预约演示
更新于:2025-05-16
Opelconazole
更新于:2025-05-16
概要
基本信息
原研机构 |
在研机构 |
非在研机构- |
权益机构- |
最高研发阶段临床3期 |
首次获批日期- |
最高研发阶段(中国)- |
特殊审评孤儿药 (欧盟) |
登录后查看时间轴
结构/序列
分子式C38H37F3N6O3 |
InChIKeyOSAMZQJKSCAOHA-CWRQMEKBSA-N |
CAS号1931946-73-4 |
关联
6
项与 Opelconazole 相关的临床试验NCT05238116
A Double-blind, Randomized, Placebo-controlled Study to Assess the Safety and Efficacy of Nebulized PC945 When Added to Systemic Antifungal Therapy for the Treatment of Refractory Invasive Pulmonary Aspergillosis (OPERA-T Study)
To assess the safety and efficacy of nebulized PC945 in combination with systemic antifungal therapy for the treatment of refractory IPA
开始日期2022-06-14 |
申办/合作机构 |
NCT05037851
A Randomized Controlled Open-label Study to Assess the Safety and Tolerability of Nebulized PC945 for Prophylaxis or Pre-emptive Therapy Against Pulmonary Aspergillosis in Lung Transplant Recipients (OPERA-S Study)
A study to evaluate the safety and tolerability of opelconazole for the prevention of fungal aspergillus infections in the lung in participants who have received a lung transplant.
开始日期2021-11-19 |
申办/合作机构 |
NCT03905447
An Open-label, Pilot Study to Assess Safety, Tolerability, Pharmacokinetics and Effects of Inhaled PC945 in the Pre-emptive Treatment of Aspergillus Fumigatus Colonisation in Lung Transplant Recipients
This study tests the effects of pre-emptive treatment with an experimental drug PC945 in lung transplant recipients whose lungs are infected by the fungus Aspergillus fumigatus.
PC945 may be useful in treating patients infected with Aspergillus fumigatus as, unlike the usual treatments, it is inhaled into the lung and has been designed to stay there and treat the infection. Participants will be monitored for up-to 12 weeks for the presence of Aspergillus in their lungs. Suitable participants will receive PC945 for an initial 28 days (Pre-emptive treatment phase) and, if needed, a further 8-weeks (Extended treatment phase).The amount of fungus in the patients' lungs will be measured over the course of the study. Participants with lung infections but not eligible for PC945 will be followed-up for 16-weeks on standard of care treatment. The study will take place at multiple sites in UK and 10 participants will receive PC945. The maximum study duration will be about 28 weeks.
PC945 may be useful in treating patients infected with Aspergillus fumigatus as, unlike the usual treatments, it is inhaled into the lung and has been designed to stay there and treat the infection. Participants will be monitored for up-to 12 weeks for the presence of Aspergillus in their lungs. Suitable participants will receive PC945 for an initial 28 days (Pre-emptive treatment phase) and, if needed, a further 8-weeks (Extended treatment phase).The amount of fungus in the patients' lungs will be measured over the course of the study. Participants with lung infections but not eligible for PC945 will be followed-up for 16-weeks on standard of care treatment. The study will take place at multiple sites in UK and 10 participants will receive PC945. The maximum study duration will be about 28 weeks.
开始日期2019-09-17 |
申办/合作机构 |
100 项与 Opelconazole 相关的临床结果
登录后查看更多信息
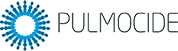
100 项与 Opelconazole 相关的转化医学
登录后查看更多信息
100 项与 Opelconazole 相关的专利(医药)
登录后查看更多信息
24
项与 Opelconazole 相关的文献(医药)2025-06-01·CLINICAL MICROBIOLOGY AND INFECTION
New treatment options for critically important WHO fungal priority pathogens
Review
作者: Egger, Matthias ; Kriegl, Lisa ; Hoenigl, Martin ; Krause, Robert ; Boyer, Johannes
BACKGROUND:
Yet often overlooked in public health discourse, fungal infections pose a crucial global disease burden associated with annual mortality rates approximately equal to tuberculosis and HIV. In response, the WHO published its first global priority list of fungal pathogens in 2022 assigning Aspergillus fumigatus, Candida albicans, Candida auris, and Cryptococcus neoformans to the critical group.
OBJECTIVES:
This review provides succinct insights into novel antifungals in development, aiming to contribute valuable information and perspectives with a focus on recent clinical findings and new treatment approaches for critical members of the WHO fungal pathogen priority list.
SOURCES:
PubMed literature search using 'Aspergillus fumigatus', 'Cryptococcus neoformans', 'Candida auris', and 'Candida albicans', along with the names of novel antifungal substances, including 'fosmanogepix', 'ibrexafungerp', 'opelconazole', 'oteseconazole', 'MAT2203', 'olorofim', and 'rezafungin' was conducted.
CONTENT:
For each critical pathogen, current issues and global clinical data from recent trials are covered. The remarkable development of three new antifungal therapeutics recently receiving Food and Drug Administration approval (ibrexafungerp-June 2021, oteseconazole -April 2022, and rezafungin-March 2023) is outlined, with two more exciting new antifungal substances, namely, olorofim and fosmanogepix expecting approval within the next years. Ibrexafungerp, fosmanogepix, and rezafungin have additionally been granted orphan drug status by the European Medicines Agency in Europe (ibrexafungerp-November 2021, fosmanogepix-July 2022, and rezafungin-January 2024).
IMPLICATIONS:
Although the limited number of targets and the emergence of resistance have posed challenges to antifungal treatment, new drugs such as ibrexafungerp, rezafungin, fosmanogepix, or olorofim have shown promising clinical efficacy. These drugs not only provide alternative options for invasive fungal infections but also alleviate treatment in outpatient settings. More clinical data, implementation of stewardship programmes, and surveillance, including utilization of drugs in agriculture, are necessary to prevent resistance development and to ensure the safety and efficacy of these new agents.
2025-03-13·ACS Medicinal Chemistry Letters
Is a Fungal Apocalypse Inevitable or Just a Hallucination? An Overview of the Antifungal Armamentarium Used in the Fight against Pathogenic Fungi
Review
作者: Hanafy, Doaa M. ; Leaver, David J.
The World Health Organization (WHO) fungal priority pathogens list (WHO FPPL) published in 2022 highlighted the inequity and research challenges faced by researchers who study pathogenic fungi that afflict humans. Antifungal drugs are the only weapon available to treat infections; however, these drugs are old, are not effective against multidrug-resistant (MDR) fungal strains, and are associated with substantial toxicity in clinical use. This Microperspective summarizes challenges pertaining to antifungal drug discovery in addition to highlighting recent advances and antifungal agents in clinical trials.
2024-02-28·Journal of the Pediatric Infectious Diseases Society
Pipeline of Novel Antifungals for Invasive Fungal Disease in Transplant Recipients: A Pediatric Perspective
Review
作者: Fisher, Brian T ; Hanisch, Benjamin R ; Huppler, Anna R ; Hsu, Alice Jenh
Abstract:
Invasive fungal disease (IFD) remains a significant cause of morbidity and mortality in children undergoing transplantation. There is a growing armamentarium of novel antifungal agents recently approved for use or in late stages of clinical development. The overarching goal of this review is to discuss the mechanisms of action, spectrum of activity, stage of development, and pediatric-specific data for the following agents: encochleated amphotericin B deoxycholate, fosmanogepix, ibrexafungerp, isavuconazole, olorofim, opelconazole, oteseconazole, and rezafungin. Additionally, key drug attributes of these novel agents and their potential future therapeutic roles in pediatric transplant recipients are discussed.
13
项与 Opelconazole 相关的新闻(医药)2024-04-15
Inhaled opelconazole observed to be generally well tolerated in this study as prophylaxis against pulmonary aspergillosis in lung transplant patients
Discontinuations due to drug-related adverse events and drug-drug interactions lower in the opelconazole group vs standard of care
Prevention and eradication of Aspergillus and Candida in the lungs observed with opelconazole monotherapy
LONDON, April 15, 2024 (GLOBE NEWSWIRE) -- Pulmocide Ltd., (“the Company”) a late-stage biopharmaceutical company developing novel inhaled therapies for patients suffering from serious acute and chronic respiratory diseases, today announced topline results from the OPERA-S study: a Phase 2 safety and tolerability study in lung transplant patients receiving inhaled opelconazole monotherapy as prophylaxis against pulmonary aspergillosis. Opelconazole is an investigational inhaled triazole antifungal being developed to prevent and treat pulmonary aspergillosis. In this study, opelconazole was generally well tolerated with a low incidence of drug-related adverse events (AEs) and a low incidence of treatment-limiting respiratory AEs. Importantly, there were no dose reductions or discontinuations of opelconazole prophylaxis or of immunosuppressant medications due to opelconazole-related drug-drug interactions (DDIs). Despite the expected small numbers, there was evidence of prevention of pulmonary aspergillosis and of eradication in the lungs of both Aspergillus and Candida colonization with opelconazole monotherapy.
In this open-label, active-controlled trial, 102 patients were randomized in the ICU after receiving a lung transplant in a 2:1 ratio to either inhaled opelconazole or standard of care (SOC) antifungal prophylaxis, and were treated for up to 12 weeks.
The safety and tolerability of opelconazole, the main focus of this study, and the ability to remain on antifungal prophylaxis and immunosuppressive therapy, were summarized descriptively as the study was not statistically powered for between group comparisons. Results from this trial indicated that opelconazole was generally safe and well tolerated. The number of related adverse events occurring in ≥ 2% of opelconazole patients was low. These were cough (6.2%), nausea (4.6%) and respiratory tract irritation (3.1%), all of which were mild or moderate in severity. Importantly, respiratory AEs related to opelconazole were rarely treatment-limiting, leading to discontinuation in two out of 65 opelconazole patients. Drug-related AEs together with DDIs leading to discontinuation of the antifungal medication, or DDIs leading to discontinuation of an immunosuppressant medication, occurred less commonly in the opelconazole group (7.7%) versus in the SOC antifungal prophylaxis group (27.3%). Numerically, more opelconazole patients (72.3%) completed the 12 weeks of prophylaxis compared to the initial SOC antifungal treatment (69.7%). Three patients in the study died: one in the opelconazole group (1.5%) and two in the SOC group (6%).
Efficacy in preventing breakthrough pulmonary Aspergillus disease and eradication of colonization were summarized descriptively as exploratory outcomes. As expected, given the relatively small sample size, the incidence of breakthrough fungal disease in the intent-to-treat population was low and similar between groups, in 4% of the opelconazole patients and in 3% of the SOC patients. In addition, opelconazole appeared to eradicate Aspergillus colonization in all six patients who entered the study already colonized. In two patients colonized prior to randomization with Fusarium and Penicillium, opelconazole also achieved eradication. Aspergillus colonization was also eradicated in the two SOC patients who were colonized at study entry. In addition, opelconazole eradicated Candida colonization of the airways in 12 of the 15 patients colonized at study entry (80%), providing additional evidence of opelconazole’s antifungal activity. In the SOC group, Candida colonization of the airways was eradicated in four of the six patients colonized at study entry (67%). One opelconazole patient (1.5%) and three SOC patients (9.1%) developed oral candidiasis during the study.
“The data support that inhaled opelconazole was generally safe and well tolerated in this study when administered as monotherapy prophylaxis in lung transplant patients, a critically ill patient population with major pulmonary morbidity,” stated Dr. Lance Berman, Chief Medical Officer of Pulmocide. “Based on discussions with clinicians who care for lung transplant patients, it appears that a potent antifungal agent delivered directly to the lungs with a low discontinuation rate and a negligible risk for DDIs would be a promising alternative. We believe that the use of opelconazole as a prophylaxis agent in patients at risk of pulmonary aspergillosis warrants further investigation.”
“As a physician who regularly treats these patients, I find the results to be very promising,” commented Dr. Shahid Husain, Professor of Medicine, Infectious Diseases, at the University of Toronto and who served on the study steering committee in addition to being an investigator in the trial. “If we can provide and maintain potent antifungal protection without having to compromise vital immunosuppressive therapy, then we may be able to further improve outcomes for our patients.”
More detailed results from this study are expected to be provided at medical meetings and through peer-reviewed publication in the months ahead.
About Opelconazole
Pulmocide’s investigational product, opelconazole, is a potent novel azole therapy specifically designed for inhaled use to maximize the amount of drug in the lung while providing minimal systemic exposure. This pro anticipated to enhance efficacy with a low risk of adding to the toxicities and drug-drug interactions seen with systemic antifungal therapies. Opelconazole has the potential to be useful in a variety of conditions where Aspergillus has been implicated, including chronic pulmonary aspergillosis, patients with severe asthma complicated by allergic bronchopulmonary aspergillosis, and severe flu or COVID-19 complicated by invasive aspergillosis. Opelconazole also has the potential to be used as prophylaxis in immunocompromised patients at risk of developing pulmonary aspergillosis, most commonly patients with an underlying hematological malignancy or recipients of a stem cell or solid organ transplant. Opelconazole is being supplied within the UK for patients with serious or life-threatening pulmonary aspergillosis according to the MHRA’s Guidance Note 14 (the Specials program). 1 Although drawing definitive conclusions regarding efficacy and safety from this program is limited by the open-label, non-randomized, uncontrolled nature of the program, observations suggest that in this program, inhaled opelconazole was generally well tolerated and effective in treating these patients.2, 3, 4 These clinical observations were noted in patients who had failed, or were intolerant of, prior antifungal therapy. These treatment responses led to advancing the clinical development of this investigational product which is currently in a Phase 3 clinical trial in patients with Invasive Pulmonary Aspergillosis (IPA) who are not responding to antifungal therapy (the OPERA-T study).5
About Pulmonary Aspergillosis
The incidence of pulmonary fungal disease has increased substantially over the past two decades with Aspergillus species being the most common pathogen.4 Invasive pulmonary aspergillosis is associated with high morbidity and mortality rates in immunocompromised patients including those undergoing hematological stem cell or solid organ transplantation (particularly lung transplants) and some patients in critical care, including those with COVID-19 or influenza-associated pulmonary aspergillosis.5 Aspergillus infection also plays an important role in severe asthma and cystic fibrosis and has been correlated with poorer clinical outcomes in patients with chronic obstructive pulmonary disease.5 Chronic lung infections with Aspergillus can leave patients with extensive and permanent lung damage, requiring a lifetime of antifungal treatment.5
About Pulmocide
Pulmocide Ltd ( ) is a late-stage biopharmaceutical company focused on the development of a novel inhaled azole therapy for patients at risk of developing serious complications associated with aspergillosis, such as immunocompromised patients and those with severe pulmonary diseases. The company is currently focused on acute and chronic treatments for pulmonary aspergillosis and its lead Phase 3 product opelconazole is being developed initially for the treatment of invasive pulmonary aspergillosis.
References:
MHRA. (2014). The supply of unlicensed medicinal products (“specials”). Retrieved from
Murray, A., Cass, L., Ito, K., et al. (2020). PC945, a Novel Inhaled Antifungal Agent, for the Treatment of Respiratory Fungal Infections. J Fungi (Basel), 6(4).
Pagani, N., Armstrong-James, D., & Reed, A. (2020). Successful salvage therapy for fungal bronchial anastomotic infection after -lung transplantation with an inhaled triazole anti-fungal PC945. J Heart Lung Transplant, 39(12), 1505-1506.
Singh, S., Moore, L. S. P., Mughal, N., et al. (2023). Novel inhaled antifungal for pseudomembranous Aspergillus tracheobronchitis complicating connective tissue disease. Thorax, 78(1), 110-111.
Pulmocide Contact:
Jennifer Giottonini Cayer
Chief Business Officer and Head of Corporate Development
Pulmocide Ltd
jcayer@pulmocide.com
Media Contact:
Michael Tattory
LifeSci Communications
mtattory@lifescicomms.com
临床结果临床3期临床2期免疫疗法
2024-01-03
LONDON, Jan. 03, 2024 (GLOBE NEWSWIRE) -- Pulmocide Ltd., (“the Company”) a late-stage biopharmaceutical company developing opelconazole for patients suffering from serious acute and chronic respiratory diseases, today announced that Dan Burgess, Chairman and CEO, will present a corporate update at the 42nd Annual J.P. Morgan Healthcare Conference on Wednesday, January 10, 2024 from 5:00pm – 5:25pm PT in San Francisco. About OpelconazolePulmocide’s investigational product, opelconazole, is a potent novel azole therapy specifically designed for inhaled use to maximize the amount of drug in the lung while providing minimal systemic exposure. This profile is anticipated to enhance efficacy with a low risk for adding to the toxicities and drug-drug interactions seen with systemic antifungal therapies. Under the United Kingdom’s Special Needs provision, opelconazole was found to be generally well tolerated and demonstrated remarkable clinical responses. In this program, patients with a variety of different clinical profiles who had failed previous antifungal treatment options responded well when opelconazole was added to their treatment regimen. Opelconazole has the potential to be useful in a variety of conditions where Aspergillus has been implicated, including chronic pulmonary aspergillosis, cystic fibrosis, severe asthma, allergic bronchopulmonary aspergillosis, chronic pulmonary obstructive disease, severe flu, and post-COVID-19-associated lung damage. A late-stage clinical program has been initiated to support registration in patients who have failed prior therapy for invasive pulmonary aspergillosis (IPA). The safety and efficacy of opelconazole is currently under evaluation in a Phase 3 clinical trial in patients with refractory IPA. Enrollment in a Phase 2 prophylaxis safety study in lung transplant recipients was recently completed with data expected in the first quarter of 2024. About Pulmonary AspergillosisThe incidence of pulmonary fungal disease has increased substantially over the past two decades with Aspergillus species being the most common pathogen.1 Invasive pulmonary aspergillosis is associated with high morbidity and mortality rates in immuno-compromised patients including those undergoing hematological stem cell or solid organ transplantation (particularly lung transplants) and some patients in critical care, including those with COVID-19 or influenza-associated pulmonary aspergillosis.2 Aspergillus infection also plays an important role in severe asthma and cystic fibrosis and has been correlated with poorer clinical outcomes in patients with chronic obstructive pulmonary disease.2 Chronic lung infections with Aspergillus can leave patients with extensive and permanent lung damage, requiring a lifetime of antifungal treatment.2 About PulmocidePulmocide Ltd (www.pulmocide.com) is a late-stage biopharmaceutical company focused on the development of a novel inhaled azole therapy for patients at risk of developing serious complications associated with aspergillosis, such as immunocompromised patients and those with severe pulmonary diseases. The company is currently focused on acute and chronic treatments for pulmonary aspergillosis and its lead product opelconazole is being developed initially for the treatment of invasive pulmonary aspergillosis. References Where Aspergillosis Comes From, Centers for Disease Control and Prevention, accessed 12 October 2023Kousha M. et al: Pulmonary aspergillosis: a clinical review. Eur Respir Rev, 2011; 20(212):156-174 For further information, please contact: Pulmocide Contact:Jennifer Giottonini CayerChief Business Officer and Head of Corporate DevelopmentPulmocide Ltdjennifer@pulmocide.com Media Contact:Michael TattoryLifeSci Communications mtattory@lifescicomms.com
临床3期临床结果临床2期
2023-10-17
Pulmocide Ltd., (“the Company”) a late-stage biopharmaceutical company developing novel inhaled therapies for patients suffering from serious acute and chronic respiratory diseases, today announced new clinical drug-drug interaction data for its inhaled antifungal agent, opelconazole, which was presented at ID Week 2023 in Boston, Massachusetts, on October 14, 2023.
Increased drug interactions have been previously reported to limit the use of preventative and therapeutic antifungal medications.1 This is particularly concerning for triazole antifungal agents which have Cytochrome P450 drug interactions with many of the anti-rejection and oncology drugs used to treat the patients’ underlying diseases.1 Based on previously performed in vitro drug-drug interaction data, opelconazole was anticipated to have a very low risk for Cytochrome P450 induction or inhibition.
The results from these in vitro studies subsequently informed the design of a Phase 1 drug-drug interaction study in 24 healthy volunteers. In this study, opelconazole, dosed to steady state concentrations, showed no inhibition of CYP3A4 using midazolam as the probe with an AUC0-24h geometric mean ratio of 1.13 (90% CI 1.05, 1.22), and no inhibition of CYP1A2 using caffeine as the probe with an AUC0-24h geometric mean ratio of 0.81 (90% CI 0.77, 0.86). Similar results were observed for geometric ratios using Cmax.2 These data fall below the threshold stipulated by the FDA Guidance on Clinical Drug Interaction Studies (geometric mean ratio of at least 1.25), suggesting opelconazole poses a negligible risk for an inhibitory effect.3 In this study, opelconazole was generally well tolerated with no serious adverse events reported and no evidence of bronchospasm by lung function testing.2
“Conversations with clinical experts treating patients with life threatening invasive pulmonary aspergillosis have indicated that the potential for drug-drug interactions with antifungal agents and those medications used to treat the underlying disease is a foremost concern,” said Dr. Lance Berman, Chief Medical Officer of Pulmocide. “Opelconazole was specifically designed to be administered via inhalation in order to achieve high lung concentrations and low systemic uptake. These low systemic levels, now observed in multiple clinical trials and in the UK Special Needs provision, have been estimated to be too low to have an inhibition or induction of a drug-drug interaction effect. We are encouraged that these clinical trial results confirm this low potential for Cytochrome P450 drug-drug interactions for opelconazole.”
About Opelconazole
Pulmocide’s investigational product, opelconazole, is a potent novel azole therapy specifically designed for inhaled use to maximize the amount of drug in the lung while providing minimal systemic exposure. This profile is anticipated to enhance efficacy with a low risk for adding to the toxicities and drug-drug interactions seen with systemic antifungal therapies. Under the United Kingdom’s Special Needs provision, opelconazole was found to be generally well tolerated and demonstrated remarkable clinical responses. In this program, patients with a variety of different clinical profiles who had failed previous antifungal treatment options responded well when opelconazole was added to their treatment regimen. Opelconazole has the potential to be useful in a variety of conditions where Aspergillus has been implicated, including chronic pulmonary aspergillosis, cystic fibrosis, severe asthma, allergic bronchopulmonary aspergillosis, chronic pulmonary obstructive disease, severe flu, and post-COVID-19-associated lung damage. A late-stage clinical program has been initiated to support registration in patients who have failed prior therapy for invasive pulmonary aspergillosis (IPA). The safety and efficacy of opelconazole is currently under evaluation in a Phase 3 clinical trial in patients with refractory IPA. Enrollment in a Phase 2 prophylaxis safety study in lung transplant recipients was recently completed with data expected in the first quarter of 2024.
About Pulmonary Aspergillosis
The incidence of pulmonary fungal disease has increased substantially over the past two decades with Aspergillus species being the most common pathogen.4 Invasive pulmonary aspergillosis is associated with high morbidity and mortality rates in immuno-compromised patients including those undergoing hematological stem cell or solid organ transplantation (particularly lung transplants) and some patients in critical care, including those with COVID-19 or influenza-associated pulmonary aspergillosis.5 Aspergillus infection also plays an important role in severe asthma and cystic fibrosis and has been correlated with poorer clinical outcomes in patients with chronic obstructive pulmonary disease.5 Chronic lung infections with Aspergillus can leave patients with extensive and permanent lung damage, requiring a lifetime of antifungal treatment.5
About Pulmocide
Pulmocide Ltd (www.pulmocide.com) is a late-stage biopharmaceutical company focused on the development of a novel inhaled azole therapy for patients at risk of developing serious complications associated with aspergillosis, such as immunocompromised patients and those with severe pulmonary diseases. The company is currently focused on acute and chronic treatments for pulmonary aspergillosis and its lead product opelconazole is being developed initially for the treatment of invasive pulmonary aspergillosis.
References
Patterson T. et al: Practice Guidelines for the Diagnosis and Management of Aspergillosis: 2016 Update by the Infectious Diseases Society of America; Clinical Infectious Disease, 2016;63(4):e1–60
The content above comes from the network. if any infringement, please contact us to modify.

临床结果临床3期临床1期
100 项与 Opelconazole 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 侵袭性肺曲霉菌病 | 临床3期 | 美国 | 2022-06-14 | |
| 侵袭性肺曲霉菌病 | 临床3期 | 阿根廷 | 2022-06-14 | |
| 侵袭性肺曲霉菌病 | 临床3期 | 澳大利亚 | 2022-06-14 | |
| 侵袭性肺曲霉菌病 | 临床3期 | 奥地利 | 2022-06-14 | |
| 侵袭性肺曲霉菌病 | 临床3期 | 比利时 | 2022-06-14 | |
| 侵袭性肺曲霉菌病 | 临床3期 | 巴西 | 2022-06-14 | |
| 侵袭性肺曲霉菌病 | 临床3期 | 加拿大 | 2022-06-14 | |
| 侵袭性肺曲霉菌病 | 临床3期 | 智利 | 2022-06-14 | |
| 侵袭性肺曲霉菌病 | 临床3期 | 哥伦比亚 | 2022-06-14 | |
| 侵袭性肺曲霉菌病 | 临床3期 | 法国 | 2022-06-14 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
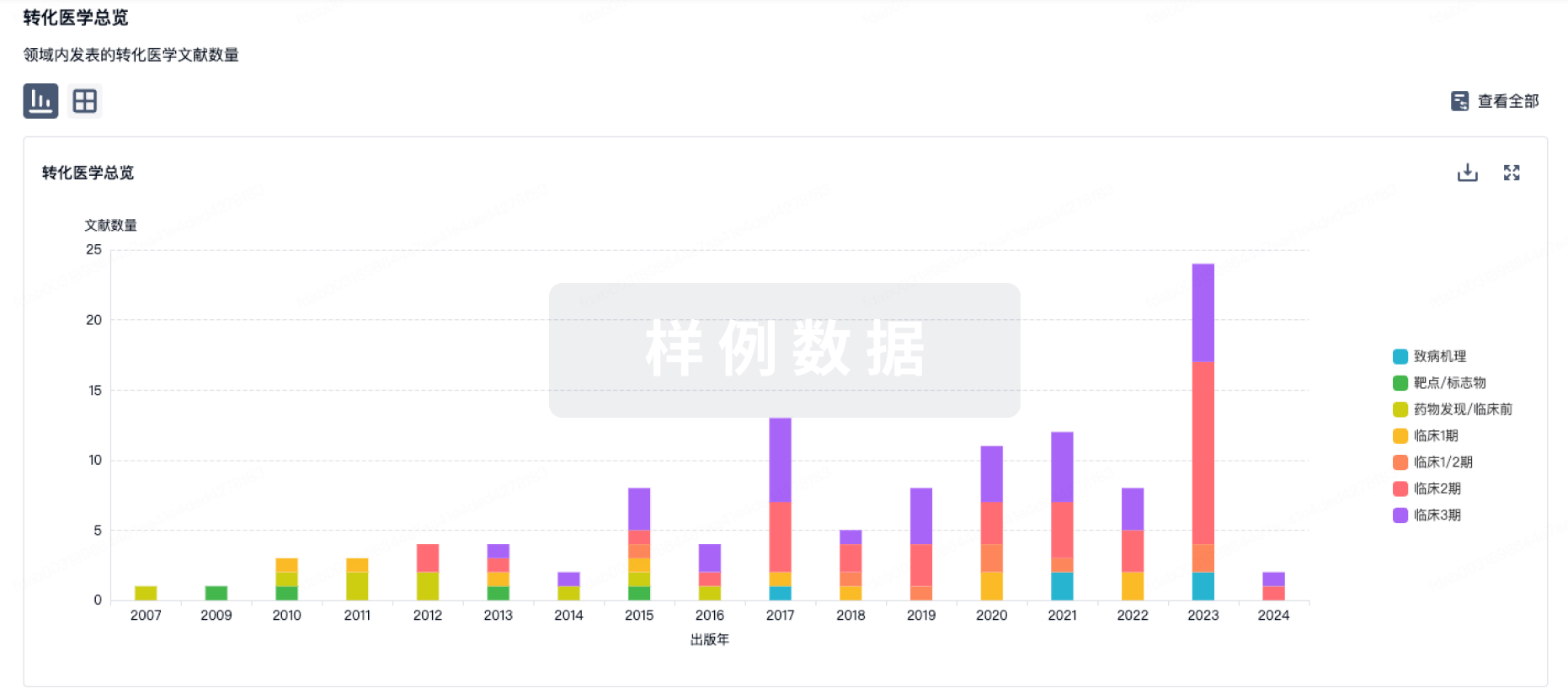
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
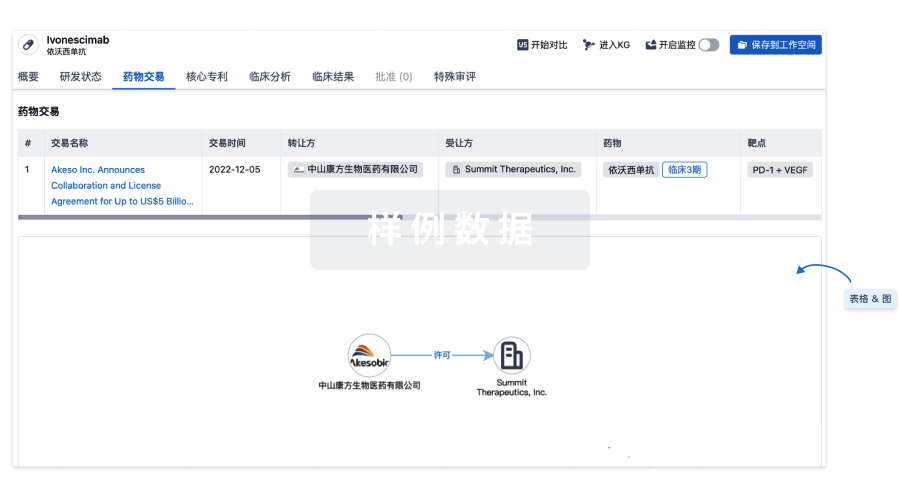
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用