预约演示
更新于:2025-06-21
DLP-201
更新于:2025-06-21
概要
基本信息
原研机构 |
在研机构- |
非在研机构 |
权益机构- |
最高研发阶段无进展药物发现 |
首次获批日期- |
最高研发阶段(中国)- |
特殊审评- |
关联
2
项与 DLP-201 相关的临床试验ISRCTN85736336
Controlled study of hepatitis B virus level alteration in hepatocellular carcinoma: monotherapy with transcatheter arterial chemoembolisation versus double therapy with transcatheter arterial chemoembolisation and interferon-alpha: a randomised controlled trial
开始日期2008-12-01 |
申办/合作机构- |
EUCTR2005-005161-11-IT
Treatment with leucocytic interferon-alpha more ribavirine towards peg-interferon to reduced doses more ribavirine in patients affections from positive chronic hepatitis HCV that in course of arranged therapy demand the reduction of the peghilato dosage of interferon. - ND
开始日期2005-08-01 |
申办/合作机构- |
100 项与 DLP-201 相关的临床结果
登录后查看更多信息
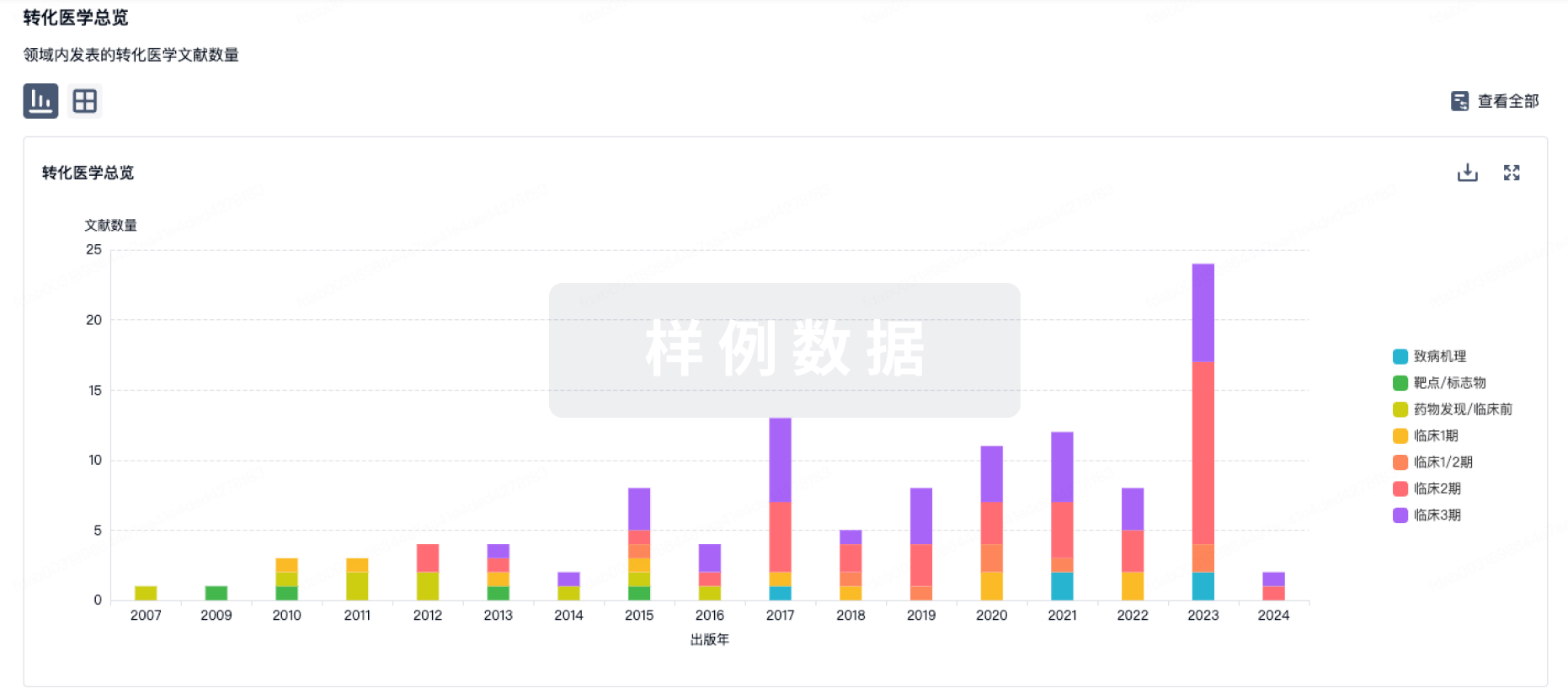
100 项与 DLP-201 相关的转化医学
登录后查看更多信息
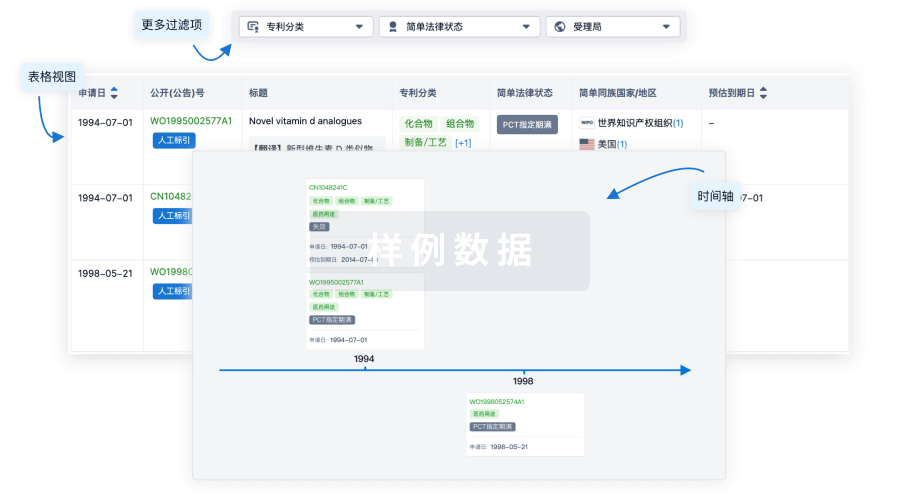
100 项与 DLP-201 相关的专利(医药)
登录后查看更多信息
3,252
项与 DLP-201 相关的文献(医药)2025-08-01·LEUKEMIA RESEARCH
Treatment strategy for indolent adult T-cell leukemia-lymphoma
Article
作者: Imaizumi, Yoshitaka ; Miyazaki, Yasushi ; Kato, Takeharu
Adult T-cell leukemia-lymphoma (ATL), a distinct peripheral T-lymphocytic malignancy associated with human T-lymphotropic virus type-1, can be classified into four subtypes based on clinical manifestations: acute, lymphoma, chronic, and smoldering types. The smoldering and chronic types without poor prognostic factors are classified as indolent ATL. Watchful waiting until disease progression and skin-directed therapy have been recommended as standard treatment strategies, and combination therapy with interferon-alpha and the antiviral drug zidovudine may be used in some cases. High-risk cases for prognosis, identified based on prognostic scores such as Indolent ATL-Prognostic index (iATL-PI) and various biomarkers, should be carefully monitored. Furthermore, early intervention methods must be developed and validated for these cases.
2025-03-01·BRAIN BEHAVIOR AND IMMUNITY
Neurotransmitter and metabolic effects of interferon-alpha in association with decreased striatal dopamine in a non-human primate model of cytokine-Induced depression
Article
作者: Tharp, Gregory K ; Bosinger, Steven E ; Felger, Jennifer C ; Block, Andrew M ; Bekhbat, Mandakh ; Dickinson, Sarah Y
Inflammatory stimuli administered to humans and laboratory animals affect mesolimbic and nigrostriatal dopaminergic pathways in association with impaired motivation and motor activity. Alterations in dopaminergic corticostriatal reward and motor circuits have also been observed in depressed patients with increased peripheral inflammatory markers. The effects of peripheral inflammation on dopaminergic pathways and associated neurobiologic mechanisms and consequences have been difficult to measure in patients. Postmortem tissue (n = 11) from an established, translationally-relevant non-human primate model of cytokine-induced depressive behavior involving chronic interferon-alpha (IFN-a) administration was utilized herein to explore the molecular mechanisms of peripheral cytokine effects on striatal dopamine. Dopamine (but not serotonin or norepinephrine) was decreased in the nucleus accumbens (NAcc) and putamen of IFN-a-treated animals (p < 0.05). IFN-a had no effect on number of striatal neurons or dopamine terminal density, suggesting no overt neurodegenerative changes. RNA sequencing examined in the caudate, putamen, substantia nigra, and prefrontal cortical subregions revealed that while IFN-a nominally up-regulated limited numbers of genes enriching inflammatory signaling pathways in all regions, robust, whole genome-significant effects of IFN-a were observed specifically in putamen. Genes upregulated in the putamen primarily enriched synaptic signaling, glutamate receptor signaling, and inflammatory/metabolic pathways downstream of IFN-a, including MAPK and PI3K/AKT cascades. Conversely, gene transcripts reduced by IFN-a enriched oxidative phosphorylation (OXPHOS), protein translation, and pathways regulated by dopamine receptors. Unsupervised clustering identified a gene co-expression module in the putamen that was associated with both IFN-a treatment and low dopamine levels, which enriched similar inflammatory, metabolic, and synaptic signaling pathways. IFN-a-induced reductions in dopamine further correlated with genes related to excitotoxic glutamate, kynurenine, and altered dopamine receptor signaling (r = 0.78-97, p < 0.05). These findings provide insight into the immunologic mechanisms and neurobiological consequences of peripheral inflammation effects on dopamine, which may inform novel treatment strategies targeting inflammatory, metabolic or neurotransmitter systems in depressed patients with high inflammation.
2025-02-27·BLOOD
Targeted interferon therapy with modakafusp alfa for relapsed or refractory multiple myeloma
Article
作者: Kaufman, Jonathan L. ; Li, Cheryl ; Biran, Noa ; Vogl, Dan T. ; Holstein, Sarah A. ; Chaudry, Maria ; Atrash, Shebli ; Suryanarayan, Kaveri ; Collins, Sabrina ; Benson, Don ; Nadeem, Omar ; Liu, Yuyin ; Parot, Xavier
Abstract:
Interferon alfa has activity against multiple myeloma (MM). Modakafusp alfa is an immunocytokine comprising 2 attenuated interferon alfa-2b molecules and an anti-CD38 immunoglobulin G4 antibody, targeting delivery of interferon alfa to CD38-expressing (CD38+) immune and myeloma cells. This phase 1/2 trial enrolled patients with relapsed/refractory multiple myeloma with ≥3 prior lines of treatment and refractory to, or intolerant of, ≥1 proteasome inhibitor and ≥1 immunomodulatory drug. During dose escalation, modakafusp alfa was administered at 10 doses in 4 schedules across 13 cohorts. The primary end point was safety for dose escalation, and overall response rate (ORR) for dose expansion. We enrolled 106 patients who had received a median of 6.5 lines of prior therapy; 84% of patients had myeloma previously refractory to an anti-CD38 antibody. The most feasible dosing schedule was every 4 weeks (Q4W), at which the maximum tolerated dose was 3 mg/kg. Among 30 patients treated at 1.5 mg/kg Q4W, the ORR was 43.3%, with a median duration of response of 15.1 months (95% confidence interval [CI], 7.1-26.1); median progression-free survival was 5.7 months (95% CI, 1.2-14). Grade ≥3 adverse events (AEs) occurred in 28 (93.3%) patients, the most common were neutropenia (66.7%) and thrombocytopenia (46.7%); infections were reported in 8 (26.7%) patients (including grade 3 in 4 [16.7%]). Modakafusp alfa therapy induced upregulation of the type 1 interferon gene signature score, increased CD38 receptor density in CD38+ cells, and innate and adaptive immune cell activation. Modakafusp alfa resulted in antitumor activity and immune activation in patients with MM. AEs were primarily hematologic. This trial was registered at www.clinicaltrials.gov as #NCT03215030.
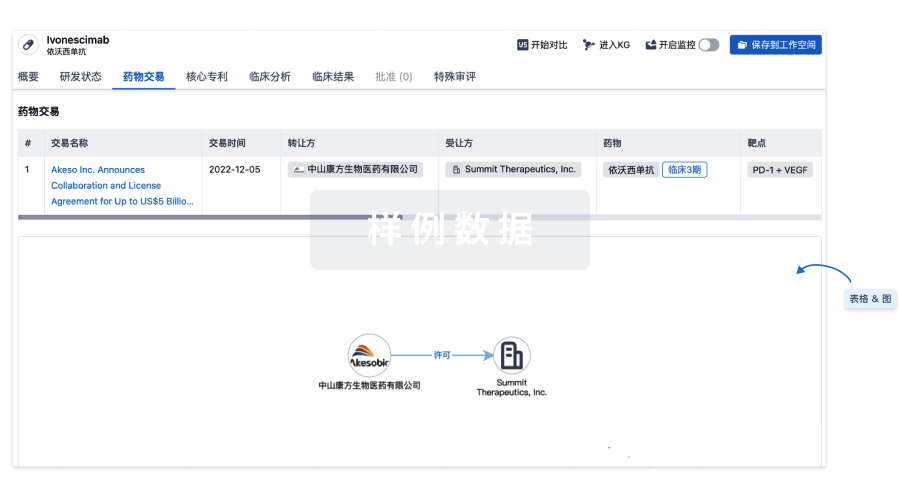
100 项与 DLP-201 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 丙型肝炎 | 药物发现 | 美国 | - |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
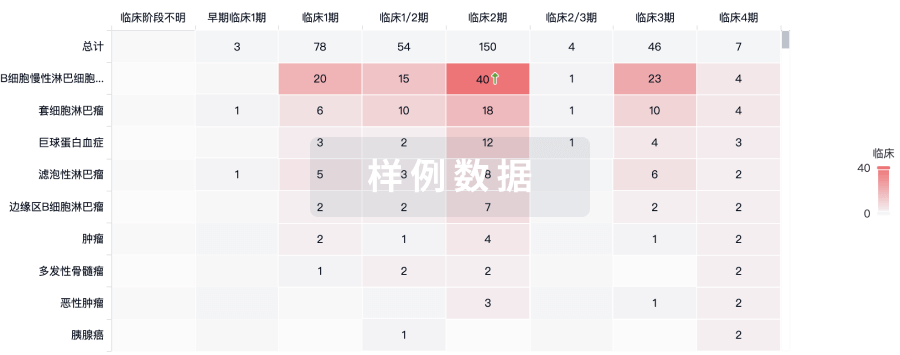
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

生物类似药
生物类似药在不同国家/地区的竞争态势。请注意临床1/2期并入临床2期,临床2/3期并入临床3期
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
