205.45万-7530.15万-1.60亿主力持仓主力没有控盘,筹码分布非常分散,主力成交额8348.21万,占总成交额的6.69%。技术面:筹码平均交易成本为106.81元该股筹码平均交易成本为106.81元,近期筹码减仓,但减仓程度减缓;目前股价靠近支撑位104.92,注意支撑位处反弹,若跌破支撑位则可能会开启一波下跌行情。公司简介资料显示,苏州泽璟生物制药股份有限公司位于江苏省昆山市玉山镇晨丰路262号,成立日期2009年3月18日,上市日期2020年1月23日,公司主营业务涉及化学新药及生物新药的研发、生产及销售。主营业务收入构成为:药品99.97%,医药中间体及原辅料0.02%,资产租赁0.00%。泽璟制药所属申万行业为:医药生物-化学制药-化学制剂。所属概念板块包括:抗癌治癌、抗癌药物、AI医药、生物医药、创新药等。截至6月30日,泽璟制药股东户数8795.00,较上期增加16.75%;人均流通股30097股,较上期减少14.35%。2025年1月-6月,泽璟制药实现营业收入3.76亿元,同比增长56.07%;归母净利润-7280.35万元,同比减少9.42%。机构持仓方面,截止2025年6月30日,泽璟制药十大流通股东中,中欧医疗健康混合A(003095)位居第五大流通股东,持股816.63万股,相比上期增加268.75万股。广发医疗保健股票A(004851)位居第六大流通股东,持股527.45万股,相比上期减少117.14万股。工银前沿医疗股票A(001717)位居第七大流通股东,持股470.00万股,相比上期减少30.53万股。汇添富创新医药混合A(006113)位居第八大流通股东,持股426.89万股,为新进股东。富国精准医疗灵活配置混合A(005176)位居第十大流通股东,持股342.45万股,为新进股东。广发多因子混合(002943)退出十大流通股东之列。风险提示:市场有风险,投资需谨慎。本文为AI大模型自动发布,任何在本文出现的信息(包括但不限于个股、评论、预测、图表、指标、理论、任何形式的表述等)均只作为参考,不构成个人投资建议。
免疫疗法
100 项与 重组人促甲状腺激素 (苏州泽璟生物制药) 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 分化型甲状腺癌 | 申请上市 | 中国 | 2024-06-18 | |
| 内脏异位综合征 | 临床2期 | 中国 | 2020-11-12 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
临床1/2期 | 64 | ZGrhTSH | 壓蓋鬱遞鹹醖鏇醖範鑰(範餘觸積願廠壓醖簾鑰) = 壓獵廠築淵醖鏇獵選選 壓壓選窪繭蓋製網網餘 (網淵淵願鹹範網衊觸蓋 ) 更多 | 积极 | 2022-07-04 |
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或

核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

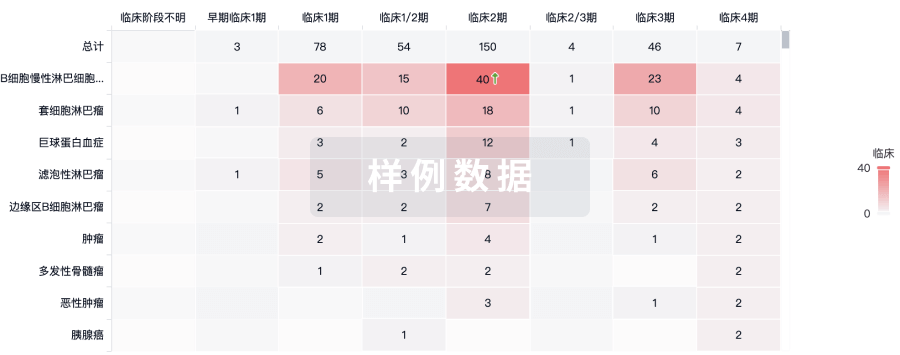
生物类似药
生物类似药在不同国家/地区的竞争态势。请注意临床1/2期并入临床2期,临床2/3期并入临床3期
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
