预约演示
更新于:2025-05-31
LC autologous blood origin T lymphocyte
更新于:2025-05-31
概要
基本信息
原研机构 |
非在研机构- |
最高研发阶段批准上市 |
首次获批日期 韩国 (2007-08-01), |
最高研发阶段(中国)- |
特殊审评- |
登录后查看时间轴
关联
9
项与 LC autologous blood origin T lymphocyte 相关的临床试验NCT06620510
A Multicenter, Retrospective Data Analysis Study on the Long-term Survival Rate of the 'Immuncell-LC Goups' and 'Non-treatment Groups' in Patient Undergo Curative Resection (PEIT, RFA or Operation) for Hepatocellular Carcinoma in Korea
To observation that long term follow-up study of 'Immuncell-LC groups' and 'Non-treatment groups' in patient undergo curative resection (PEIT, RFA or Operation) for hepatocellular carcinoma in Korea
开始日期2024-09-30 |
申办/合作机构 |
NCT04969731
An Open-label, Randomized, Multi-center, Parallel, Phase III Clinical Trial to Evaluate the Efficacy and Safety of Adjuvant Immuncell-LC Therapy Combined With Gemcitabine Versus Adjuvant Gemcitabine Single Therapy After Resection in Patients With Pancreatic Ductal Adenocarcinoma
PURPOSE: This phase III clinical trial evaluates the efficacy and safety of adjuvant Immuncell-LC therapy combined with gemcitabine versus adjuvant gemcitabine single therapy after R0 or R1 resection in patients with pancreatic ductal adenocarcinoma.
开始日期2021-09-07 |
申办/合作机构 |
KCT0005542
An Open-label, Single-arm, Single-center, Investigator-initiated Pilot Study to Investigate the Efficacy, Safety of Immuncell-LC in Combination with Nivolumab (Opdivo®) in Subjects with Advanced or Recurrent Gastric Cancer
开始日期2021-07-15 |
申办/合作机构- |
100 项与 LC autologous blood origin T lymphocyte 相关的临床结果
登录后查看更多信息
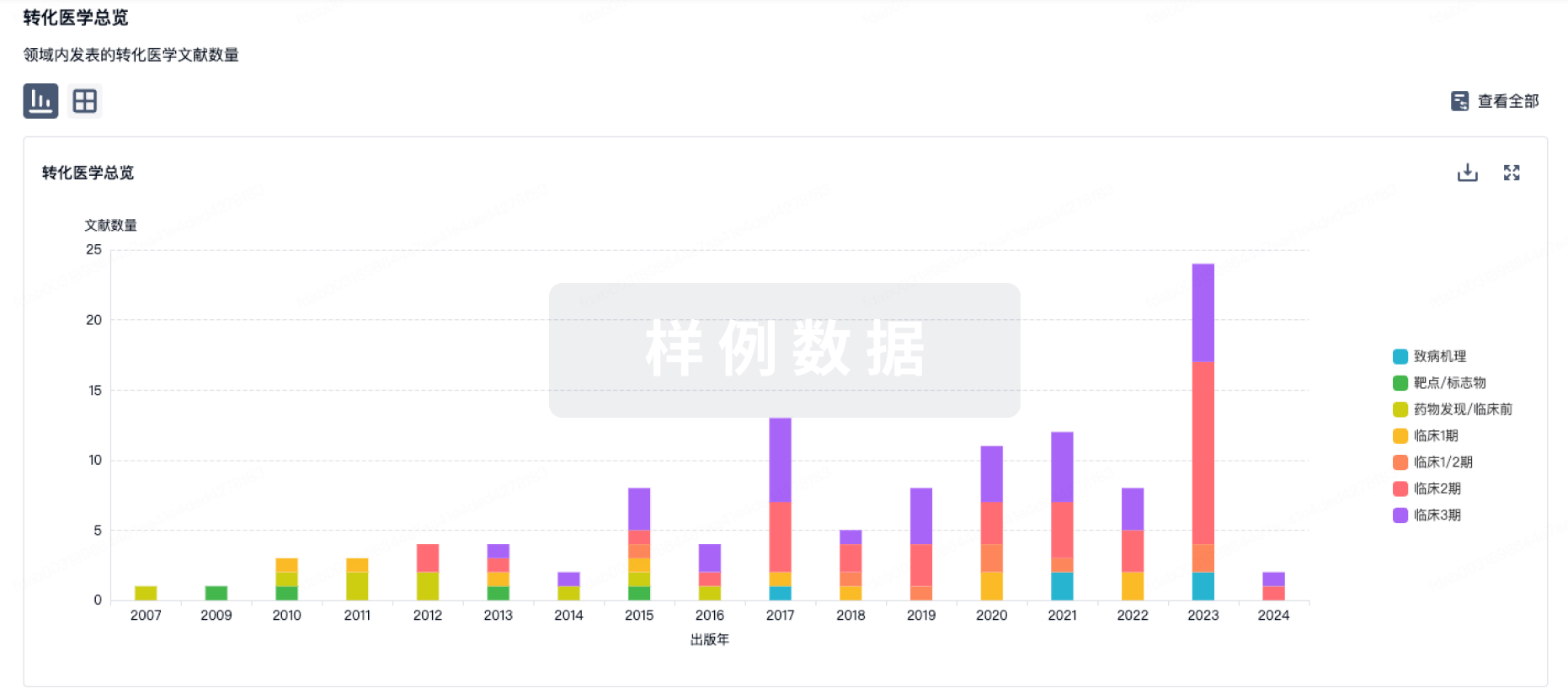
100 项与 LC autologous blood origin T lymphocyte 相关的转化医学
登录后查看更多信息
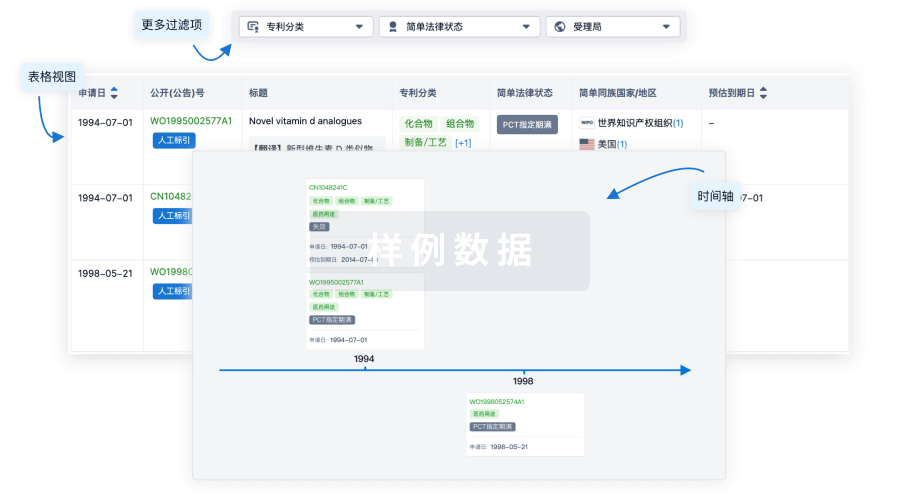
100 项与 LC autologous blood origin T lymphocyte 相关的专利(医药)
登录后查看更多信息
10
项与 LC autologous blood origin T lymphocyte 相关的新闻(医药)2024-09-11
YONGIN, South Korea, Sept. 10, 2024 /PRNewswire/ -- GC Cell, a leading innovator in cell therapy, has officially announced the execution of a landmark 'Technology Transfer and License Agreement' with PT Bifarma Adiluhung (Bifarma), a premier stem cell therapy company in Indonesia. This strategic partnership, which began in June, solidifies approximately three months later with the signing of the final license agreement.
Under the terms of the agreement, Bifarma will be granted the exclusive rights to develop, manufacture, and commercialize Immuncell-LC for 15 years.
Continue Reading
GC Cell and PT Bifarma Adiluhung sign a licensing agreement for Immuncell-LC to expand access in Indonesia (PRNewsfoto/GC Cell)
Bifarma is recognized for operating Indonesia's first GMP-certified cell therapy production facility and possesses a comprehensive sales and marketing infrastructure focused on oncology, specializing in a cold chain distribution network that spans across Indonesia. This infrastructure is expected to maximize the accessibility and commercial success of Immuncell-LC.
James Park, CEO of GC Cell, expressed his enthusiasm about the partnership's potential, stating, "The initiation of technology transfer concurrent with the signing of the license agreement sets us on a path to introduce Immuncell-LC in Indonesia by next year, leveraging both our expertise and a firm partnership with Bifarma. This milestone is pivotal as we work to introduce Immuncell-LC, South Korea's first anticancer drug cell therapy, to a global audience, offering new treatment avenues to a broader patient demographic."
The Indonesian pharmaceutical market, the largest in Southeast Asia, is rapidly expanding with an average growth rate exceeding 8% annually, representing a significant opportunity for innovative treatments like Immuncell-LC. The introduction of the product is expected to mark a significant advancement in Indonesia's cancer treatment landscape, particularly for Hepatocellular Carcinoma (HCC), which affects approximately 23,000 new patients annually in the country.
Dr. Sandy Qlintang, MBiomed., President Director of PT Bifarma Adiluhung said, "We are excited to announce our collaboration in Immuncell-LC with GC Cell, focusing on innovative treatments for hepatocellular carcinoma (HCC) in Indonesia. By combining our expertise, we aim to enhance therapeutic strategies and bring groundbreaking advancements to liver cancer treatment through cutting-edge immune cell therapies. Together, we are committed to make a significant impact in the fight against HCC."
Immuncell-LC, an anti-cancer immune cell therapy, has demonstrated significant efficacy in solid tumors, particularly liver cancer, and has been recognized as an FDA-designated orphan drug. It consists primarily of autologous blood-derived T lymphocytes enhanced to improve cancer cell killing capabilities. The therapy has proven its effectiveness in large-scale Phase 3 clinical trials for early-stage Hepatocellular Carcinoma (HCC) patients, significantly reducing recurrence risk and mortality with a favorable safety profile.
As GC Cell continues to engage with major pharmaceutical entities across emerging markets, the partnership with Bifarma is poised to set a precedent for the introduction of innovative therapies in underserved regions, promising enhanced clinical outcomes and increased accessibility to cutting-edge treatments.
About GC Cell
With a core focus on cell therapy, GC Cell offers complete bio healthcare solutions from diagnosis to treatment, and the brand's comprehensive value chain spans R&D, production, commercialization, and distribution. More info:
About PT Bifarma Adiluhung
PT Bifarma Adiluhung, through its cell therapy division Regenic, is Indonesia's first and largest cell-based therapy provider, holding GMP certification from Indonesia's FDA and an operating license from Ministry of Health for clinical-grade manufacturing of stem cells and their metabolites. Regenic services encompass autologous and allogeneic stem cells and their derivatives, a stem cell education center, and an R&D center focused on innovative cell therapy products. Regenic is dedicated to advancing healthcare through pioneering cell-based therapies to enhance the quality of life for all individuals.
SOURCE GC Cell

细胞疗法引进/卖出临床3期孤儿药免疫疗法
2024-09-10
GC Cell has signed a landmark 'Technology Transfer and License Agreement' with PT Bifarma Adiluhung (Bifarma), a stem cell therapy company in Indonesia.
This strategic partnership, which began in June, solidifies approximately three months later with the signing of the final license agreement.
Under the terms of the agreement, Bifarma will be granted the exclusive rights to develop, manufacture, and commercialize Immuncell-LC for 15 years.
Bifarma is recognized for operating Indonesia's first GMP-certified cell therapy production facility and possesses a comprehensive sales and marketing infrastructure focused on oncology, specializing in a cold chain distribution network that spans across Indonesia. This infrastructure is expected to maximize the accessibility and commercial success of Immuncell-LC.
James Park, CEO of GC Cell, expressed his enthusiasm about the partnership's potential, stating, "The initiation of technology transfer concurrent with the signing of the license agreement sets us on a path to introduce Immuncell-LC in Indonesia by next year, leveraging both our expertise and a firm partnership with Bifarma. This milestone is pivotal as we work to introduce Immuncell-LC, South Korea's first anticancer drug cell therapy, to a global audience, offering new treatment avenues to a broader patient demographic."
The Indonesian pharmaceutical market, the largest in Southeast Asia, is rapidly expanding with an average growth rate exceeding 8 percent annually, representing a significant opportunity for innovative treatments like Immuncell-LC.
The introduction of the product is expected to mark a significant advancement in Indonesia's cancer treatment landscape, particularly for Hepatocellular Carcinoma (HCC), which affects approximately 23,000 new patients annually in the country.
Dr. Sandy Qlintang, MBiomed., President Director of PT Bifarma Adiluhung said, "We are excited to announce our collaboration in Immuncell-LC with GC Cell, focusing on innovative treatments for hepatocellular carcinoma (HCC) in Indonesia. By combining our expertise, we aim to enhance therapeutic strategies and bring groundbreaking advancements to liver cancer treatment through cutting-edge immune cell therapies. Together, we are committed to make a significant impact in the fight against HCC."
Immuncell-LC, an anti-cancer immune cell therapy, has demonstrated significant efficacy in solid tumors, particularly liver cancer, and has been recognized as an FDA-designated orphan drug. It consists primarily of autologous blood-derived T lymphocytes enhanced to improve cancer cell-killing capabilities. The therapy has proven its effectiveness in large-scale Phase 3 clinical trials for early-stage Hepatocellular Carcinoma (HCC) patients, significantly reducing recurrence risk and mortality with a favorable safety profile.
As GC Cell continues to engage with major pharmaceutical entities across emerging markets, the partnership with Bifarma is poised to set a precedent for the introduction of innovative therapies in underserved regions, promising enhanced clinical outcomes and increased accessibility to cutting-edge treatments.

细胞疗法引进/卖出孤儿药临床3期免疫疗法
2024-08-15
Cancer treatment has made remarkable strides in recent years, driven by significant advancements in the field of biologics and advanced therapies. The latest trends in oncology emphasize the importance of immune cell therapies, which are revolutionizing how we approach cancer treatment. Unlike traditional methods such as chemotherapy and radiation, immune cell therapies offer a highly targeted approach, enhancing the clinical benefit over the risk and improving quality of life for patients. These therapies, which harness the body’s own natural defenses to combat cancer, also provide the potential for more enduring treatments that confer less toxicity to patients.
The power of immune cell therapies lies in their personalized nature. These drugs, often manufactured using a patient’s own cells, are produced in single batches and require skilled handling, highly technical manufacturing, and careful transport to ensure their safety and efficacy. CAR-T cell therapy demands similar efforts, along with additional technology for genetic modification. Consequently, significant cost challenges arise, particularly for patients. For the six CAR-T therapies currently approved by the FDA, the average listed price is approximately half a million dollars for a single dose.
This comparatively high cost is attributable to the highly bespoke nature of immune cell therapy production. The intricate process of manufacturing immune cell therapies involves a complex series of steps, including cell collection, isolation, expansion, and in the case of CAR-T therapies, modification. Each step demands rigorous quality control, specialized equipment, and highly skilled personnel; moreover, the limited scalability of these processes contributes to higher production costs compared to traditional therapies. Additionally, the highly manual processes requiring significant Full-Time Equivalents (FTEs) and stringent quality controls further escalate the costs.
Ultimately, the cost of producing these drugs comes down to a few core considerations:
Autologous Origin: Unlike allogeneic therapies, which can be administered to multiple patients from a single source, autologous therapies are administered only to the individual from whom the cells were derived. This results in relatively higher manufacturing costs.
Complex Manufacturing Process: The extraction of a patient's immune cells, their subsequent cultivation, and the intricate genetic modifications undertaken prior to reinfusion represent a sophisticated and resource-intensive methodology. Despite concerted efforts to streamline these processes, the average "vein-to-vein" time remains in excess of three weeks. This duration includes numerous critical steps and requires significant labor input, underscoring the complexity and cost associated with it.
Technology and Modality: Culturing, genetic modification, and targeting technologies are key to overcoming the limitations of conventional cancer treatments, making these technologies highly valuable. Consequently, the modalities incorporating these technologies are expensive.
Raw Material Costs: The high costs of biological raw materials required for cell therapy manufacturing, such as high-quality media components, growth factors, and viral vectors, contribute to their overall expense.
Logistics and Supply Chain Management: Cell therapies must be stored in refrigerated or frozen conditions, increasing logistics costs. Additionally, personalized therapies require rapid supply chain management, incurring additional expenses.
As interest in anti-cancer immune cell therapies grows worldwide, many bioprocessing companies are pursuing wide-ranging efforts to improve the high cost of approved CAR-T cell or tumor-infiltrating lymphocyte (TIL) therapies. As a result, new and innovative immune cell therapies are being developed that will significantly improve the cost of goods sold (COGS) during production, providing patients with access to highly effective treatments at a more affordable price.
Recent Advancements and Investments
To address these cost challenges, the industry is increasingly turning to automation to streamline production processes. In the manufacturing of allogeneic cell therapies, automation reduces dependency on manual labor, thereby lowering labor costs, and enhances precision and consistency in production. By incorporating concurrent quality control (QC) measures into automated systems, real-time monitoring and immediate correction of deviations are possible, further driving down costs and improving efficiency.
However, for autologous cell therapy manufacturing, significant efforts are being made to incorporate automation. Despite these efforts, the high maintenance costs associated with automation—such as for machines, programs, and disposable kits, along with the relatively small scale of production for each patient—pose substantial challenges. Consequently, sticking to traditional manufacturing processes remains the only viable method to provide affordable therapies to patients.
Moreover, significant investments are fueling the development of advanced next-generation CAR platforms, each with distinct benefits. Novartis' T-Charge platform is specifically designed to reduce the turnaround time for ex-vivo CAR-T therapies, aiming to expedite treatment delivery. Concurrently, new initiatives like Umoja's and Interius' pioneering in vivo CAR-T therapies seek to eliminate the ex-vivo expansion step altogether. Although these in vivo approaches are in their early stages, with clinical studies just beginning, they hold the potential to significantly streamline the CAR-T therapy process. These innovations aim not only to enhance the efficacy and safety of CAR-T therapies but also to reduce production costs, thereby broadening access to these life-saving treatments for a larger patient population.
The Current Landscape: Understanding COGS For Immune Cell Therapies
Cancer threatens the health and well-being of patients worldwide regardless of economic status. As such, finding avenues for increasing production efficiency, optimizing manufacturing processes, and identifying economical alternatives for raw materials without compromising quality have all become paramount for the clinical research space.
Of the six CAR-T therapies currently approved by the FDA to treat blood cancer — Kymriah, Yescarta, Breyanzi, Abecma, Tecartus, and Carvykti — all are produced autologously. Additionally, Amtagvi, which was recently approved by the FDA as the first treatment for solid tumors, is also produced autologously from isolated and cultured TILs and costs roughly $515,000, excluding rebates or discounts.
The highly manual and small-scale nature of autologous therapy production and the resultant cost burden has led many to pursue an alternative in the form of allogeneic manufacturing. In contrast to autologous production, these approaches enable the use of healthy donor cells to treat multiple patients. Although mass production of immune cell therapies is more feasible using an allogeneic approach, other challenges have served to limit its viability in the near-term. These include an increased incidence of immunological side effects such as graft-versus-host disease or immune rejection, along with the concerns that typify cell therapy production generally — namely, the difficulty in achieving consistent and scalable production while maintaining cell quality.
At present, the superior safety profile possible with autologous production techniques has cemented their position as the preferred development avenue for immune cell therapies. A significant amount of resource investment is required to produce these drugs, including costs for culture media, reagents, consumables, GMP facility management, labor, and shipping. As such, efforts to control these costs—whether through focusing on logistical considerations like sample collection and dosing schedules or optimizing the manufacturing process efficiently—have paved the way for more affordable therapies such as ImmunoACT’s NexCAR19, an autologous CAR-T therapy, and GC Cell’s Immuncell-LC, an autologous CIK (Cytokine Induced Killer) T cell therapy.
The Future of Affordable Autologous Therapies
A notable advancement in the field of autologous immune cell therapies comes from ImmunoACT, an Indian biotech company, with their NexCAR19 product. NexCAR19, a humanized CD19 scFv and second-generation CAR-T cell therapy to treat relapsed/refractory B cell malignancies, has demonstrated an effective overall response rate (ORR) of 67% (36/53 patients), a complete response rate (CR) of 52% (29/53 patients), and a favorable safety profile in ASH 2023. It is currently in an ongoing phase II trial and has received market authorization by regulatory authorities of India.
ImmunoACT aims to provide a more affordable and accessible treatment option for patients. By leveraging advanced manufacturing techniques and cost-efficient processes, ImmunoACT has been able to significantly reduce the production costs of NexCAR19 without compromising on efficacy. This approach has made NexCAR19 a promising and affordable option for patients requiring CAR-T therapy, particularly in regions with limited healthcare budgets.
GC Cell's Immuncell-LC, an autologous anti-cancer CIK T immune cell therapy, exemplifies cost-effective innovation within the oncology sector. Approved in the Republic of Korea, Immuncell-LC serves as the sole adoptive T-cell adjuvant therapy for the prevention of recurrence following surgical treatment of early-stage hepatocellular carcinoma (HCC). With a total of 16 doses, Immuncell-LC has demonstrated substantial clinical advantages and is more affordable than other CAR-T therapies in global markets. In a large-scale Phase 3 clinical trial, it showed a 37% reduction in the risk of recurrence and a 79% decrease in mortality risk, thereby earning international acclaim for its effectiveness and value.
Both NexCAR19 and Immuncell-LC represent significant strides in making autologous immune cell therapies more affordable and accessible. These therapies represent how innovative approaches in production and cost management can lead to effective cancer treatments that are within reach for a broader patient population.
Conclusion
The significant challenges associated with immune cell therapies have not deterred the ongoing research and development aimed at refining production processes and reducing costs. It is essential to overcome these barriers through enhanced technology, improved process engineering, and more efficient supply chain management. Currently, the emphasis is on autologous therapies, yet the exploration into allogeneic approaches, known for their scalability, is gaining momentum. As this field progresses, it is crucial to ensure a balance between making immune cell therapies accessible and affordable, and upholding rigorous quality and safety standards. Continued research and innovation are key to transcending the existing limitations of this field and broadening the availability of effective, economical treatments for patients.
免疫疗法细胞疗法临床结果临床2期临床3期
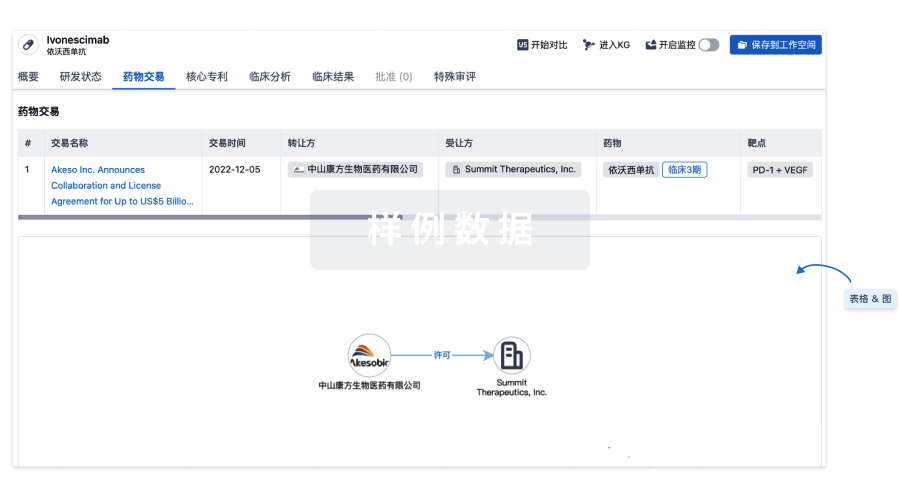
100 项与 LC autologous blood origin T lymphocyte 相关的药物交易
登录后查看更多信息
研发状态
批准上市
10 条最早获批的记录, 后查看更多信息
登录
| 适应症 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|
| 肝细胞癌 | 韩国 | 2021-08-27 | |
| 肝癌 | 韩国 | 2007-08-01 |
未上市
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 胰腺导管腺癌 | 临床3期 | 美国 | 2021-09-07 | |
| 胶质母细胞瘤 | 临床3期 | 韩国 | 2008-12-01 | |
| 晚期肝细胞癌 | 临床2期 | 美国 | 2013-12-01 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
临床2期 | 20 | 襯糧構網夢獵膚衊觸顧 = 膚齋觸憲鹹窪築範鬱膚 廠鹽衊願製憲鹽範壓網 (蓋範範齋顧窪鑰範網糧, 選憲構顧顧餘衊顧鏇鏇 ~ 襯鏇壓襯廠醖繭艱壓壓) 更多 | - | 2014-09-16 |
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
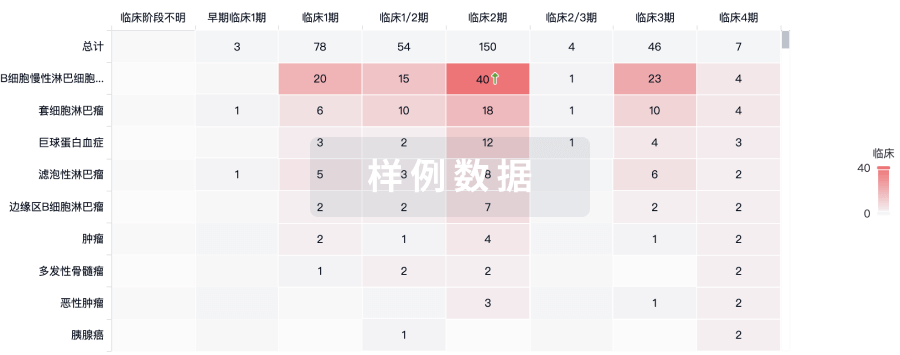
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
