预约演示
更新于:2025-08-23
Factor VIII(Intas Biopharmaceuticals Ltd.)
凝血因子 VIII(Intas Biopharmaceuticals Ltd.)
更新于:2025-08-23
概要
基本信息
在研机构- |
权益机构- |
最高研发阶段撤市 |
首次获批日期- |
最高研发阶段(中国)- |
特殊审评- |
登录后查看时间轴
关联
100 项与 凝血因子 VIII(Intas Biopharmaceuticals Ltd.) 相关的临床结果
登录后查看更多信息
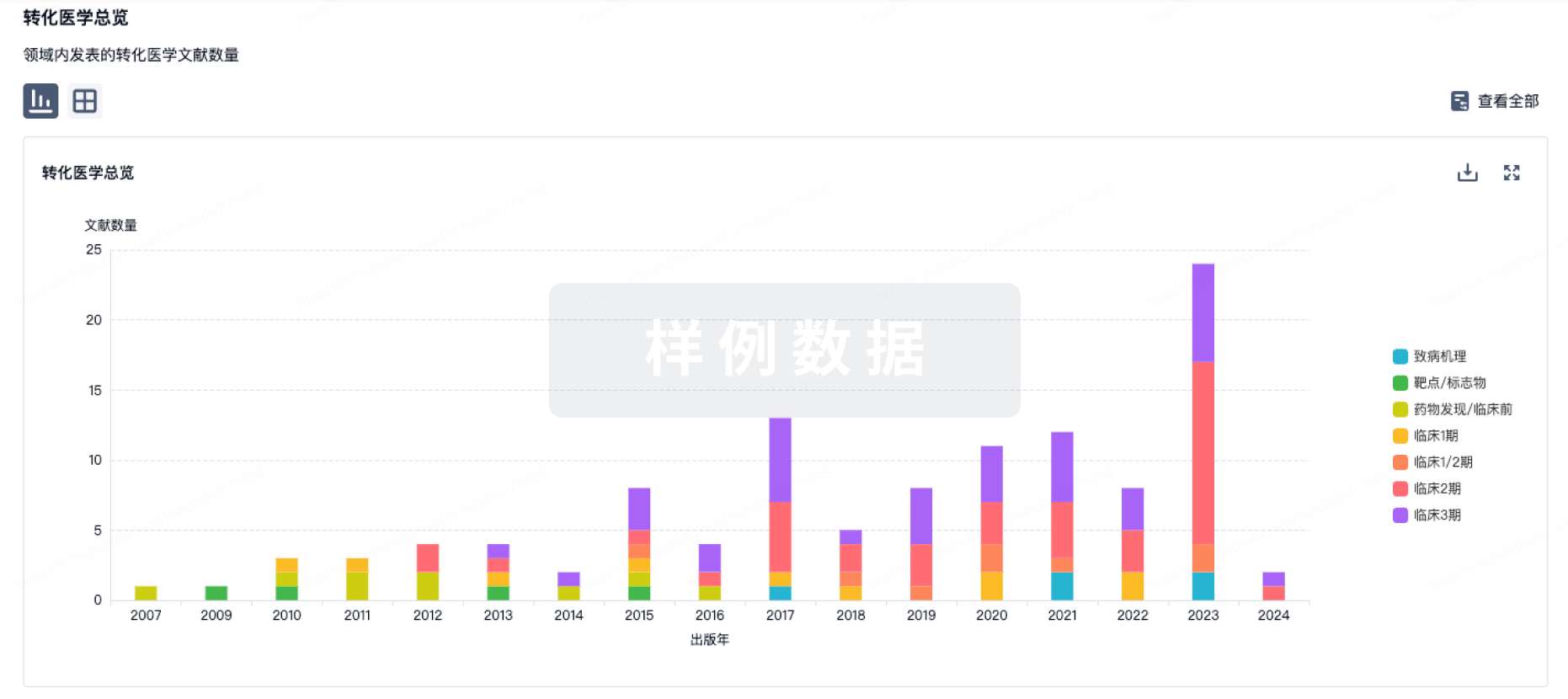
100 项与 凝血因子 VIII(Intas Biopharmaceuticals Ltd.) 相关的转化医学
登录后查看更多信息
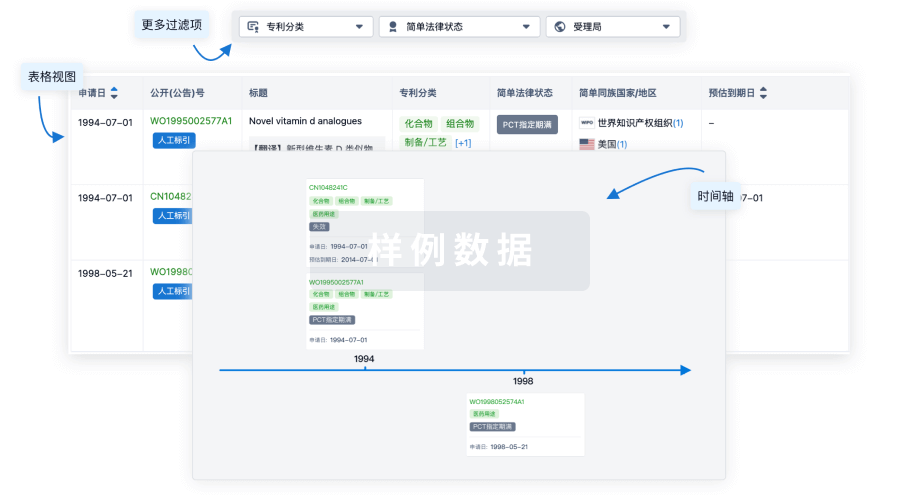
100 项与 凝血因子 VIII(Intas Biopharmaceuticals Ltd.) 相关的专利(医药)
登录后查看更多信息
2
项与 凝血因子 VIII(Intas Biopharmaceuticals Ltd.) 相关的新闻(医药)2022-08-26
·药明康德
今日,BioMarin Pharmaceutical公司宣布,欧盟委员会(EC)批准其用于治疗血友病A的基因疗法Roctavian(valoctocogene roxaparvovec)有条件上市,用于治疗严重血友病A成人患者。这些患者没有携带凝血因子VIII抑制物或针对腺相关病毒5(AAV5)抗体的病史。新闻稿指出,这款一次性治疗是首款治疗血友病A的获批基因疗法,有望显著减轻患者的治疗负担。
血友病A是由于缺乏凝血因子VIII而导致的一种罕见遗传性出血性疾病。凝血因子的缺乏使患者凝血酶生成不足,导致凝血障碍。血友病A以反复出血及其相关并发症为主要临床表现,其中约80%为关节出血,其并发症主要是慢性出血性关节病变,且可导致严重的关节畸形。目前,血友病A的主要治疗手段是定期输注凝血因子VIII,但频繁的输注给患者的生活带来了极大不便。
Roctavian是一种使用AAV5病毒载体递送表达因子VIII的转基因的基因疗法。它的优势在于患者可能只需要接受一次治疗,肝细胞就可以持续表达因子VIII,从而不再需要长期接受预防性凝血因子注射。
欧盟委员会的决定是基于Roctavian广泛的临床开发项目的整体数据,包括全球性3期临床试验GENEr8-1的结果。这一结果近日在《新英格兰医学杂志》上发表。数据显示,与入组前一年的数据相比,单次输注Roctavian后,受试者的年出血率(ABR)显著降低,凝血因子VIII使用频率降低,凝血因子VIII活性增加。患者的因子VIII使用率和需要接受治疗的ABR分别降低了99%和84%(p<0.001)。总体来看,90%(121/134)的试验参与者没有需要治疗的出血事件,或者与接受因子VIII预防性治疗相比出血事件减少。
有条件上市意味着BioMarin将按照预设的时间线提供正在进行的临床研究的更多数据,确认这一疗法的获益大于风险。
“Roctavian在欧盟获批是医药领域的历史性里程碑。它建立在超过40年的科学发现、创新和持续不懈的努力上。我们感谢欧盟委员会认识到Roctavian作为首款血友病A基因疗法的价值。”BioMarin主席兼首席执行官Jean-Jacques Bienaimé先生说,“我们也非常感谢患者群体和研究人员,他们为这一成就奉献了时间和精力,他们的愿景是让这款一次性疗法成为现实的驱动力。”
上周,bluebird bio公司的基因疗法Zynteglo(betibeglogene autotemcel,beti-cel)获得美国FDA批准上市,成为治疗需要接受常规血红细胞输注的β地中海贫血患者的首款获批基因疗法。今天,基因疗法在治疗血友病A方面再获突破。期待这一创新模式在治疗血液疾病方面获得更多突破,让患者摆脱终身接受治疗的负担!
参考资料:[1] First Gene Therapy for Adults with Severe Hemophilia A, BioMarin's ROCTAVIAN™ (valoctocogene roxaparvovec), Approved by European Commission (EC). Retrieved August 24, 2022, from https://www.prnewswire.com/news-releases/first-gene-therapy-for-adults-with-severe-hemophilia-a-biomarins-roctavian-valoctocogene-roxaparvovec-approved-by-european-commission-ec-301611980.html
内容来源于网络,如有侵权,请联系删除。
基因疗法
2022-05-12
Hemlibra Accounted For More Than 85% Of Global Bispecific Antibodies Sales In 2021
Global Bispecific Antibody Market Insight 2028 Report Highlights:
Detailed Market Sales & Trends Insight
Quarterly & Yearly Sales Insight Of Approved Antibodies Till Q1 2022
Global and Regional Market Analysis
Global Bispecific Antibody Market Opportunity Assessment: > USD 20 Billion
Market Sales Insight 2020 Till 2028
Approved Drug Sales Forecast Till 2028
Approved Drug In Market: 4 Drugs
Ongoing Clinical Trials Assessment by Status, Phase and Region
Key Market Dynamics
Download Report:
https://www.kuickresearch.com/report-global-bispecific-antibodies-antibody-market-size-blincyto-hemlibra-rybrevant-sales
Hemlibra is bispecific antibody which restores the hemostatic process and indicated for the routine prophylaxis to prevent or reduce the frequency of bleeding episodes in adult and pediatric patient’s ages newborn and older with hemophilia A with or without factor VIII inhibitors. It mainly acts by mimicking the action of clotting Factor VIIIa (Activated VIII) and hence maintains the normal process of blood clotting. Factor VIII lays an important role in the process of blood coagulation as it activates several other clotting factors.
In 2021 Hemlibra Accounted For More Than 85% Of Global Bispecific Antibodies Sales
It is product of Roche which gained approval in 2018. The regulatory bodies have approved Hemlibra as preventive treatment to minimize the frequency of bleeding episodes in children and adults, newborn and older, with hemophilia A with or without VIII inhibitors. It is administered subcutaneously (under the skin) and only once weekly, every two weeks or every four weeks. Owing to their ability to specifically target two different factors which are involved in clotting cascade, the drug has demonstrated significant blood control.
In 2021, Hemlibra accounted for about 85% share in the global market which is mainly attributed to surge in cases of hemophilia A and its encouraging response in the management of disease. For instance in 2021, the global sales of the drug have significantly increased by 40% in comparison to last year. Amid region, US is dominating the market which is attributed to rising awareness about the availability of bispecific antibody and presence of favorable reimbursement policies in the region. Genetech has developed Hemlibra Co-pay program which helps eligible patients to reduce their out-of pocket cost in their course of treatment. The eligible patient should not be government beneficiary and/or participant in a federal or state-funded health insurance program. The eligible patient in hemlibra co-pay program as low as US$ 5 per treatment to a maximum benefit of US$ 15,000 per year in drug co-pay costs.
Apart from Hemlibra, three other bispecific antibody constructs including Blincyto, Rybrevant, and Vabysmo have also entered the global market. Rybrevant and Vbysmo has reently entered the global market and are expected to follow similar sales pattern as Hemlibra and Blincyto, which will drive the growth of market during the forecast period. Till 2021, it has been demonstrated that the cumulative sales of bispecific antibodies were about US$ 9 Billion, thus indicating positive future of these antibody constructs in pharmaceutical market. The promising response of these drugs has also gained interest from pharmaceutical giants to actively invest in research and development activities related to bispecific antibodies.
As per our report findings, the global bispecific antibody market is expected to surpass US$ 20 Billion by 2028. It is expected that about 3-5 bispecific antibodies will gain approval in the market. For instance in 2022, European Medicine Agency has adopted a positive opinion on the conditional marketing approval of mosunetuzumab (Lunsumio). Mosunetuzumab developed Biogen is novel CD20xCD3 T-cell engaging bispecific antibody in development and is indicated for B-cell non-Hodgkin’s lymphoma (NHL), including follicular lymphoma (FL) and diffuse large B-cell lymphoma (DLBCL). In addition to this, rise in prevalence of chronic diseases, unmet need of targeted therapies, and ability of bispecific antibodies to target the multifactorial nature of chronic diseases will also drive the growth of market during the forecast period.
Our report provides comprehensive analysis on globally approved bispecific antibodies therapeutics along with their commercial information including patent, price, dosage, and quarterly and yearly sales till Q1 2022. Apart from this, the report also provides in-depth analysis on ongoing clinical trials in the market. The major players mentioned in the report include Amgen, Roche, Emergent Biosolution, Jounce Therapeutics, Eli Lilly, AstraZeneca, Regenron Pharmaceuticals, Genmab, and others.
抗体
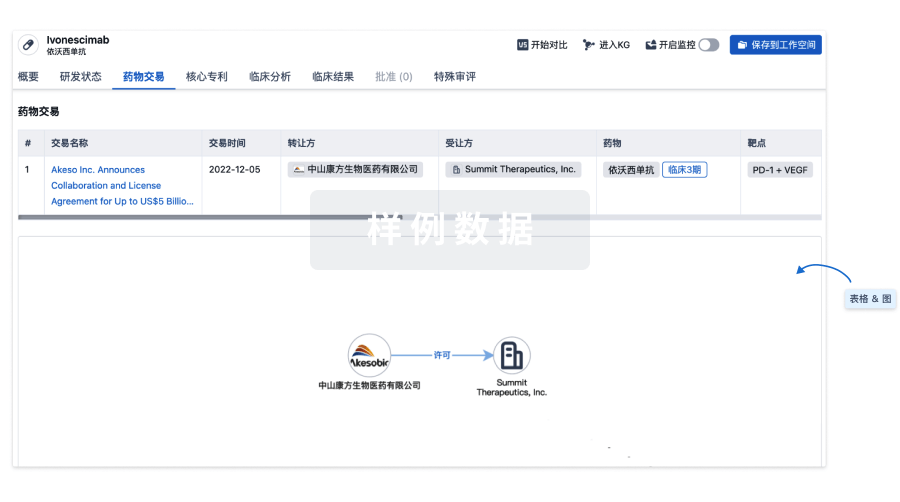
100 项与 凝血因子 VIII(Intas Biopharmaceuticals Ltd.) 相关的药物交易
登录后查看更多信息
研发状态
10 条最早获批的记录, 后查看更多信息
登录
| 适应症 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|
| 血友病A | - | - |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

生物类似药
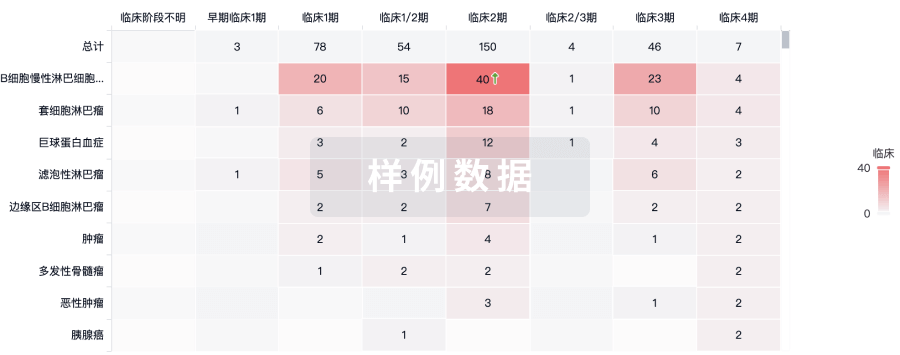
生物类似药在不同国家/地区的竞争态势。请注意临床1/2期并入临床2期,临床2/3期并入临床3期
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用