预约演示
更新于:2025-06-28
Nitroaspirin
更新于:2025-06-28
概要
基本信息
结构/序列
分子式C16H13NO7 |
InChIKeyIOJUJUOXKXMJNF-UHFFFAOYSA-N |
CAS号175033-36-0 |
关联
3
项与 Nitroaspirin 相关的临床试验NCT01001260
Biosynthesis of PGD2 in Vascular Injury
To investigate the biosynthesis of PGD2 during percutaneous transluminal coronary angioplasty (PTCA) procedure.
开始日期2007-08-01 |
申办/合作机构 |
NCT01256775
A Multicenter, Double-blind, Randomized, Parallel Group Study to Assess the Effect of NCX4016 vs Placebo on Walking Distance in Patients With Peripheral Arterial Occlusive Disease at Leriche-Fontaine Stage II
Peripheral arterial disease (PAD) is almost invariably associated with a generalized atherosclerotic involvement of the arterial tree and endothelial dysfunction. Previous short term studies showed improvement of vascular reactivity and walking capacity in PAD patients by measures aimed at restoring Nitric Oxide (NO) production. NO is also known to prevent the progression of atherosclerosis. We wished to assess whether the prolonged administration of a NO-donating agent (NCX 4016) improves the functional capacity of PAD patients and affects the progression of atherosclerosis as assessed by carotid intima-media thickness (IMT).
Four hundred forty two patients with stable intermittent claudication were enrolled in a prospective, double blind, placebo-controlled study and randomized to either NCX 4016 800mg bid or its placebo for 6 months. The primary study outcome was the absolute claudication distance (ACD) on a constant treadmill test (10% incline, 3km/hr); main secondary end-point was the change of the mean far-wall right common carotid artery IMT.
Four hundred forty two patients with stable intermittent claudication were enrolled in a prospective, double blind, placebo-controlled study and randomized to either NCX 4016 800mg bid or its placebo for 6 months. The primary study outcome was the absolute claudication distance (ACD) on a constant treadmill test (10% incline, 3km/hr); main secondary end-point was the change of the mean far-wall right common carotid artery IMT.
开始日期2003-09-01 |
申办/合作机构 |
NCT00157508
A Pilot, Randomised, Double-blind, Cross-over Study to Assess the Renal and Systemic Effects of NCX4016 in Patients With Type 2 Diabetes and Early Nephropathy
Aspirin is commonly used for treatment of painful and inflammatory diseases and in the prevention of the cardiovascular disease. A major drawback of aspirin treatment is the well recognized gastrointestinal toxicity. Recent research indicate that coupling a nitric oxide (NO)derivate to the aspirin moiety retains its therapeutic effects while avoiding its undesirable gastrointestinal side effects. NO has cytoprotective effects, such as blood flow modulation, mucus release and repair of mucosal injury. NCX4016, a NO-releasing derivative of acetylsalicilic acid, has been shown to retain the analgesic, anti-inflammatory and antithrombotic activity of aspirin, but with less gastrointestinal toxicity. In addition, preliminary data suggested that NCX4016 may restore insulin sensitivity in eNOS deficient mice.
This study was aimed to evaluate the activity of NCX4016, compared to aspirin, on albuminuria, insulin sensitivity and cardiac and renal hemodynamic in patients with type 2 diabetes mellitus. The patients after one month of placebo treatment, entered two 1-month treatments periods, with equivalent doses (800 mg of NCX4016, 325 mg of aspirin) of NCX4016 or aspirin.
This study was aimed to evaluate the activity of NCX4016, compared to aspirin, on albuminuria, insulin sensitivity and cardiac and renal hemodynamic in patients with type 2 diabetes mellitus. The patients after one month of placebo treatment, entered two 1-month treatments periods, with equivalent doses (800 mg of NCX4016, 325 mg of aspirin) of NCX4016 or aspirin.
开始日期2003-03-01 |
100 项与 Nitroaspirin 相关的临床结果
登录后查看更多信息
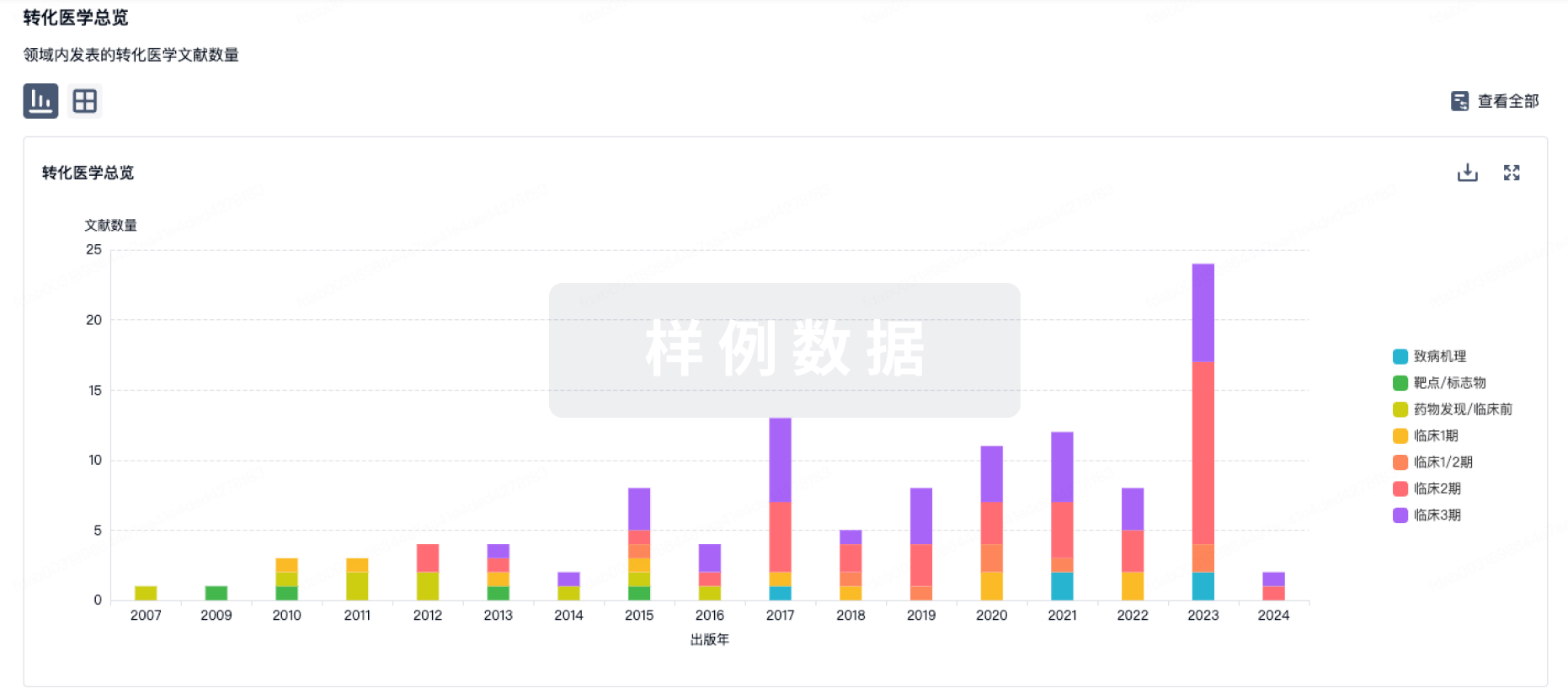
100 项与 Nitroaspirin 相关的转化医学
登录后查看更多信息
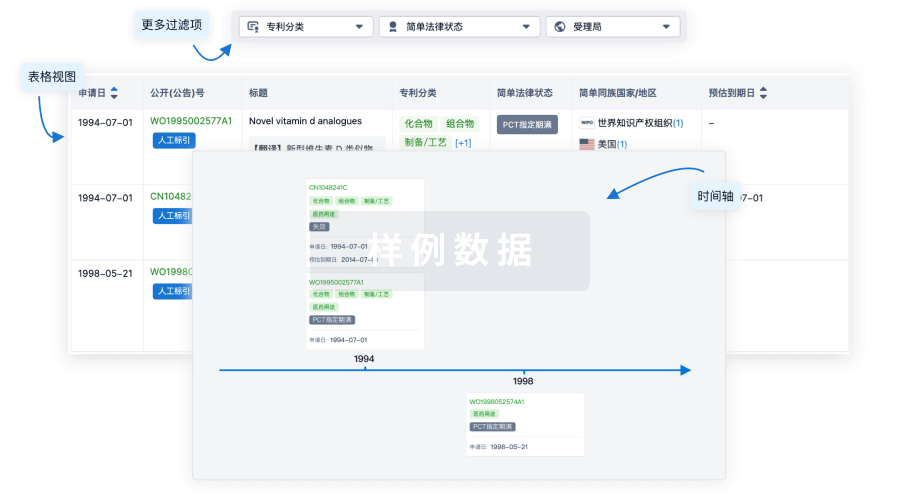
100 项与 Nitroaspirin 相关的专利(医药)
登录后查看更多信息
248
项与 Nitroaspirin 相关的文献(医药)2025-06-10·Circulation reports
An Aspirin-Free Strategy for Patients Undergoing Staged Percutaneous Coronary Intervention ― A Subgroup Analysis of the STOPDAPT-3 Trial ―
Article
作者: Nishida, Yasunori ; Natsuaki, Masahiro ; Kimura, Takeshi ; Ishino, Mitsunori ; Takenaka, Hiroyuki ; Ishikawa, Tetsuya ; Ando, Kenji ; Isawa, Tsuyoshi ; Yokomatsu, Takafumi ; Ono, Koh ; Nishikawa, Ryusuke ; Yamamoto, Ko ; Kitahara, Hideki ; Suwa, Satoru ; Yamaguchi, Koji ; Obayashi, Yuki ; Kozuma, Ken ; Doijiri, Tatsuki ; Morimoto, Takeshi ; Watanabe, Hirotoshi ; Chinen, Toshiya ; Kimura, Tomoya
Background:
No previous studies have evaluated the effect of an aspirin-free strategy for patients undergoing staged percutaneous coronary intervention (PCI).
Methods and Results:
We conducted a post hoc subgroup analysis in patients undergoing staged PCI within 1 month in STOPDAPT-3 (n=6,002), which randomly compared prasugrel monotherapy with dual antiplatelet therapy (DAPT) in patients with acute coronary syndrome or high bleeding risk. The co-primary endpoints were major bleeding (Bleeding Academic Research Consortium 3 or 5) and cardiovascular events (a composite of cardiovascular death, myocardial infarction, definite stent thrombosis, or stroke) at 1 month. There were 814 patients undergoing staged PCI within 1 month (no-aspirin group, n=401; DAPT group, n=413). The median interval from randomization to the first staged PCI was 8 (interquartile range 5-13) days. More than 90% of the patients received assigned antiplatelet agents at all staged PCI procedures. The effect of no-aspirin relative to DAPT was not different for the co-primary bleeding (3.74% vs. 1.94%; HR 1.94; 95% CI 0.82-4.57) and cardiovascular (3.49% vs. 2.42%; HR 1.44; 95% CI 0.64-3.25) endpoints. The no-aspirin group compared with the DAPT group had a numerically higher incidence of the co-primary cardiovascular endpoint, which occurred after the first staged PCI procedure (2.49% vs. 1.21%; HR 2.07; 95% CI 0.71-6.05).
Conclusions:
An aspirin-free prasugrel monotherapy relative to DAPT had numerically higher risks of cardiovascular and major bleeding events in patients undergoing staged PCI at 1 month.
2025-02-08·European Heart Journal-Cardiovascular Pharmacotherapy
An aspirin-free strategy for percutaneous coronary intervention in patients with diabetes: a pre-specified subgroup analysis of the STOPDAPT-3 trial
Article
作者: Ikari, Yuji ; Natsuaki, Masahiro ; Ishikawa, Tetsuya ; Kimura, Takeshi ; Takenaka, Hiroyuki ; Ogata, Nobuhiko ; Ando, Kenji ; Sugimoto, Atsuhiko ; Ishibashi, Yuki ; Nishikawa, Ryusuke ; Yamamoto, Ko ; Kaitani, Kazuaki ; Isawa, Tsuyoshi ; Suwa, Satoru ; Hashimoto, Katsushi ; Ono, Koh ; Miyabe, Tomonori ; Ikuta, Akihiro ; Obayashi, Yuki ; Masuda, Kazunori ; Morimoto, Takeshi ; Watanabe, Hirotoshi ; Kurita, Tairo
Abstract:
Aims:
Safety of aspirin-free strategy immediately after percutaneous coronary intervention (PCI) for cardiovascular events in patients with diabetes was unknown.
Methods and results:
We conducted the prespecified subgroup analysis on diabetes in the STOPDAPT-3 trial, which randomly compared prasugrel (3.75 mg/day) monotherapy (2984 patients) to dual antiplatelet therapy (DAPT) with prasugrel and aspirin (2982 patients) in patients with acute coronary syndrome or high bleeding risk. The co-primary endpoints were major bleeding events (Bleeding Academic Research Consortium 3 or 5) and cardiovascular events (a composite of cardiovascular death, myocardial infarction, definite stent thrombosis, or stroke) at 1 month. Of 5966 study patients, there were 2715 patients (45.5%) with diabetes. Patients with diabetes more often had chronic coronary syndrome, heart failure or cardiogenic shock, and comorbidities than those without. Patients with diabetes compared to those without had higher incidences of major bleeding and cardiovascular events. Regardless of diabetes, the effect of no-aspirin relative to DAPT was not different for the co-primary bleeding (diabetes: 5.05% vs. 5.47%; HR, 0.92; 95%CI, 0.66–1.28 and non-diabetes: 3.99% vs. 4.07%; HR, 0.98; 95%CI, 0.69–1.38; P for interaction = 0.81) and cardiovascular (diabetes: 5.54% vs. 5.15%; HR, 1.08; 95%CI, 0.78–1.49 and non-diabetes: 2.95% vs. 2.47%; HR, 1.20; 95%CI, 0.79–1.82; P for interaction = 0.70) endpoints. The incidences of subacute definite or probable stent thrombosis and any coronary revascularization were higher in the no-aspirin group than in the DAPT group regardless of diabetes.
Conclusions:
The effects of an aspirin-free prasugrel monotherapy (3.75 mg/day) relative to DAPT for major bleeding and cardiovascular events were not different regardless of diabetes.
2024-12-02·ChemMedChem
Virtual and in Vitro Screening Employing a Repurposing Approach Reveal 13‐cis‐Retinoic Acid is a PTP1B Inhibitor
Article
作者: Elena Mendieta‐Wejebe, Jessica ; Del Carmen Navarrete‐Mondragón, Reyna ; Cortés‐Benítez, Francisco ; González‐Andrade, Martin ; Pérez‐Villanueva, Jaime
Abstract:
Current treatments for type 2 diabetes (T2D) mainly rely on exercise, dietary control, and anti‐diabetic drugs to enhance insulin secretion and improve insulin sensitivity. However, there is a need for more therapeutic options, as approved drugs targeting different pharmacological objectives are still unavailable. One potential target that has attracted attention is the protein tyrosine phosphatase 1B (PTP1B), which negatively regulates the insulin signaling pathway. In this work, a comprehensive computational screening was carried out using cheminformatics and molecular docking on PTP1B, employing a rigorous repurposing approach. The screening involved approved drugs and compounds under research as anti‐diabetics that bind to targets such as peroxisome proliferator‐activated receptor gamma (PPAR‐γ) and α‐glucosidase. Several computational hits were then meticulously tested in vitro against PTP1B, with 13‐cis‐retinoic acid (3a) showing an IC50 of 0.044 mM and competitive inhibition. Molecular dynamics studies further confirmed that 3a can bind to the catalytic binding site of PTP1B. Finally, 3a is the first time it has been reported as an inhibitor of PTP1B, making it a potentially valuable candidate for further studies in D2T treatment.
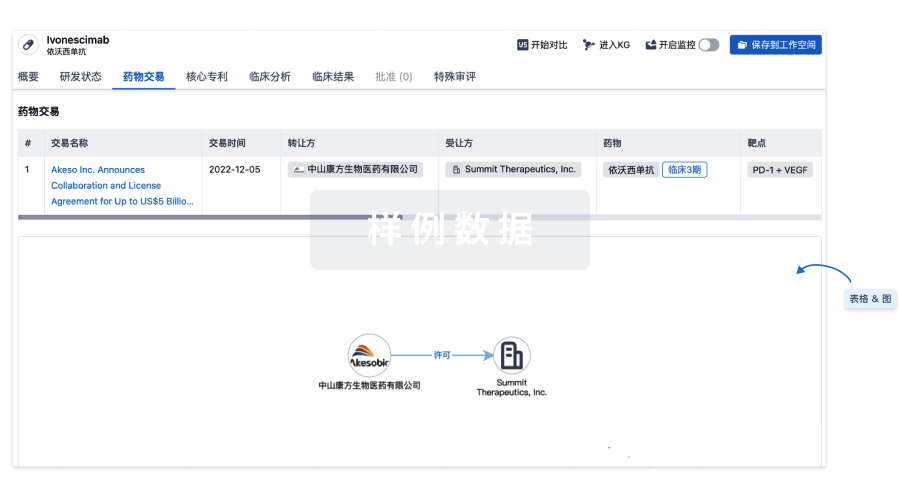
100 项与 Nitroaspirin 相关的药物交易
登录后查看更多信息
外链
| KEGG | Wiki | ATC | Drug Bank |
|---|---|---|---|
| - | - | - |
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 间歇性跛行 | 临床2期 | 意大利 | 2003-09-01 | |
| 外周动脉闭塞性疾病 | 临床2期 | 意大利 | 2003-09-01 | |
| 2型糖尿病 | 临床2期 | 意大利 | - | |
| 2型糖尿病 | 临床2期 | 瑞士 | - | |
| 疼痛 | 临床2期 | 美国 | - |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用