预约演示
更新于:2025-05-07
CLDN18.2-targeted CAR-T(Renji Hospital)
CLDN18.2-targeted CAR-T(仁济医院)
更新于:2025-05-07
概要
基本信息
药物类型 CAR-T |
别名- |
作用方式 抑制剂、拮抗剂 |
作用机制 CLDN18.2抑制剂(Claudin 18.2蛋白抑制剂)、CXCR4拮抗剂(C-X-C基序趋化因子受体4拮抗剂) |
在研适应症 |
非在研适应症- |
原研机构 |
在研机构 |
非在研机构- |
权益机构- |
最高研发阶段临床前 |
首次获批日期- |
最高研发阶段(中国)临床前 |
特殊审评- |
关联
100 项与 CLDN18.2-targeted CAR-T(仁济医院) 相关的临床结果
登录后查看更多信息
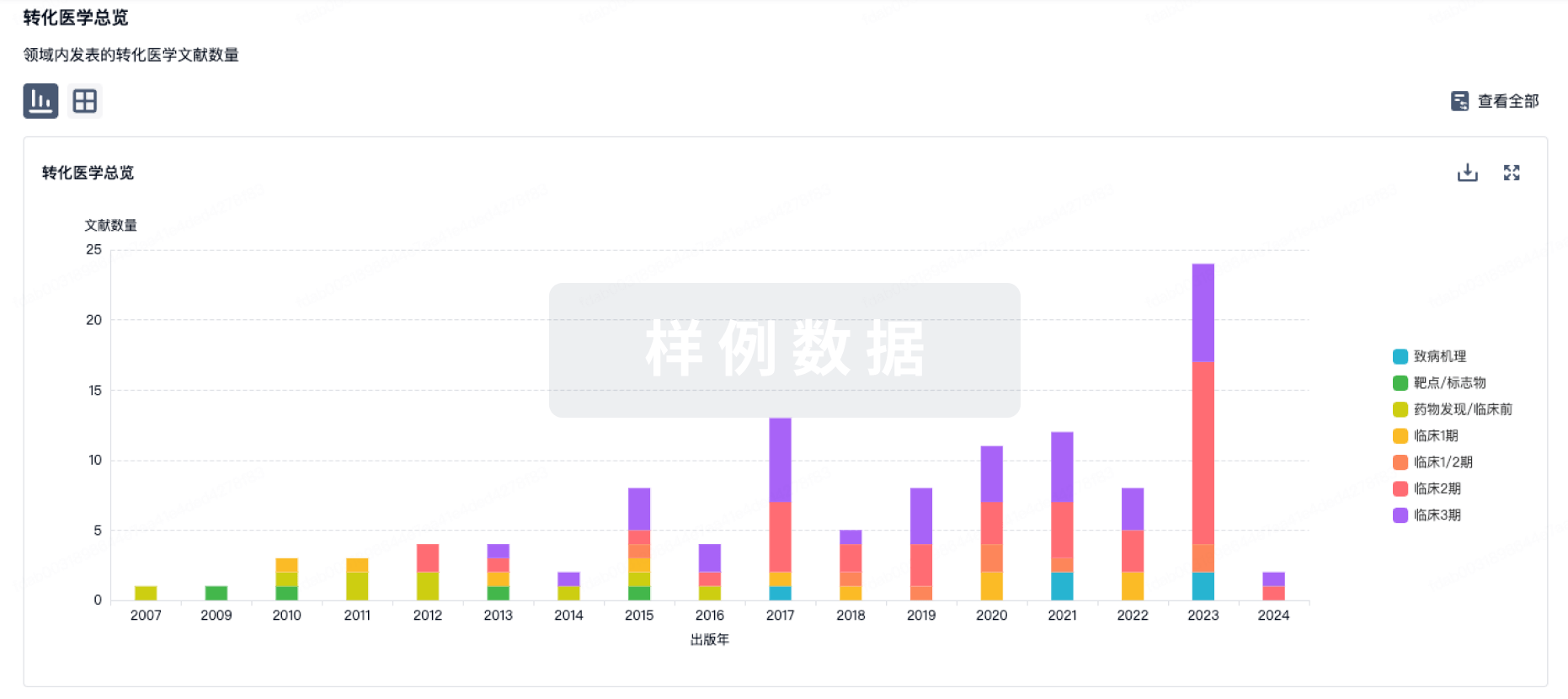
100 项与 CLDN18.2-targeted CAR-T(仁济医院) 相关的转化医学
登录后查看更多信息
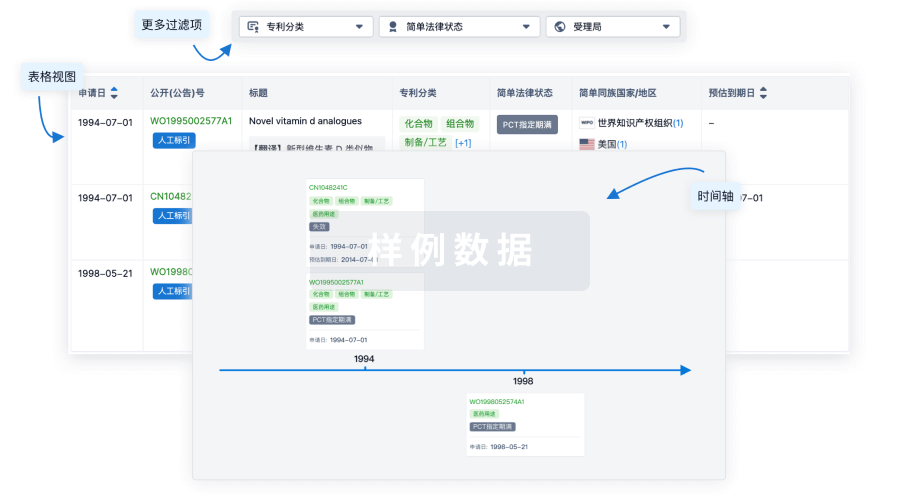
100 项与 CLDN18.2-targeted CAR-T(仁济医院) 相关的专利(医药)
登录后查看更多信息
3
项与 CLDN18.2-targeted CAR-T(仁济医院) 相关的文献(医药)2023-11-01·Molecular Therapy
CXCR4-modified CAR-T cells suppresses MDSCs recruitment via STAT3/NF-κB/SDF-1α axis to enhance efficacy against pancreatic cancer
Article
作者: Dong, Yiwei ; Luo, Hong ; Sun, Ruixin ; Sun, Yansha ; Liu, Yifan ; Jiang, Hua ; Wu, Chuanlong ; Du, Guoxiu ; Shi, Bizhi ; Zhou, Min ; Li, Zonghai
2019-04-01·JNCI: Journal of the National Cancer Institute
Claudin18.2-Specific Chimeric Antigen Receptor Engineered T Cells for the Treatment of Gastric Cancer
Article
作者: Li, Zonghai ; Shi, Bizhi ; Jia, Jie ; Wang, Huamao ; Zhang, Honghong ; Li, Qixiang ; Du, Guoxiu ; Jiang, Hua ; Wang, Peng ; Shi, Zhimin ; Yang, Linlin ; Wang, Cong
British Journal of Cancer
Peripheral blood neutrophils contribute to Claudin18.2-specific CAR-T cell treatment resistance in advanced gastric cancer
Article
作者: Tao, Min ; Xue, Ran ; Zhang, Panpan ; Zhang, Xiaotian ; Liu, Dan ; Li, Jiarui ; Ma, Mingyang ; Liu, Lian ; Shen, Lin ; Qi, Changsong ; Liu, Chang ; Zhang, Miao ; Zhang, Cheng ; Gong, Jifang
100 项与 CLDN18.2-targeted CAR-T(仁济医院) 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 胰腺导管腺癌 | 临床前 | 中国 | 2023-09-20 |
登录后查看更多信息
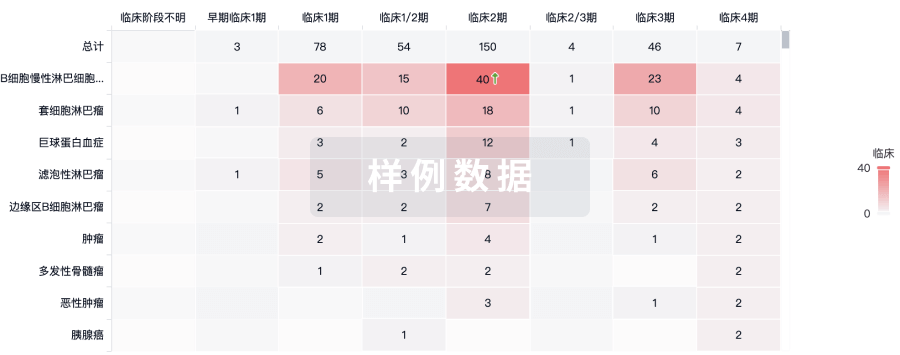
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或

核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
