预约演示
更新于:2025-08-02
MR3
更新于:2025-08-02
概要
基本信息
药物类型 纳米抗体 |
别名 MR3 |
作用方式 抑制剂 |
作用机制 SARS-CoV-2 S protein抑制剂(冠状病毒刺突糖蛋白抑制剂) |
在研适应症 |
非在研适应症- |
非在研机构- |
权益机构- |
最高研发阶段临床前 |
首次获批日期- |
最高研发阶段(中国)临床前 |
特殊审评- |
关联
100 项与 MR3 相关的临床结果
登录后查看更多信息
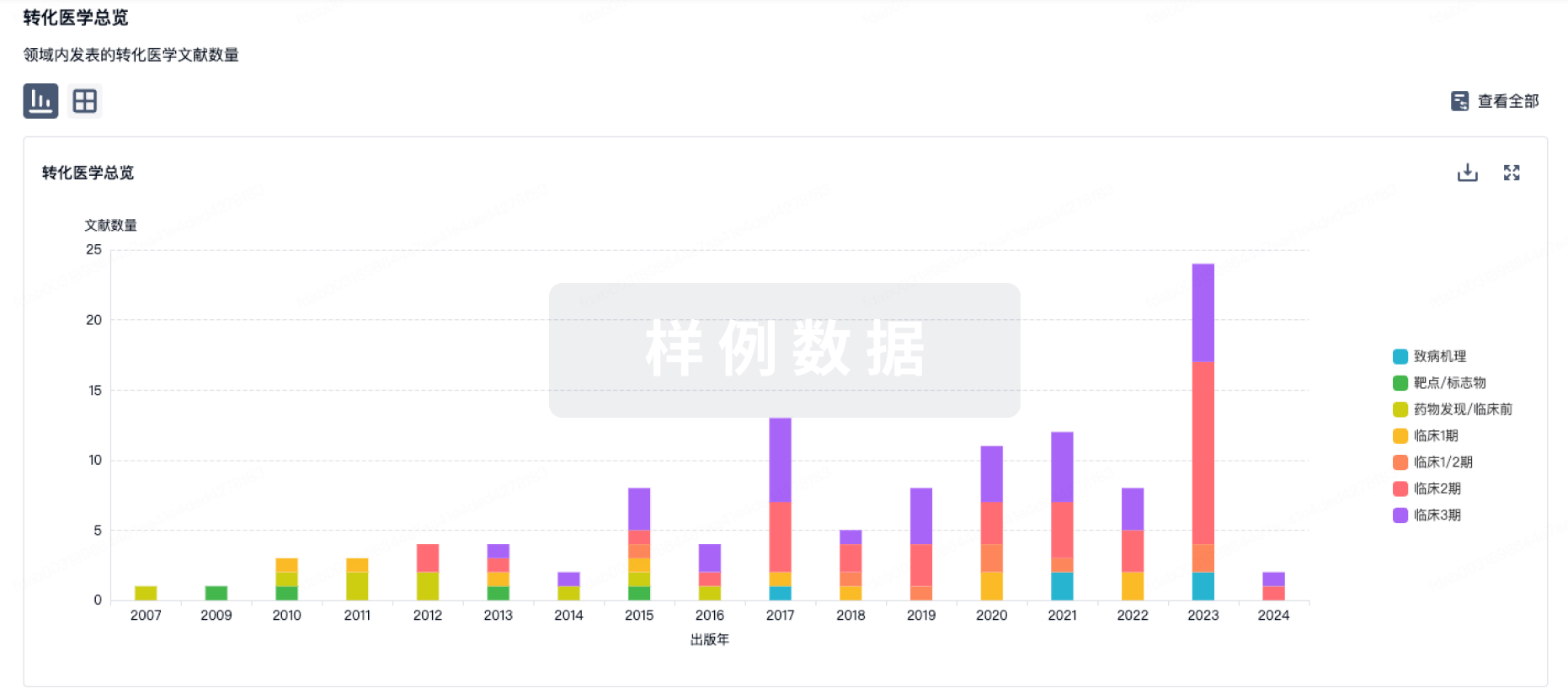
100 项与 MR3 相关的转化医学
登录后查看更多信息
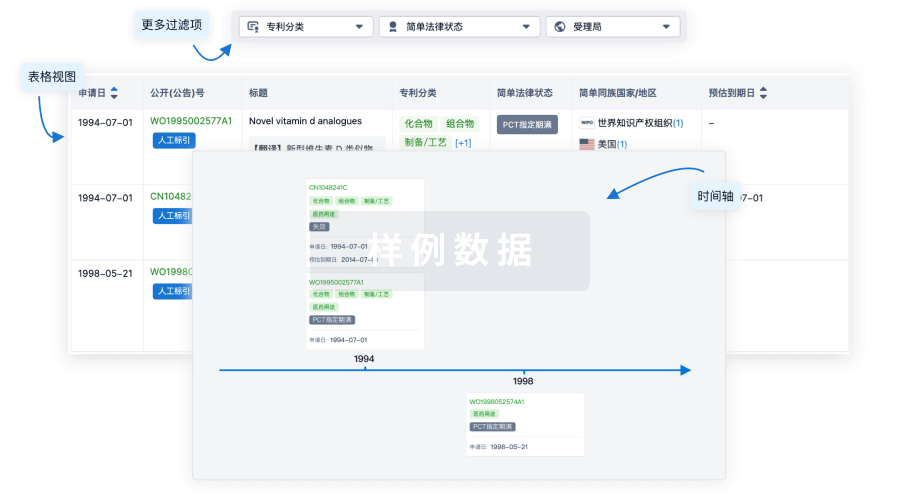
100 项与 MR3 相关的专利(医药)
登录后查看更多信息
13
项与 MR3 相关的文献(医药)2025-04-24·JOURNAL OF MEDICINAL CHEMISTRY
Rational Design of Methylene Blue–Raloxifene Conjugates for Efficient Breast Tumor Elimination Triggered by ERα Degradation
Article
作者: Mo, Xiaoman ; Dong, Yongxi ; Zhang, Silong ; He, Huan ; Wang, Ziwei ; Liu, Bing ; Qing, Luolong ; Yu, Bingqiong ; Zhang, Yu ; Yu, Qiying ; Pan, Weidong ; Chai, Yue’e
Small molecules capable of degrading estrogen receptor α (ERα) are of significant interest in breast cancer treatment. Herein, we rationally designed a series of ERα degraders (MR1-MR3) by conjugating methylene blue, a bifunctional photosensitizer, with the raloxifene pharmacophore. The lead compound MR3 exhibited high affinity to ERα, and it can induce a complete depletion of ERα in MCF7 breast cancer cells after 660 nm irradiation (0.4 W/cm2) for 1 min. Owing to the ERα degradation merit, MR3 displayed a 45-fold boosted anticancer activity (IC50 = 0.55 μM) after irradiation. In the breast cancer xenograft mouse model, MR3 induced an obvious tumor regression (tumor growth inhibition = 118%), which was superior to that of the FDA-approved ERα degrader Faslodex. These important features make MR3 extremely intriguing for breast cancer treatment.
2017-01-01·Annals of hematology3区 · 医学
Imatinib dose reduction in patients with chronic myeloid leukemia in sustained deep molecular response
3区 · 医学
Article
作者: Osorio, Santiago ; Pereira, Arturo ; Jiménez-Velasco, Antonio ; Correa, Juan-Gonzalo ; Pérez, Isabel ; Cervantes, Francisco ; Sánchez-Guijo, Fermín ; Redondo, Sara ; Colomer, Dolors ; Ferrer-Marín, Francisca ; Steegmann, Juan-Luis ; García-Gutiérrez, Valentín
To determine whether a lower imatinib dose could minimize toxicity while maintaining the molecular response (MR), imatinib dose was reduced to 300 mg daily in 43 patients with chronic myeloid leukemia (CML) in sustained deep molecular response to first-line imatinib 400 mg daily. At the time of dose reduction, median duration of the deep response was 4.1 (interquartile range (IQR) 2.2-5.9) years; molecular response was MR4, MR4.5, and MR5 of the international scale in 6, 28, and 9 patients, respectively. Toxicity grade was 1, 2, and 3 in 28, 8, and 1 patients, respectively; 6 patients underwent dose reduction without having side effects. With a median of 1.6 (IQR 0.7-3.2) years on imatinib 300 mg daily, only one patient lost the deep molecular response to MR3. At the last follow-up, response was MR3, MR4, MR4.5, and MR5 in 1, 3, 9, and 30 patients, respectively. Toxicity improvement was observed in 23 (62.2 %) of the 37 patients with side effects, decreasing to grade 0 in 20 of them. All but one anemic patients improved (p = 0.01), the median Hb increase in this subgroup of patients being 1 g/dL. In CML patients with sustained deep response to the standard imatinib dose, reducing to 300 mg daily significantly improves tolerability and preserves efficacy.
2013-11-01·Toxicology and applied pharmacology3区 · 医学
3,5,4′-Trimethoxystilbene, a natural methoxylated analog of resveratrol, inhibits breast cancer cell invasiveness by downregulation of PI3K/Akt and Wnt/β-catenin signaling cascades and reversal of epithelial–mesenchymal transition
3区 · 医学
Article
作者: Wei-Jen Chen ; Tzong-Der Way ; Hui-Mei Hong ; Jie-Heng Tsai ; Chih-Li Lin ; Min-Hsiung Pan ; Li-Sung Hsu
The molecular basis of epithelial-mesenchymal transition (EMT) functions as a potential therapeutic target for breast cancer because EMT may endow breast tumor-initiating cells with stem-like characteristics and enable the dissemination of breast cancer cells. We have recently verified the antitumor activity of 3,5,4'-trimethoxystilbene (MR-3), a naturally methoxylated derivative of resveratrol, in colorectal cancer xenografts via an induction of apoptosis. The effect of MR-3 on EMT and the invasiveness of human MCF-7 breast adenocarcinoma cell line were also explored. We found that MR-3 significantly increased epithelial marker E-cadherin expression and triggered a cobblestone-like morphology of MCF-7 cells, while reciprocally decreasing the expression of mesenchymal markers, such as snail, slug, and vimentin. In parallel with EMT reversal, MR-3 downregulated the invasion and migration of MCF-7 cells. Exploring the action mechanism of MR-3 on the suppression of EMT and invasion indicates that MR-3 markedly reduced the expression and nuclear translocation of β-catenin, accompanied with the downregulation of β-catenin target genes and the increment of membrane-bound β-catenin. These results suggest the involvement of Wnt/β-catenin signaling in the MR-3-induced EMT reversion of MCF-7 cells. Notably, MR-3 restored glycogen synthase kinase-3β activity by inhibiting the phosphorylation of Akt, the event required for β-catenin destruction via a proteasome-mediated system. Overall, these findings indicate that the anti-invasive activity of MR-3 on MCF-7 cells may result from the suppression of EMT via down-regulating phosphatidylinositol 3-kinase (PI3K)/AKT signaling, and consequently, β-catenin nuclear translocation. These occurrences ultimately lead to the blockage of EMT and the invasion of breast cancer cells.
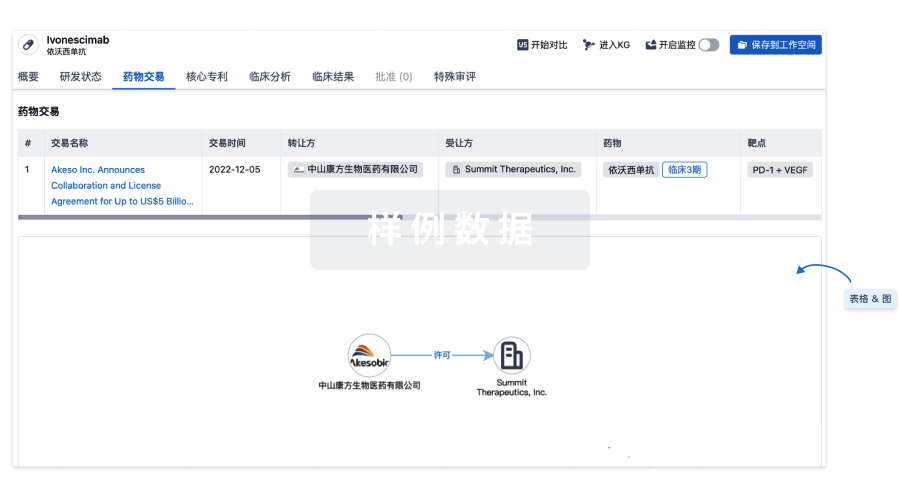
100 项与 MR3 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 新型冠状病毒感染 | 临床前 | 中国 | 2021-07-30 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
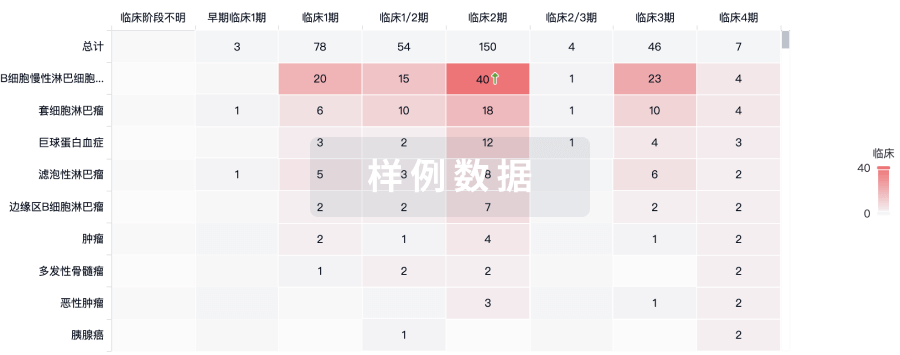
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

生物类似药
生物类似药在不同国家/地区的竞争态势。请注意临床1/2期并入临床2期,临床2/3期并入临床3期
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用