预约演示
更新于:2025-05-07
Ecchymosis
瘀斑
更新于:2025-05-07
基本信息
别名 ECCHYMOSIS、Ecchymoses、Ecchymosis + [22] |
简介 Extravasation of blood into the skin, resulting in a nonelevated, rounded or irregular, blue or purplish patch, larger than a petechia. |
关联
5
项与 瘀斑 相关的药物靶点- |
作用机制- |
在研机构 |
原研机构 |
非在研适应症- |
最高研发阶段临床3期 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
靶点- |
作用机制- |
在研机构 |
原研机构 |
非在研适应症- |
最高研发阶段临床阶段不明 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
52
项与 瘀斑 相关的临床试验NCT06483204
Steroids for Rhinoplasty: Pain, Nausea, Edema and Ecchymosis
This study will be a prospective randomized study to evaluate the effect of medrol dosepaks (oral corticosteroids) on postoperative outcomes among patients undergoing rhinoplasty by Facial Plastic Surgeons at Vanderbilt. Outcomes will include postoperative pain, nausea, and patient experience, with secondary outcomes of swelling and bruising.
Methylprednisolone is an oral corticosteroid that has been shown in multiple RCTs and is used extensively that it can significantly reduce postoperative swelling and bruising in postoperative rhinoplasty patients, however, we have not examined if those effects extend to their pain ratings, nausea, and overall patient experience. Current research on use of steroids in rhinoplasty suggests that its use may decrease pain and nausea and benefit the patients overall experience.
Minimizing complications for any surgery is of upmost importance for surgeons.. However, the benefits of oral corticosteroid use for rhinoplasty patients in the immediate post-operative period are poorly understood and practice patterns vary widely. To identify and quantify the benefits and drawbacks of oral corticosteroid use in the immediate post-operative period for primary rhinoplasty patients, pain, swelling, nausea, patient experience, and post-operative swelling will be studied.
Methylprednisolone is an oral corticosteroid that has been shown in multiple RCTs and is used extensively that it can significantly reduce postoperative swelling and bruising in postoperative rhinoplasty patients, however, we have not examined if those effects extend to their pain ratings, nausea, and overall patient experience. Current research on use of steroids in rhinoplasty suggests that its use may decrease pain and nausea and benefit the patients overall experience.
Minimizing complications for any surgery is of upmost importance for surgeons.. However, the benefits of oral corticosteroid use for rhinoplasty patients in the immediate post-operative period are poorly understood and practice patterns vary widely. To identify and quantify the benefits and drawbacks of oral corticosteroid use in the immediate post-operative period for primary rhinoplasty patients, pain, swelling, nausea, patient experience, and post-operative swelling will be studied.
开始日期2025-04-01 |
NCT06840574
The Effect of Nutritional Supplementation on Actinic Purpura: a Pilot Study
Purpura is a macule or papule of blood in the skin. It is mostly seen in mature skin that is often prone to significant bruising. Small lesions of less than 5 mm are called petechiae and larger ones, found mostly in subcutaneous tissue, are called ecchymosis. Actinic purpura occurs almost exclusively in elderly populations. This single-blind randomized clinical trial evaluates the effect of an 8-week nutritional supplement intervention in comparison with isolated vitamin C supplements on actinic purpura in older adults. We will enroll thirty (30) otherwise healthy participants, both male and female, aged 55 years and older. Changes in participants' skin condition will be assessed at visit 1 (baseline), visit 2 (4-week), and visit 3 (8-week) using questionnaires, standard digital photography, and clinical grading of the skin lesions.
开始日期2025-03-01 |
申办/合作机构 |
NCT06450392
The Effect of Local and Systemic Tranexamic Acid on Edema and Ecchymosis in Orbital Surgery - a Prospective, Multicenter, Randomized, Double-blinded, Control Trial
Tranexamic acid is a synthetic reversible competitive inhibitor to plasminogen lysine receptor, which prevents plasmin formation and stabilizes the fibrin matrix, thus reducing bleeding. While recent studies have demonstrated the antifibrinolytic benefits of TXA in obstetric and gynecologic conditions, traumatic hemorrhage, cardiac surgery, total knee arthroplasty, and more, there is a paucity of clinical data on TXA use in plastic surgery. The aim of this study is to evaluate the effect of local and systemic TXA on postoperative periocular ecchymosis/edema in orbital surgery.
开始日期2024-10-07 |
申办/合作机构 |
100 项与 瘀斑 相关的临床结果
登录后查看更多信息
100 项与 瘀斑 相关的转化医学
登录后查看更多信息
0 项与 瘀斑 相关的专利(医药)
登录后查看更多信息
3,656
项与 瘀斑 相关的文献(医药)2025-05-01·Annals of Vascular Surgery
Efficacy and Safety of Endovenous Microwave Ablation Versus Endovenous Laser Ablation for Varicose Veins in Chronic Great Saphenous Vein Insufficiency: A Meta-Analysis
Review
作者: Aurora, Ruth Grace ; Dakota, Iwan ; Suwana, Averina Geffanie ; Adiarto, Suko ; Taofan ; Kalaij, Ayers Gilberth Ivano ; Zahrani, Sania ; Indriani, Suci ; Saputro, Keviano Bobby
2025-05-01·Journal of Plastic, Reconstructive & Aesthetic Surgery
Evaluation of the safety and efficacy of tranexamic acid use in face and neck lift surgery: A systematic review
Review
作者: Safran, Tyler ; ElAbd, Rawan ; Hiyzajie, Taliah ; Richa, Yasmina ; Gilardino, Mirko ; Pu, Lucy
2025-05-01·Journal of Vascular Surgery: Venous and Lymphatic Disorders
Continuation of anticoagulation through ambulatory phlebectomy does not impact postoperative bleeding risk
Article
作者: Wrana, Kristy ; Li, Ya-Huei ; Gallagher, James ; Gifford, Edward D ; Ayach, Mouhanad ; Cleary, Colin M ; Aitcheson, Elizabeth ; Orosco, Emily ; Davoudi, Kaveh ; Bailey, Allison ; Shah, Parth
67
项与 瘀斑 相关的新闻(医药)2025-04-30
·梅斯医学
今年48岁的赵先生,最近1个月总是感觉到腹痛,因腹痛加重来到医院就诊。肠镜发现直肠有隆起病变,可见一大小0.8*0.9cm隆起,表面光滑。经过行内镜下黏膜剥离术(ESD),病理确诊为神经内分泌肿瘤(NET,G1)。图1HE:肿瘤细胞排列呈巢状、条带状及小梁状分布,细胞大小较一致,圆形核和细腻的染色质。图2免疫组化:突触素(Syn)阳性。它离我们并不遥远神经内分泌肿瘤(neuroendocrine neoplasm,NEN)这是一类起源于肽能神经元和神经内分泌细胞的实体肿瘤。也许你对神经内分泌肿瘤一头雾水,不但没听说过,甚至会错误地认为神经和内分泌得了肿瘤?事实上,苹果前CEO乔布斯和知名演员赫本,也是因患上了这种罕见肿瘤去世的,神经内分泌肿瘤并不遥远。发病率明显上升神经内分泌瘤是罕见病,约占所有恶性肿瘤的2%左右,欧美人群的神经内分泌肿瘤的发病率大在2.5~5人/10万人,在过去30年内发病率增加了5倍,相比其他肿瘤,神经内分泌肿瘤发病率的增加更加迅速。国内外研究数据均提示,NENs的发病率在不断上升。美国流行病学调查结果显示,与其他类型肿瘤相比,NENs发病率上升趋势更为显著,在1973-2012年40年间,发病率增加了6.4倍,达到6.98/10万人年,亚洲人群中发病率约0.11~2.20 /10 万人年。遍布全身神经内分泌肿瘤(neuroendocrine neoplasm,NEN)从字面上就可以大概知道,这是一类起源于肽能神经元和神经内分泌细胞的实体肿瘤。由于神经内分泌细胞遍布全身各处,特别是广泛分布于消化系统和呼吸系统,所以可发生在除指甲趾甲、毛发除外的体内任何部位,最常见的是胃、肠、胰腺等消化系统神经内分泌肿瘤(约占所有神经内分泌肿瘤的2/3,60%-70%左右),其次是肺支气管神经内分泌肿瘤(约20%-30%左右),另有少数发生在肾上腺、胸腺、甲状腺等部位。根据WHO(世界卫生组织) 整体命名方案,所有来自于神经内分泌细胞和组织发生的肿瘤,都命名为神经内分泌肿瘤。而神经内分泌肿瘤中99%都是恶性,可能发生的区域几乎涵盖了所有的器官。从神经系统里面的垂体、内分泌器官的甲状腺、甲状旁腺到胰腺中的胰岛、消化道中的内分泌细胞等都被纳入进神经内分泌肿瘤的概念中。这些神经内分泌肿瘤只有当恶性程度非常高、分化非常差的时候才命名为“神经内分泌癌”。而分化较好的一部分,仍然以“神经内分泌肿瘤”来命名。这一部分分化较好的瘤又会根据增殖的情况来分级,分成G1、G2甚至G3。但它们仍然还是属于恶性肿瘤的范畴。临床表现多样由于肽能神经元和神经内分泌细胞可合成、分泌、储存多种生物活性胺、小分子多肽或激素等,所以产生各种千奇百怪的多样化的症状表现,常不典型。患者主要表现为压迫症状、神经内分泌症状和转移引起症状。症状轻时无明显症状,重时可出现代谢紊乱,甚至危及生命。(一)典型症状神经内分泌肿瘤的典型症状可分为压迫症状、神经内分泌症状和转移引起症状三大类。1、压迫症状(1)局部肿块:肿瘤生长较大可在原发灶或转移灶触及肿块。(2)非特异性消化道症状(消化道肿瘤):腹痛、恶心、呕吐、黄疽、肠梗阻、消化道出血等。(3)非特异性呼吸系统症状(呼吸道肿瘤):咳嗽、咳痰、吞咽困难(压迫食道)气促、呼吸困难(压迫支气管)等。(4)非特异性泌尿道症状:排尿困难、无痛性肉眼尿血等。(5)垂体压迫症状:表现为头痛、视物模糊、视野缺损、失明等。2、神经内分泌症状(1)卓-艾综合征(2)惠普尔(Wipple)三联征(3)库欣综合征(4)肌无力综合征(5)抗利尿激素分泌异常综合征(6)醛固酮增多症3、转移症状(1)脑转移:头晕头痛、呕心呕吐、癫痫、肢体运动障碍等。(2)肝转移:黄疸、腹水、全身瘀点、瘀斑等。(3)肺转移:咳嗽、咳痰、气促、呼吸困难等。(4)骨转移:骨转移部位疼痛、病理性骨折等。(二)部分类型肿瘤典型症状1、胰高血糖素瘤:游走性坏死性红斑、糖耐量受损、体重下降等。2、生长抑素瘤:糖尿病和/或低血糖、胆石症、脂肪性腹泻等。3、血管活性肠肽瘤:严重水样腹泻、脱水、低钾血症、胃酸缺乏或胃酸过少。4、Ⅰ型胃神经内分泌瘤:表现为自身免疫性萎缩性胃炎,胃酸缺乏、缺铁性或巨幼红细胞性贫血,胃镜下可见黏膜下多发息肉或黏膜肿物。5、Ⅱ型胃神经内分泌瘤:胃底体黏膜广泛肥厚、水肿、溃疡及糜烂,多发性消化道溃疡。(三)其他症状1、神经系统病变小脑皮质变性、周围神经病(感觉或运动)、肌无力等神经系统病变,肿瘤经治疗后消失或缓解时,其肌无力症状也随之缓解。2、黑棘皮病3、皮肌炎4、骨关节增生5、弥散性血管内凝血6、皮肤色素沉着7、性激素分泌异常8、生长激素分泌异常9、促甲状腺激素分泌异常诊断根据相应的临床表现,肿瘤标记物检测,影像学检查及病理学检查进行神经内分泌肿瘤的诊断。完整的诊断内容包括肿瘤部位、分级、分期以及功能状态。胃肠胰是NEN最常发生的部位,约占所有NEN的55%-70%。胃肠胰NEN的诊断是基于临床症状、激素水平、各种影像学检查以及组织病理学证实。应采取实验室检查、定位诊断的方法明确,确诊依靠或组织检查或手术组织病理检查。实验室检查:CgA、肽类激素测定、激发实验定位诊断:CT、MRI、SSRS病理检查:细针穿刺、活组织检查、术后病理诊断按照肿瘤的增殖活性将胃肠胰神经内分泌肿瘤分级为:G1、G2、G3。治疗神经内分泌肿瘤的治疗方式多样,包括内镜、外科、内科、核素、介入、化疗、中医、姑息治疗和心理治疗,多学科整合诊疗可以给予患者个体化的治疗方案。选择何种治疗手段,取决于肿瘤的分级、分期、发生部位以及是否具有分泌激素的功能。参考资料1、毛歆歆,陈杰 2022版WHO神经内分泌肿瘤分类解读 中华病理学杂志, 2024,53(7) : 655-659.2、中国临床肿瘤学会神经内分泌肿瘤专家委员会 中国胃肠神经内分泌肿瘤专家共识(2019年版)3、陈旻湖等,消化病学,人民卫生出版社,第一版,2019:930~9434、李洁等,胰腺和胃肠道来源神经内分泌肿瘤分类-2018 ARC/WHO分类框架共识解读,肿瘤综合治疗电子杂志,2018,4(4):16~205、中国抗癌协会神经内分泌肿瘤整合诊治指南 中国肿瘤临床来源 | 梅斯医学编辑 | 素碧神经系统罕见病交流群↓点击下方“阅读原文”,下载梅斯医学APP吧!
2025-04-08
·梅斯医学
29岁的白领苏晴(化名)最近一年体重飙升30斤,即便每天只吃沙拉、喝凉水,腰腹仍像“吹气球”般膨胀。更诡异的是,她的脸变得圆如满月,后背隆起“水牛包”,皮肤薄得像纸,轻轻一碰就淤青,大腿内侧还爬满紫红色裂纹。同事调侃她“怀孕了”,体检医生却查出高血压(160/100mmHg)、血糖飙升,最终转诊至内分泌科。接诊医师为苏晴进行了详细的检查,结果显示:皮质醇节律消失:8AM血皮质醇620nmol/L(正常138-635),12PM 580nmol/L(正常<275);小剂量地塞米松抑制试验失败(皮质醇未被抑制);垂体MRI:垂体左侧微腺瘤(直径4mm)。经过综合分析最终确诊为库欣病。女性发病率是男性的5-10倍库欣病(Cushing disease)由分泌促肾上腺皮质激素(adrenocorticotropic hormone, ACTH)的垂体腺瘤引起,可致高皮质醇血症,是内源性库欣综合征的最常见病因(60%~80%) 。库欣病占垂体肿瘤的15%,大多数为微腺瘤(直径<10 mm),多数直径<6 mm;近10%为大腺瘤,可表现为侵袭性,向鞍外扩展或浸润。系统性回顾分析显示,库欣病的汇总患病率为22例/百万人,年发病率为0.24/10万。国内尚缺乏大规模流行病学数据。成人库欣病的诊断年龄为40~60岁,女性发病率是男性的5~10倍。临床表现库欣综合征临床表型多样,多为非特异性,如肥胖、糖尿病、高血压、月经紊乱、抑郁等。典型症状包括满月脸、水牛背、向心性肥胖、皮肤紫纹、多血质、近端肌无力、脆性骨折、非创伤性皮肤瘀斑、与年龄不相符的骨质疏松等;儿童常伴有生长发育停滞。当临床表现典型时,库欣综合征易被诊断,而轻症者的临床表现往往与代谢疾病存在重叠,诊断存在一定难度。库欣病临床表现呈一定的年龄异质性。年轻患者更易出现生殖系统受累、皮肤异常、多毛和抑郁状态,而年长患者的心血管疾病、血管栓塞事件、肌无力和骨质疏松发生率更高。与肾上腺库欣综合征相比,性欲减退、月经紊乱和多毛在库欣病中更多见,可能与高皮质醇水平对下丘脑促性腺激素释放激素分泌的抑制及肾上腺雄激素分泌增加有关。筛查与诊断一、库欣综合征的筛查1.出现与年龄不符的症状者,如高血压和骨质疏松等。2.出现多种和进行性发展的典型症状提示库欣综合征可能者,如肌病、多血质、紫纹、瘀斑、皮肤菲薄。3.身高百分位数减低而体重增加的儿童。4.合并肾上腺意外瘤者。对疑诊人群进行评估前需了解有无外源性糖皮质激素的应用史,包括口服、直肠用、吸入、外用或注射剂,尤其是含有糖皮质激素的外用软膏、中药甘草和关节腔内或神经髓鞘内注射剂等,以排除医源性库欣综合征。二、库欣综合征的定性诊断对疑诊人群,推荐进行24 h尿游离皮质醇、午夜血或唾液皮质醇、1 mg地塞米松抑制试验或小剂量地塞米松抑制试验(2 mg/d×48 h)检查。建议至少进行上述2项及以上筛查试验,如结果异常则高度怀疑库欣综合征,需要进行下一步定性和定位检查( 图1 )。除上述检查指标外,还应关注其他垂体肾上腺激素评估,包括甲状腺功能、性激素、生长激素等。治疗治疗目标包括治疗原发病、实现皮质醇水平正常化、缓解体征和临床症状、治疗相关合并症、保护垂体功能、提高生活质量。1.药物治疗药物治疗可通过控制下丘脑-垂体的ACTH合成和分泌、抑制肾上腺糖皮质激素的合成和分泌,以及阻断外周糖皮质激素的效应等来发挥作用,可作为控制高皮质醇血症的有效选择。随着有前景药物引入和新药靶点开发,药物治疗的地位不断提升。2.手术治疗2.1 经蝶窦垂体手术被推荐为大多数库欣病的一线治疗方法。手术缓解率为65%~90%,术后疾病持续活动状态为3.4%~35.0%。2.2 肾上腺切除术双侧肾上腺切除术通常作为所有其他方案都失败后的最后治疗手段。对于严重高皮质醇血症患者,往往需要快速有效降低皮质醇,以避免病情失控造成长期的全身性影响,双侧肾上腺切除术可能更有必要。2.3放射治疗适用人群:术后疾病持续或复发状态或侵袭性肿瘤的辅助治疗。对于手术高风险或拒绝手术患者,也可作为主要治疗方法。参考文献:1. 中华医学会内分泌学分会. 库欣病诊治专家共识(2025). 中华内分泌代谢杂志,2025,41(03):186-197.2.李娇娇,王嘉熙,奚悦.库欣病的1例报告[J].锦州医科大学学报,2021,42(03):110-113.DOI:10.13847/j.cnki.lnmu.2021.03.024.来源 | 梅斯医学编辑 | wanny神经系统罕见病交流群↓点击下方“阅读原文”,下载梅斯医学APP吧!
诊断试剂
2025-04-07
·生物探索
引言巨细胞动脉炎 (Giant-cell arteritis, GCA)是一种挺“偏爱”咱们长辈的血管炎症性疾病,常常带来恼人的头痛、视力模糊甚至失明的风险。一直以来,治疗这种病主要依赖糖皮质激素 (glucocorticoids),也就是我们常说的“激素”。激素效果虽好,但长期使用带来的副作用和停药后疾病容易复发的问题,一直是医生和患者心头的一块大石。不过,4月2日发表在国际顶级医学期刊《The New England Journal of Medicine》上的一项重磅研究“A Phase 3 Trial of Upadacitinib for Giant-Cell Arteritis” (SELECT-GCA III期临床试验),似乎为GCA患者带来了一缕新的曙光!这项研究聚焦于一种名为“乌帕替尼 (Upadacitinib)”的口服药物,它在治疗GCA方面展现出了令人鼓舞的效果,特别是在帮助患者减少激素用量、实现长期病情稳定方面。这到底是一款什么样的“神药”?它真的能帮助GCA患者摆脱对激素的长期依赖吗?它的效果和安全性如何? “老年专属”的血管“火焰”—— 巨细胞动脉炎 (GCA) 究竟是什么?在我们深入了解新疗法之前,有必要先认识一下巨细胞动脉炎 (GCA)。这可不是普通的炎症,它是一种主要攻击我们身体里大、中型动脉血管的“系统性血管炎 (systemic vasculitis)”。想象一下,我们身体里的血管就像是输送血液和氧气的管道,如果这些管道因为炎症而变得狭窄、堵塞甚至受损,那后果可是相当严重的。GCA有个很显著的特点,那就是它几乎“专挑”50岁以上的人群下手,发病高峰更是在70岁以后,而且女性患者比男性更为常见。根据全球范围的统计,在50岁以上的人群中,每10万人里大约就有51位GCA患者,是成年人中最常见的原发性血管炎。那么,GCA具体会引起哪些不适呢?它的症状多种多样,最常见的包括:顽固性头痛:常常是新出现的、局限在一侧或双侧头部的疼痛,尤其是在太阳穴(颞部)附近。头皮或颞部触痛:轻轻触摸头皮或太阳穴区域,就会感到明显的疼痛。下颌“跛行” (jaw claudication):咀嚼食物时,下巴肌肉会感到疲劳和疼痛,需要停下来休息一会儿才能继续。这就像走路多了腿会酸痛一样,是血管供血不足的表现。视力障碍:这是GCA最令人担忧的并发症!可能出现视力模糊、复视(看东西重影),甚至突然的、永久性的失明。这是因为眼部血管受累,导致视神经缺血。其他缺血性并发症:比如可能导致中风等。伴随风湿性多肌痛 (Polymyalgia rheumatica, PMR):很多GCA患者同时或先后出现PMR的症状,表现为颈部、肩部、上臂、臀部和大腿的肌肉疼痛和僵硬,尤其在早晨起床时最为明显。可以说,GCA不仅影响生活质量,严重时甚至可能致残(尤其是失明)。因此,找到有效且安全的治疗方法,对于改善患者预后至关重要。甜蜜的“负担”—— 激素治疗的两难困境谈到GCA的治疗,糖皮质激素 (glucocorticoids) 是绕不开的话题。几十年来,它一直是治疗GCA的“基石”和主要武器。激素能够快速、有效地抑制血管的炎症反应,缓解头痛、肌肉疼痛等症状,更重要的是,能显著降低失明等严重并发症的风险。可以说,在GCA的急性期,激素是当之无愧的“救火队员”。然而,凡事有利有弊。激素这把“双刃剑”,在斩断炎症的同时,也可能给患者带来沉重的“负担”。长期、大剂量地使用激素,会带来一系列副作用,可能影响到身体的方方面面:代谢紊乱:引起血糖升高(甚至诱发糖尿病)、血脂异常、体重增加、水牛背、满月脸等库欣综合征表现。骨骼问题:导致骨质疏松,增加骨折风险。免疫力下降:增加感染的风险,让普通的感冒也可能变得麻烦。心血管问题:可能导致血压升高。皮肤问题:皮肤变薄、出现瘀斑、痤疮等。精神影响:可能引起情绪波动、失眠,甚至更严重的精神症状。更令人头疼的是,GCA是一种慢性、易复发的疾病。虽然初始剂量的激素效果显著,但医生通常会尝试逐渐减少激素用量(即“减量”),以期用最小有效剂量来控制病情,减少副作用。可现实往往很骨感——研究显示,大约有50%到80%的GCA患者在激素减量过程中或停药后,会出现疾病复发 (disease flare)!这意味着症状卷土重来,患者不得不重新加大激素剂量,再次陷入“有效-副作用-减量-复发”的循环中。目前,虽然已经有一款名为托珠单抗 (tocilizumab) 的白细胞介素-6受体抑制剂 (interleukin-6 receptor inhibitor) 被批准用于治疗GCA,为部分患者提供了新选择,但它并非适用于所有患者,且价格昂贵,仍有相当一部分患者亟需更有效、更安全的“激素替代”或“激素节约”疗法。寻找能够让患者在减少甚至摆脱激素的同时,又能有效控制病情、防止复发的治疗方案,成为了GCA领域一个亟待解决的“痛点”。精准“断电”—— 乌帕替尼如何从源头阻击炎症?面对激素治疗的困境和患者的迫切需求,研究人员将目光投向了炎症发生的更深层机制。研究发现,在GCA的发病过程中,一些特定的“信号兵”——也就是细胞因子 (cytokines) 扮演了关键角色,它们像是在血管壁上“煽风点火”,驱动着炎症的发生和发展。其中,两位“主犯”就是白细胞介素-6 (interleukin-6, IL-6) 和 干扰素-γ (interferon-gamma, IFN-γ)。有趣的是,这些炎症“信号兵”要发挥作用,需要通过“JAK-STAT”的信号通路 (Janus kinase-signal transducer and activator of transcription pathway) 来传递信息。你可以把JAK想象成一个关键的“信号开关”。如果能找到一种方法把这个“开关”关掉,是不是就能有效阻止炎症信号的传递,从而控制GCA的病情呢?这正是乌帕替尼 (Upadacitinib) 的设计思路!乌帕替尼是一种口服的、选择性的JAK抑制剂 (Janus kinase inhibitor),它能比较精准地作用于JAK家族中的JAK1亚型。通过抑制JAK1的功能,乌帕替尼能够有效阻断包括IL-6和IFN-γ在内的多种与GCA发病相关细胞因子的信号传导,从源头上控制炎症。由于这种精准的作用机制,乌帕替尼已经在多种自身免疫性疾病(如类风湿关节炎、银屑病关节炎、溃疡性结肠炎等)的治疗中显示出良好的疗效和安全性,并获得了批准。那么,它在GCA这个同样由免疫系统“误伤”自身血管引发的疾病中,表现又会如何呢?这正是SELECT-GCA研究想要回答的核心问题。严格的“大考”—— SELECT-GCA 试验设计一项新药是否有效、安全,不能凭空想象,必须经过严格的临床试验来验证。SELECT-GCA研究就是这样一场针对乌帕替尼治疗GCA的III期“大考”。这场“考试”在全球24个国家的100个研究中心进行,可谓规模宏大、设计严谨。研究者们招募了428位年满50周岁、确诊为GCA(通过颞动脉活检或影像学检查证实)并且在研究开始前8周内病情处于活动期的患者。这些患者中,有些是刚刚确诊的“新发病例 (new-onset disease)” (约占70%),有些则是之前治疗效果不佳或激素减量后复发的“复发病例 (relapsing disease)” (约占30%)。所有患者在入组前都接受过每日至少40mg泼尼松(或等效激素)的治疗,入组时正在接受每日20-60mg的泼尼松治疗。然后,这些患者被随机分入三个不同的治疗组,比例为2:1:1:乌帕替尼15mg组 (n=209):每天口服一次15mg乌帕替尼,同时配合一个为期26周的激素逐渐减停方案。乌帕替尼7.5mg组 (n=107):每天口服一次7.5mg乌帕替尼,同样配合一个为期26周的激素逐渐减停方案。安慰剂组 (n=112):每天口服一次外观与乌帕替尼无异但没有活性成分的安慰剂 (placebo),同时配合一个相对缓慢的、为期52周的激素逐渐减停方案。研究的主要终点是:在治疗第52周时,达到“持续缓解 (sustained remission)”状态的患者比例。这里的“持续缓解”有严格定义:从治疗第12周开始一直到第52周,患者都没有出现任何GCA的症状或体征,并且严格遵守了预设的激素减量方案(没有因为病情反复而增加激素用量)。除了这个主要问题,研究还设置了多个次要终点,包括:持续完全缓解(不仅没症状,炎症指标如红细胞沉降率 ESR 和 C反应蛋白 CRP 也恢复正常)、疾病复发情况、累积激素使用总量、患者自我报告的疲劳程度和生活质量改善情况等等。成绩斐然!15mg乌帕替尼显著提高持续缓解率经过长达52周的严谨观察和数据收集,SELECT-GCA研究的主要结果终于揭晓,而成绩单确实令人振奋,特别是对于15mg剂量的乌帕替尼!我们来看最重要的主要终点——在第52周时达到持续缓解 (sustained remission)的患者比例:在接受乌帕替尼15mg + 26周激素减停方案的患者中,有46.4%的人达到了持续缓解状态。相比之下,在接受安慰剂 + 52周激素减停方案的患者中,只有29.0%的人达到了持续缓解。这个差异(46.4% vs 29.0%)在统计学上是显著的 (P=0.002),这意味着服用15mg乌帕替尼的患者,在更快减少激素的情况下,实现长期病情稳定的可能性,要显著高于仅接受标准激素治疗(配合安慰剂)的患者。简单来说,15mg乌帕替尼组的持续缓解率几乎是安慰剂组的1.6倍!那么,7.5mg剂量的乌帕替尼表现如何呢?研究结果显示,7.5mg组的持续缓解率为41.1%。虽然这个数字看起来也高于安慰剂组的29.0%,但经过严格的统计学检验,这个差异并未达到预设的显著性标准。这表明,在这个研究中,只有15mg剂量的乌帕替尼显示出优于安慰剂的明确疗效。研究者们还考察了一个更严格的疗效指标——持续完全缓解 (sustained complete remission),即不仅没有临床症状,连血液中的炎症指标(ESR和CRP)也从第12周到第52周持续保持正常。在这个更严格的标准下,15mg乌帕替尼的优势更加明显:乌帕替尼15mg组达到持续完全缓解的比例为37.1%。安慰剂组仅为16.1%。这个差异同样具有高度统计学意义 (P<0.001)。这意味着,超过三分之一服用15mg乌帕替尼的患者,不仅临床症状消失,连体内的炎症反应也得到了持续、深度的控制,而安慰剂组只有不到六分之一能达到这个理想状态。这些核心数据有力地证明了,每日一次口服15mg乌帕替尼,配合一个26周激素减停方案,在诱导和维持GCA患者病情缓解方面,显著优于传统的、更缓慢的激素减停方案(配合安慰剂)。 这无疑为GCA的治疗带来了新的希望。不止缓解!更少激素、更少复发、生活质量up up!SELECT-GCA研究的惊喜还不止于此!除了核心的缓解率数据,研究还揭示了15mg乌帕替尼在其他几个对患者至关重要的方面也表现出色,真正体现了“激素节约”和改善生活质量的潜力。1. 大幅减少激素总用量:跟“激素负担”说拜拜?这是许多患者和医生都极为关注的一点。研究精确计算了患者在52周内累积使用的激素总量(以泼尼松等效剂量计算)。结果显示:乌帕替尼15mg组的中位累积激素剂量为1615毫克。安慰剂组的中位累积激素剂量则高达2882毫克。这个差距是巨大的,并且统计学上显著 (P<0.001)。这意味着,接受15mg乌帕替尼治疗的患者,在一年内所需的激素总量几乎减少了近一半 (约44%)!这直接关系到患者长期承受激素副作用的风险大大降低。更有意思的是一项事后分析 (post hoc analysis) 数据:研究者们考察了在52周试验完成的患者中,有多少人需要用到超出原定减量计划的“额外”激素(通常是因为病情反复)。结果发现:15mg乌帕替尼组中,需要额外使用的激素中位数仅为20毫克(95%CI为0-40毫克)。而安慰剂组中,这个数字飙升至512.5毫克(95%CI为35-1109毫克)!这更加直观地说明,15mg乌帕替尼不仅让患者遵循了更快速的激素减停计划,而且在整个过程中,他们因为病情波动而需要“临时加药”的情况也显著减少。2. 有效降低疾病复发风险:让病情“稳”下来!GCA患者最怕的就是病情反复发作 (disease flare)。研究追踪了患者在52周内首次出现疾病复发的时间以及发生复发的总人数:与安慰剂组相比,15mg乌帕替尼组发生首次疾病复发的时间显著推迟。在52周内,经历至少一次疾病复发的患者比例:乌帕替尼15mg组为34.3%。安慰剂组为55.6%。这个差异同样显著 (P=0.001)。也就是说,服用15mg乌帕替尼将患者在一年内经历疾病复发的风险降低了大约38% (风险比 Hazard Ratio 约为0.57-0.62,具体取决于计算方式)。更少的复发意味着更稳定的病情,更少需要调整治疗方案,患者的生活也能更加安心。3. 改善生活质量:告别疲劳,拥抱活力!疾病本身以及长期治疗(尤其是激素)常常让患者感到疲惫不堪,生活质量大打折扣。研究通过标准化的问卷(如FACIT-疲劳量表、SF-36健康调查问卷的生理功能部分)评估了患者的感受:结果显示,与安慰剂组相比,接受15mg乌帕替尼治疗的患者,在减轻疲劳感方面有显著改善 (P=0.004)。同时,他们的整体生理健康状况(反映在SF-36 PCS得分上)也得到了显著提升 (P=0.002)。这意味着,15mg乌帕替尼不仅控制了疾病的客观指标,也实实在在地改善了患者的主观感受和日常生活能力。综合来看,15mg乌帕替尼带来的好处是全方位的:它不仅能更有效地让病情达到并维持缓解状态,还能显著减少患者对激素的依赖、降低疾病复发的风险,并改善患者的疲劳感和整体生活质量。这对于长期被GCA和激素副作用困扰的患者来说,无疑是一个巨大的福音。安全性警报解除?大家关心的副作用问题谈及新药,尤其是像JAK抑制剂这类免疫调节药物,大家最关心的问题之一就是:它安全吗?会不会带来新的风险?SELECT-GCA研究同样对乌帕替尼的安全性进行了密切监测和评估。总体来看,在长达52周的治疗期内,乌帕替尼组(包括7.5mg和15mg)的整体安全性特征与安慰剂组相似。也就是说,并没有观察到因为使用了乌帕替尼而导致不良事件发生率显著增加的情况。值得一提的是,JAK抑制剂这类药物,既往研究曾提示可能与一些特定的安全风险相关,比如主要不良心血管事件 (Major Adverse Cardiovascular Events, MACE)(如心肌梗死、中风等)和血栓事件。考虑到GCA患者本身就是心血管疾病的高风险人群(因为年龄较大),这一点尤其引人关注。然而,在SELECT-GCA这项研究中,结果令人安心:在整个52周的治疗期间,接受乌帕替尼治疗的两个组(7.5mg和15mg)中,均未发生任何主要不良心血管事件 (MACE)。当然,这只是一个临床试验的结果,还需要在更大人群和更长时间的真实世界应用中持续观察,但至少在这个研究中,乌帕替尼并未显示出增加心血管风险的信号。此外,研究还观察到一些有趣的现象:因不良事件而提前停药的患者比例,反而是安慰剂组最高 (20.5%),而乌帕替尼7.5mg组为16.8%,15mg组最低 (15.3%)。因疗效不佳而提前停药的患者比例,也是安慰剂组最高 (7.1%),而乌帕替尼7.5mg组为3.7%,15mg组为3.3%。这些数据从侧面反映了,15mg乌帕替尼不仅疗效更好,其整体耐受性也可能优于长期、较高剂量的激素治疗方案(安慰剂组实质上是接受更长时间、可能更高累积剂量的激素治疗)。当然,任何药物都有可能发生副作用,乌帕替尼也不例外。研究中也报告了一些常见的不良事件,但总体发生率在各组间没有显著差异,或者在乌帕替尼组并未显示出明确的风险升高。具体的副作用谱还需要参考更详细的药物说明和医生的专业评估。总而言之,基于SELECT-GCA研究在52周的数据,15mg乌帕替尼在治疗GCA时展现了良好的安全性特征,特别是在备受关注的心血管风险方面,未观察到警示信号。 其整体耐受性似乎不劣于甚至可能优于传统的长程激素疗法。迈向GCA治疗新纪元的一大步总的来说,这项发表在《新英格兰医学杂志》上的研究结果,为巨细胞动脉炎 (GCA) 的治疗带来了令人兴奋的进展。研究明确显示:每日一次口服15mg乌帕替尼 (Upadacitinib),配合一个26周糖皮质激素减停方案,在实现并维持GCA患者病情缓解(包括持续缓解和持续完全缓解)方面,显著优于传统的、依赖更长周期(52周)激素减停的安慰剂方案。更重要的是,这种疗法不仅效果显著,还带来了多重获益:显著减少了患者对激素的总需求量,有望降低长期激素副作用的风险。有效降低了疾病复发的风险,让病情更加稳定持久。显著改善了患者的疲劳感和整体生活质量。在为期52周的研究中,展现了良好的安全性,未观察到主要不良心血管事件的发生。虽然7.5mg剂量未能在此次研究中证明其优效性,但15mg乌帕替尼的成功,无疑为GCA患者,特别是那些对现有治疗反应不佳、激素依赖严重或无法耐受激素副作用的患者,提供了一个极具潜力的新治疗选择。当然,我们需要记住,这仍是一项临床研究的结果。乌帕替尼是否以及何时会在全球范围内被批准用于GCA的治疗,还需要等待监管机构的审评。并且,任何治疗决策都需要在专业医生的指导下,结合患者的具体情况(如病史、合并症、个人意愿等)来制定。但无论如何,SELECT-GCA研究的成果是GCA治疗领域向前迈出的重要一步。它不仅验证了一种新型JAK抑制剂在GCA中的价值,更重要的是,它让我们看到了未来GCA治疗可能的新方向——更有效、更安全、更少依赖激素,最终帮助患者重获更高质量的生活。让我们共同期待这一领域未来更多的突破!参考文献Blockmans D, Penn SK, Setty AR, Schmidt WA, Rubbert-Roth A, Hauge EM, Keen HI, Ishii T, Khalidi N, Dejaco C, Cid MC, Hellmich B, Liu M, Zhao W, Lagunes I, Romero AB, Wung PK, Merkel PA; SELECT-GCA Study Group. A Phase 3 Trial of Upadacitinib for Giant-Cell Arteritis. N Engl J Med. 2025 Apr 2. doi: 10.1056/NEJMoa2413449. Epub ahead of print. PMID: 40174237.责编|探索君排版|探索君转载请注明来源于【生物探索】声明:本文仅用于分享,不代表平台立场,如涉及版权等问题,请尽快联系我们,我们第一时间更正,谢谢!End往期精选围观Nature | 靶向线粒体VDAC2:破解实体瘤免疫治疗抵抗的"死亡密钥"热文Nature Medicine | 多囊女性子宫内膜藏着什么秘密?——全球首份单细胞图谱揭示治疗新方向热文Nature | 颠覆认知!大脑学习的惊人秘密:你的“潜伏知识”是如何瞬间爆发的?热文Cell | 颠覆认知!染色体形成并非依赖“骨架”,自组织模型重塑教科书热文Science | 为什么我们回想不起三岁前的经历?
临床结果
分析
对领域进行一次全面的分析。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
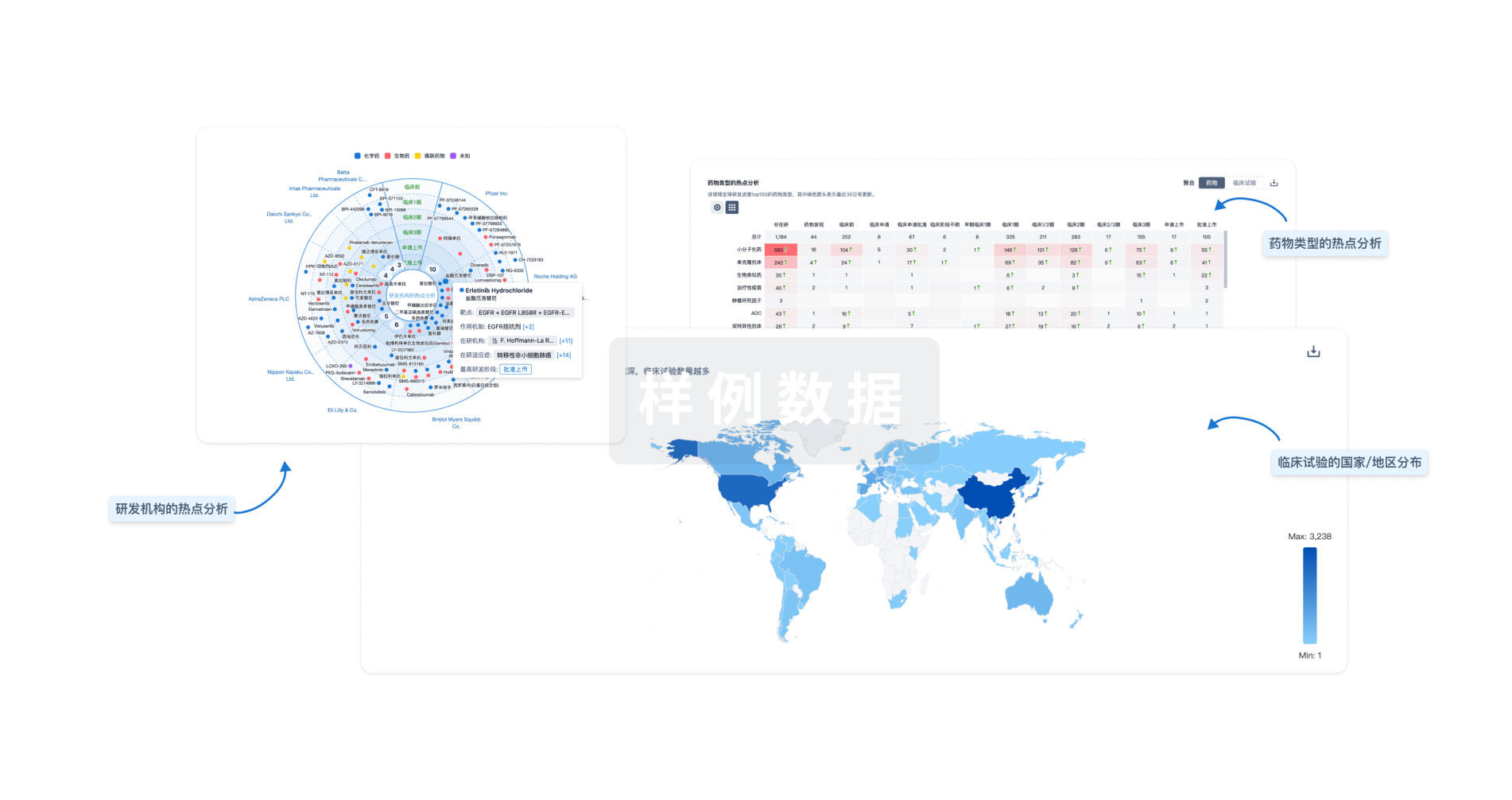
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用



