预约演示
更新于:2025-05-07
Post-traumatic neuralgia
创伤后神经痛
更新于:2025-05-07
基本信息
别名 Post-traumatic neuralgia、外傷後神経痛、ガイショウゴシンケイツウ |
简介- |
关联
4
项与 创伤后神经痛 相关的药物靶点 |
作用机制 TRPV1激动剂 |
最高研发阶段批准上市 |
首次获批国家/地区 加拿大 |
首次获批日期2010-07-15 |
靶点- |
作用机制- |
原研机构 |
非在研适应症- |
最高研发阶段临床3期 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
靶点 |
作用机制 MAGL抑制剂 |
在研机构 |
在研适应症 |
最高研发阶段临床1期 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
17
项与 创伤后神经痛 相关的临床试验NCT06772142
Early Feasibility of the Nervonik Peripheral Nerve Stimulation Device
A multicenter, 30 patient prospective single arm evaluation of the Nervonik system in symptomatic patients with chronic severe knee, elbow or shoulder pain.
COHORT 1: The initial cohort of patients will receive the Nervonik neurostimulator for up to 8 hours. The patient will remain local to the care facility for implant stimulator program changes until the patient is satisfied with the degree of pain relief. The implant will be removed from the patient at the end of the evaluation.
COHORT 2: The second cohort of patients will include those patients from cohort 1 who have determined the Nervonik implant provides suitable pain relief and agree to have a permanent implant placed. In addition, the second cohort includes non-cohort one patients meeting the trial requirements and agreeing to participate in the trial.
COHORT 1: The initial cohort of patients will receive the Nervonik neurostimulator for up to 8 hours. The patient will remain local to the care facility for implant stimulator program changes until the patient is satisfied with the degree of pain relief. The implant will be removed from the patient at the end of the evaluation.
COHORT 2: The second cohort of patients will include those patients from cohort 1 who have determined the Nervonik implant provides suitable pain relief and agree to have a permanent implant placed. In addition, the second cohort includes non-cohort one patients meeting the trial requirements and agreeing to participate in the trial.
开始日期2024-11-27 |
申办/合作机构 |
NCT06071936
Efficacy and Tolerability of AP707 in Patients With Chronic Pain Due to Traumatic or Post-operative Peripheral Neuropathy
Over the last years a rising medical need for treatment of chronic pain was identified. Based on previous findings indicating the pain modulating effects of cannabinoids in chronic pain disorders, this clinical trial investigates the efficacy and tolerability of the THC-focused nano endocannabinoid system modulator AP707 in patients with chronic pain disorders due to traumatic or post-operative peripheral neuropathy. Patients receive AP707 or placebo over the course of 14 weeks as an add-on to the standard of care. Changes in pain intensity, quality of life and sleep and others measures are monitored through different scales to assess the efficacy of AP707 in patients with chronic pain due to traumatic or post-operative peripheral neuropathy.
开始日期2023-11-02 |
申办/合作机构 |
NCT06071988
Long Term Efficacy and Tolerability of AP707 in Patients With Chronic Pain Due to Traumatic or Post-operative Peripheral Neuropathy
Over the last years a rising medical need for treatment of chronic pain was identified. Based on previous findings indicating the pain modulating effects of cannabinoids in chronic pain disorders, this clinical trial investigates the long term efficacy and tolerability of the THC-focused nano endocannabinoid system modulator AP707 in patients with chronic pain disorders due to traumatic or post-operative peripheral neuropathy. Patients receive AP707 or placebo over the course of 14 weeks as an add-on to the standard of care. Changes in pain intensity, quality of life and sleep and others measures are monitored through different scales to assess the efficacy of AP707 in patients with chronic pain due to traumatic or post-operative peripheral neuropathy.
开始日期2023-11-02 |
申办/合作机构 |
100 项与 创伤后神经痛 相关的临床结果
登录后查看更多信息
100 项与 创伤后神经痛 相关的转化医学
登录后查看更多信息
0 项与 创伤后神经痛 相关的专利(医药)
登录后查看更多信息
95
项与 创伤后神经痛 相关的文献(医药)2025-02-01·Toxicon
An update on botulinum toxin treatment of painful diabetic neuropathy, post-traumatic painful neuropathy/neuralgia, post-herpetic neuralgia and occipital neuralgia
Review
作者: Jabbari, Bahman ; Tohidian, Ava
2024-12-01·Annales de Chirurgie Plastique Esthétique
Combined ultrasound imaging/neurophysiological evaluation for surgical planning in upper limb traumatic nerve injuries with concomitant vascular damage: Two emblematic cases and a review of litterature
Article
作者: Tripoli, M ; Gagliardo, C ; Corradino, B ; Rimmaudo, G ; Rosatti, F ; Di Stefano, V ; Brighina, F ; Toia, F ; Cordova, A ; Gagliardo, A
2024-11-12·Zhongguo zhen jiu = Chinese acupuncture & moxibustion
[Development of clinical questions and outcomes on Clinical Practice Guideline of Fire Needling Therapy for Herpes Zosters].
Review
作者: Li, Bin ; Hu, Jing ; Liu, Yali ; Liu, Lu ; Zhao, Nanqi ; Ding, Nan ; Mu, Dongxiao ; Wu, Xiaodong
1
项与 创伤后神经痛 相关的新闻(医药)2025-04-21
·药智网
意大利医史学家卡斯蒂廖尼在《医学史》中指出,医学诞生于人类对痛苦的感知与缓解的渴望,疼痛研究始终是医学的核心命题。当前全球疼痛市场规模持续扩大,甚至被资本市场视为继减重药之后的医药新风口。现实案例印证了这一需求:年轻产妇分娩时急切要求无痛注射,耄耋老人临终前因止痛药失效饱受骨病折磨。数据显示,某三甲医院妇产科无痛分娩率已达85%,折射出现代社会对高效、安全止痛方案的迫切期待。临床期待着即兼顾疗效,又低副作用与高安全性的跨时代产品上市。2025年1月30日,Vertex Pharmaceuticals旗下FIC疗法Suzetrigine(VX-548)获FDA批准上市,用于治疗成人中至重度急性疼痛,该药为FDA批准的首款新机制的非阿片类止痛药物,FDA评价其或将推动疼痛管理进入了一个全新的时代。四大因素疼痛管理成为下一“风口”纵观历史,每个爆款新药都有着相似的底层逻辑,而疼痛之所以能被资本市场誉为下一个减重市场,其原因也类似,甚至更强。1. 庞大患者规模根据《中国疼痛防控与健康促进战略蓝皮书:中国疼痛医学发展报告(2020)》,我国慢性疼痛患者超过3亿人,且每年以1000万~2000万的速度在快速增长,患者人群有年轻化趋势。而另一方面,美国作为止痛药使用频率最高的国家,2020年数据显示,每两名美国成年人就拥有一张阿片类药物止痛处方,且阿片类药物的使用居全球之最。疼痛诊疗认知与止痛药使用犹如一把双刃剑,很难把控其中平衡点。2. 长久的用药周期对于疼痛而言,多数人认为其主要是由疾病所致,病在前,痛在后,但这既对也不对。与肥胖类似,如今的疼痛已不仅仅是一种症状,更是一类疾病,2018年世界卫生组织已将慢性疼痛列为独立疾病。而临床上伴随长期疼痛的疾病比比皆是,例如脊柱源性疼痛、软组织疼痛、神经病理性疼痛以及癌症性疼痛。某种层面来看,急性疼痛可以消失,但大部分慢性疼痛疾病无法治愈,患者往往需要长期服用止痛药,比之减重市场的用药周期与用药频率,明显更高。以DPN患者为例,在临床试验中,福泰制定的时间长达12周。不过,在实际生活中,不少慢性疼痛患者服用止痛药的时间远远大于12周。《Best Pract Res Clin Rheumatol》上的一项研究显示,有80%慢性疼痛患者服用止痛药物超过一年时间。3. 迫切的临床需求尽管临床上用于疼痛管理的药物与治疗方法很多,但其均存在着临床局限性:对于非甾体抗炎药而言,其虽不具备成瘾风险,但其止痛效果较差,且长期使用还会有胃肠道出血与肾损伤风险。对于阿片类药物(如芬太尼)虽然止痛效果好,对癌痛有效,但长期使用却有极大的成瘾风险,对呼吸、胃肠功能等非痛觉相关中枢系统产生抑制。更关键的是,现有疼痛管理药物还存在明显的靶向性不足,无法精准区分病理性和生理性疼痛信号,导致30%~50%神经病理性疼痛患者疗效不佳。因此,无论是临床上,还是院外市场,疼痛管理领域都存在着对更有效、更安全的疼痛治疗方法的巨大需求。4. 强烈的支付意愿长期疼痛会削弱神经自控力,疼痛程度与持续时间直接推高患者对止痛药物的依赖度和支付意愿。人类为此曾尝试过诸多非常规手段:公元46年,古罗马医师拉杰斯首创电击止痛法,将活体电鳐置于患者患处放电至麻木,认为可激发内啡肽镇痛;19世纪英国化学家戴维则发现吸入"笑气"(一氧化二氮)既能致幻又能缓解智齿剧痛,由此开创气体麻醉先河。5. 上涨的疼痛认知从医学的角度上看,这些对疼痛的轻视和忍耐是一种危险的行为。对于病源性疼痛,及时进行治疗干预是关键,而对于部分无法避免的疼痛,疼痛控制则是提升患者生活质量的有效手段。随着时代进步,大众对疼痛管理的认知也水涨船高,非甾体类药物与强效阿片类药物也逐渐被大众接受。总而言之,疼痛市场与减重市场都有着很多相类似的点,长期来看,明显具备成为爆品的潜力。时代变化20年需求迎来希望截至目前,临床上用于治疗疼痛的常见用药主要有两大类,第一类为非甾体类的消炎药,比如日常熟知的布洛芬和阿司匹林,其主要用于牙齿疼,肌肉酸痛等外周部位的炎症或外伤引起的疼痛;第二则是阿片类止痛药,代表药物有吗啡、芬太尼、可待因,因其可以阻断疼痛信号向脊髓与大脑的传递,因此理论上其止痛效果往往更强。而如今相对成熟的临床止痛药应用,却也并非一蹴而就,在人类与疼痛漫长的抗争中,无数凝聚了人类智慧的镇痛药物应运而生。有的镇痛药(阿司匹林)现已有了别的用武之地,而有的镇痛神药却消失在了历史长河中,更有的止痛药则是因其滥用风险被世界各国严格管控。图片来源:博药时至今日,止痛药领域的发展路径一方面可以说是围绕非甾体抗炎的有效性与胃肠道反应演变,而另一方面则是围绕如何降低阿片类药物成瘾性推进,期间诞生的各类新药互相弥补局限性,却又不断创造局限性,近200余年里,并没有哪款止痛药药堪称完美。直到2025年首款非阿片类药物的上市,让该领域内研究者看到了新的希望。综合临床应用场景来看,尽管阿片类镇痛药让人谈之色变,但其却是综合镇痛效果、心血管和肾脏副作用等方面,是现阶段疼痛医学的毫无疑问的基石药物,而COX-2特异性抑制剂优势渐显,逐渐有了替代传统非甾体消炎药的潜力,成为患者止痛选择的新趋势。多年来,阿片类镇痛药不仅占临床用药的最多席位,且占有绝对多的市场份额,2022年镇痛类药物PDB样本医院销售额为53.65亿元,仅地佐辛、舒芬太尼、瑞芬太尼和布托啡诺4款阿片类镇痛药的合计销售额就达36.78亿元,占市场份额的68.56%。图片来源:德邦证券但很明显,阿片类镇痛药绝非疼痛管理市场的最终归属,20年里无新机制止痛药上市也并不代表现有临床治疗已趋于完美,事实上临床上仍迫切需要一款止痛效果好、安全性佳、无成瘾性、顺应性良好、可用于慢性疼痛(如癌痛)的划时代新药。新药助力非阿片药时代来临尽管疼痛管理市场历经200余年发展,但至今,止痛药的新药研发方向仍与过去并无太大区别,绝大多数新药仍以非甾体药物优化、阿片类药物迭代两大方向,唯一不同的是,随着基础研究水平的上涨,一些拥有全新止痛机制的非阿片类新药逐渐诞生,某种层面上推动领域进入了一个全新的阶段。作为最被临床与市场寄予希望的方向,非阿片类镇痛药在过去几十年间引无数药企扎身其中,却又不断经历失败,仍不愿放弃。2006年,辉瑞花费5亿美元买下一款选择性神经生长因子(NGF)抑制剂。然而,经过十几年的研发,等待辉瑞的却是失败。2021年3月,FDA以1:19票否决了这款药物的上市申请,辉瑞不得不终止这款药物所有全球开发项目。2016年,梯瓦与再生元就NGF抑制剂Fasinumab达成2.5亿美元的研发协议,然而在其针对糖尿病周围神经病变、纤维肌痛的临床试验相继失败后,2022年再生元也选择了暂停Fasinumab的研发。2018年,已经完成三个2期临床的VX-150,虽概念性地证明了NaV1.8抑制剂在急性、慢性和神经性疼痛中的止痛作用,但由于疗效和副作用方面的原因,最终被Vertex终止。在过去的20年时间里,围绕着新型镇痛药的研发,上述类似的失败案例还有很多。可以说,过去药企们针对新型镇痛药物的研发,一直是在黑暗中前行。但这几十年对非阿片类药物的新药摸索的过程中也诞生了不少充满希望的细分赛道,有效地推动了疼痛管理新药研究的巨大进步。部分“非阿片类药物”的机制与代表药物类别作用机制代表药物乙酰苯胺类抑制中枢神经系统中前列腺素的合成对乙酰氨基酚(扑热息痛)、丙帕他莫COX抑制剂抑制COX,减少前列腺素的合成氟比洛芬酯、酮咯酸选择性COX2抑制剂抑制COX-2,减少前列腺素的合成帕瑞昔布钠、塞来昔布a2肾上腺素能受体激动剂作用于中枢和外周神经系统的a2肾上腺素能受体右美托咪定、可乐定NMDA受体拮抗剂抑制NMDA受体活性,减少兴奋性神经递质释放氯胺酮钙通道阻滞剂调节中枢神经系统钙通道,减少神经递质的钙依赖性释放VX-548TRPV1抑制剂阻断TRPV1通道的激活来发挥作用,从而实现止痛效果MTX-071NGF抑制剂抑制NGF及其受体,阻断信号传导来发挥作用Fasinumab、TanezumabWNT信号通路阻滞剂Wnt抑制剂通过调节神经元的兴奋性和脊髓突触可塑性来缓解疼痛/ATR2拮抗剂抑制P38MAPK和ERK-MAPK信号通路来缓解神经病理性疼痛TRD-205选择性CCR2拮抗剂抑制炎症和疼痛信号的传递来发挥作用CNTX-6970内源性大麻素下的FAAH通过促进内源性大麻素释放或使用外源性大麻素配体可发挥一定的镇痛作用CC-97489NTRK1抑制剂抑制NTRK1激酶的活性,阻断神经生长因子(NGF)与其受体的结合VC004、FB-1003数据来源:公开数据整理据药智数据显示,目前全球领域有超过300余种疼痛管理相关新药在研,其中除乙酰苯胺类、选择性COX2抑制剂与阿片类药物外,也有不少新生代的非阿片类药物在研,比如NaV1.8抑制剂、Nav1.7抑制剂、TRPV1抑制剂、FAAH抑制剂、NGF抑制剂等。NaV1.8/1.7抑制剂遗传研究表明,人体内一共发现9个钠通道,分别为Nav1.1-Nav1.9,其中1.7和1.8仅在周围神经中表达。在感受疼痛时,Nav1.7通道率先启动,然后Nav1.8通道在疼痛信号沿着神经传导时启动,因此在疼痛管线新药研究中,该两个靶点的相关新药研究被寄予厚望。随着研究的深入,Nav1.7抑制剂在临床试验中的表现不尽如人意,靶点占位不足、生物利用度差等问题导致其在实际应用中存在较大局限性,最终使得Nav1.7作为镇痛药物开发的靶点逐渐被取代,研究者们将注意力转向了Nav1.8这一亚型。Nav1.8主要表达于伤害感受神经元上的河豚毒素不敏感型钠通道,在外周神经系统的痛觉信号传导中起着关键性作用,是疼痛治疗的高选择性作用靶点,而且,由于Nav1.8不参与中枢神经相关的活动,Nav1.8抑制剂不会对运动功能产生影响,也不会存在成瘾性问题。2025年1月30日,FDA批准了一款名为Suzetrigine(VX-548)的新型止痛药。成为20多年来首个全新作用机制的止痛药物,即不通过阻断阿片类受体而达到镇痛目的,避免了以往药物成瘾现象,兼顾有效性与安全性。有效性方面,在过去对比普瑞巴林的临床2期试验中,疗效组VX-548的治疗者组在第12周时疼痛评分较基线降低了-2.02,止痛效果与普瑞巴林相当。安全性方面,Vertex耐受性良好,不良事件(AEs)发生率为22.9%,大多数AEs为轻度至中度,无严重不良事件(SAE)与VX-548相关,且并未出现因AEs导致治疗中断的情况。VX-548的上市,成功为Nav1.8靶点打开了想象空间,使得该领域内众多药企在成药性验证方面有了足够的底气。而在Nav1.8抑制剂的研发历程中,也充满艰辛与困难,虽然目前关于NaV1.8抑制剂的代际划分尚未形成完全统一的定义标准,但从产品优势替换层面仍可初步归纳为如今的三代产品。第一代NaV1.8抑制剂:以VX-128、VX-150等早期开发的靶向NaV1.8通道的化合物为主,主要通过阻断该通道的电压门控特性来抑制外周痛觉神经元信号传导,开创了选择性阻断NaV1.8通道的先河,但由于该阶段产品选择性不足、代谢稳定性较差等问题,多款新药被迫终止。第二代NaV1.8抑制剂:主要在早期化合物基础上对选择性和药效进行了优化改进,使其具有了更强的靶点结合能力和更低的脱靶效应,尤其是在NaV1.8抑制剂的安全性提升明显。第三代NaV1.8抑制剂:目前公开资料中并未对其定义的明确阐述,仅出现于福泰制药的相关管线宣传中,但参考过去靶向抑制剂的迭代逻辑,第三代产品或会在有效性、安全性、耐药性与特殊适应症层面形成差异化。药品名称产品分类靶点原研单位全球最高阶段中国最高阶段管线状态VX-584第二代SCN10A福泰制药批准上市暂无活跃VX-150第一代SCN10A福泰制药临床Ⅱ期暂无终止LTG-001/SCN10ALatigo Biotherapeutics临床Ⅱ期暂无活跃VX-993第三代SCN10A福泰制药临床Ⅱ期暂无活跃JMKX-000623第一代SCN10A上海济煜医药科技有限公司奥立安药厂临床Ⅱ期临床Ⅱ期活跃HRS4800第一代SCN10A江苏恒瑞医药股份有限公司临床Ⅱ期临床Ⅱ期活跃PF-4531083/SCN10A辉瑞临床Ⅱ期暂无活跃PF-06305591/SCN10A辉瑞临床Ⅰ期暂无终止VX-961第一代SCN10A福泰制药临床Ⅰ期暂无-VX-128第一代SCN10A福泰制药临床Ⅰ期暂无终止VX-973第三代SCN10A福泰制药临床Ⅰ期暂无活跃FZ008-145第一代SCN10A广州费米子科技有限责任公司健康元药业临床Ⅰ期临床申请活跃LTG-305/SCN10ALatigo Biotherapeutics临床Ⅰ期暂无活跃MK-5661/SCN10A默沙东临床Ⅰ期暂无活跃STC-004/SCN10ASiteOne Therapeutics Inc临床Ⅰ期暂无活跃HBW-004285第一代SCN10A成都海博为药业有限公司临床Ⅰ期临床Ⅰ期活跃ODM-111/SCN10A奥立安药厂临床Ⅰ期暂无活跃HRS-2129第二代SCN10A山东盛迪医药有限公司临床Ⅰ期临床Ⅰ期活跃HBW-004-03/SCN10A成都海博为药业有限公司临床申请暂无活跃CN114437062A/SCN10A成都海博为药业有限公司临床前暂无活跃数据来源:药智数据截至目前,全球还有10余款Nav1.8靶向药在研,其中福泰制药作为领域开拓者,既是技术迭代的主要推动者,也是管线布局数量最多的企业。国内企业而言,济煜医药、恒瑞医药、健康元与海博为药业则均有不同阶段与技术的布局。产品分类药品名称靶点原研单位全球最高阶段中国最高阶段管线状态第一代VX-150SCN10A福泰制药临床Ⅱ期暂无终止VX-961SCN10A福泰制药临床Ⅰ期暂无终止VX-128SCN10A福泰制药临床Ⅰ期暂无终止第二代VX-584SCN10A福泰制药批准上市暂无活跃第三代VX-993SCN10A福泰制药临床Ⅱ期暂无活跃VX-973SCN10A福泰制药临床Ⅰ期暂无活跃数据来源:药智数据TRPV1抑制剂TRPV1是一种非选择性阳离子通道,属于瞬时受体电位(TRP)离子通道家族的香草素亚家族。其最初从辣椒中被发现,因此也被称为辣椒素受体或香草素受体1。随着研究深入,TRPV1在许多疼痛传导途径的上游区的调节功能被证实,因此TRPV1成为治疗疼痛的新靶点,尤其是针对慢性疼痛,可有效避免药物成瘾和大量副作用。而对于TRPV1靶点,其最初载体其实是TRPV1激动剂,辣椒碱也被美国药典收录,但后来由于其诸多不良反应,比如灼热感、数天至几星期后会导致痛觉丧失,缺乏对有害刺激的反应,之后TRPV1抑制剂逐渐成为新的研究重点。目前,市面上已有部分新型TRPV1靶向制剂被陆续报道,其在研发数量上也是仅次于NaV抑制剂的存在,在非阿片类止痛药领域拥有不错的临床价值。据药智数据显示,全球TRPV1靶向药领域仅有Qutenza与Zucapsaicin获批上市,前者用于成人患者治疗足部与糖尿病周围神经病变(DPN)相关的神经性疼痛及治疗带状疱疹后遗神经痛引起的神经病理性疼痛;后者则用于骨关节炎。药品名称适应症场景原研单位全球最高阶段管线状态RTX-GRT7039骨关节炎疼痛格兰泰临床Ⅲ期活跃瑞尼毒素 Resiniferatoxin癌性疼痛;骨关节炎疼痛Sherrington Pharmaceuticals Inc临床Ⅲ期活跃伏卡赛辛 Vocacapsaicin术后疼痛Concentric Analgesics Inc临床Ⅲ期/SAF-312慢性疼痛;牙痛;眼痛;眼表疼痛诺华临床Ⅱ期活跃ACD-440周围神经痛;疼痛;神经病理性疼痛AlzeCure Pharma AB临床Ⅱ期活跃NEO-6860骨关节炎疼痛Neomed Institute临床Ⅱ期/V-116517带状疱疹后遗神经痛;流感病毒感染;疼痛;骨关节炎疼痛Purdue Pharma LP;盐野义制药临床Ⅱ期/DWP-05195带状疱疹后遗神经痛大熊制药临床Ⅱ期/GR-705498偏头痛;慢性疼痛;牙齿疾病;疼痛葛兰素史克临床Ⅱ期/JTS-653带状疱疹后遗神经痛Japan Tobacco Inc临床Ⅱ期/AZD-1386创伤后神经痛;带状疱疹痛;术后疼痛;神经痛;骨关节炎疼痛阿斯利康临床Ⅱ期/MK-2295术后疼痛默沙东临床Ⅱ期/JM2947疼痛JMackem Co Ltd临床Ⅰ期活跃玛伐曲普 Mavatrep疼痛强生临床Ⅰ期/ABT-102术后疼痛;炎症性疼痛;疼痛雅培临床Ⅰ期/PF-3864086疼痛辉瑞临床Ⅰ期/GRC-6211牙痛Glenmark Pharmaceuticals SA临床Ⅰ期/AMG-517疼痛安进临床Ⅰ期/BSEN-760慢性疼痛Bsense Bio Therapeutics Ltd临床前活跃数据来源:药智数据而在研药物层面,全球临床阶段用于疼痛管理的TRPV1靶向药接近20个,但其中仅有少部分管线的状态处于积极阶段,最有望上市的产品有两款,分别是格兰泰的RTX-GRT7039与Sherrington的Resiniferatoxin,均处于临床Ⅲ期阶段。后者更是在2024年5月获得了FDA的突破性疗法认定,其在降低疼痛以及安全性方面具有显著效果。TRPV1抑制剂对比NaV1.8抑制剂,其在作用机制、靶点特性及临床应用场景均存在显著差异性,TRPV1抑制剂主要抑制伤害性热刺激和炎症介导的痛觉敏化,主要应用于炎症性疼痛、慢性疼痛等领域,而NaV1.8抑制剂则直接阻断痛觉神经元的电信号传导,适用于急性疼痛和神经病理性疼痛。因此,严格意义上来讲,TRPV1抑制剂与NaV1.8抑制剂并非竞品,反而有望在未来形成协同止痛机制,也是被研究界寄予厚望的止痛技术。NGF抑制剂近1个世纪以来,学者们关注并不断揭示神经营养因子(Neurotrophins)在外周神经传导(包含疼痛的传导)过程中的重要作用。在慢性疼痛的关节周围,神经生长因子(Nerve Growth Factor,NGF)浓度异常升高,促使机体释放P物质等引发一系列神经源性炎症,最终诱发疼痛。神经生长因子(NGF)是一种重要的致痛物质,可通过促进外周炎症反应、伤害感受器敏化、异位放电、交感神经芽生及中枢敏化参与神经病理性疼痛的发生和维持,NGF及其受体已成为临床镇痛药物开发的重要靶点。抑制NGF及其受体可有效缓解神经病理性疼痛。基于NGF及其受体的镇痛药物主要是通过阻断NGF、拮抗TrkA 受体和(或)p75 受体、抑制胞内TrkA激酶活性及NGF/TrkA 下游通路等策略开发相关药物。其中NGF抑制剂的研究热度相对更高。目前,NGF抑制剂领域主要分为两个主要方向,一者是人源化NGF单克隆抗体,由于其促神经分化的作用,镇痛剂量的NGF抗体不会引起认知功能的下降,对神经系统无显著的副作用,但临床试验却发现了神经病变和破坏性关节病等副作用可能,且与剂量、用药时间正相关;另一个则是NGF小分子抑制剂,但研究进度相对靠后,多处于临床前阶段。药品名称靶点适应症方向原研单位全球最高阶段管线状态法司努单抗 FasinumabNGF腰痛;骨关节炎;骨关节炎疼痛再生元制药临床Ⅲ期活跃伏雷努单抗 FulranumabNGF;NGFR癌性疼痛;神经痛;腰痛;膀胱疼痛;骨关节炎疼痛等安进临床Ⅲ期/他奈珠单抗 TanezumabNGF;NGFR慢性疼痛;癌性疼痛;神经痛;腰痛;膀胱疼痛;骨痛;骨转移疼痛礼来;辉瑞临床Ⅲ期/LEVI-04BDNF;NGFR;NT-3;NT-4骨关节炎疼痛Levicept Ltd;辉瑞临床Ⅱ期活跃EP-9001ANGF骨转移疼痛苑东生物临床Ⅱ期活跃DS002NGF;NGFR疼痛达石药业临床Ⅱ期活跃MEDI-7352NGFR慢性疼痛;糖尿病性神经性疼痛;骨关节炎疼痛阿斯利康临床Ⅱ期/ABT-110NGF疼痛;腰痛;骨关节炎疼痛PanGenetics BV;雅培临床Ⅱ期/SSS40NGF癌性疼痛;骨转移疼痛三生制药临床Ⅰ期活跃TNM009NGF关节痛;慢性疼痛;疼痛;癌性疼痛;骨关节炎疼痛;骨转移疼痛泰诺麦博制药临床Ⅰ期活跃AK-115NGF疼痛康方生物临床Ⅰ期/MEDI-578NGFR骨关节炎疼痛Medimmune LLC临床Ⅰ期/AMG-819NGF疼痛安进临床Ⅰ期/数据来源:药智数据数据显示,目前全球共有13款用于疼痛管理的单抗进入临床阶段,但其中活跃管线占比不足50%,NGF治疗开发层面全球制药企业屡屡受挫。辉瑞/礼来合作开发的Tanezumab作为最早进入临床的NGF抗体药物,但由于其安全性问题(包括OA快速进展和全膝关节置换术需求增加)其上市之路数度受阻。再生元的Fasinumab也因安全性问题,被FDA叫停了临床试验。强生、阿斯利康、安进也纷纷布局NGF抗体项目开发,却也举步维艰。目前来看,在NGF单抗用于关节疼痛治疗层面,制约其发展的主要原因在于关节止痛后的关节置换风险,据多项数据显示,LEVI-04有望解决NGF药物的上述安全性问题,其在拥有相当的镇痛效果(WOMAC疼痛评分平均降幅大于50%)的同时,不会导致骨关节炎快速进展,甚至还能维持神经营养因子稳态,利于维持软骨和骨修复。作为疼痛管理领域最具希望的下一代镇痛药物靶点之一,领域内后来者的热情非凡,尤其是国内相关Biotech企业,目前已知的就有苑东生物的EP-9001A、达石药业的DS002、三生制药的SSS40、泰诺麦博的TNM009。当然,除了上述NaV1.8抑制剂、NGF抑制剂与TRPV1抑制剂外,当今非阿片类止痛药研发领域还有不少值得重点注意的新药领域,比如WNT信号通路阻滞剂、ATR2拮抗剂、选择性CCR2拮抗剂、α2肾上腺素受体激动剂、内源性大麻素下的FAAH、NMDAR受体拮抗剂、NTRK1抑制剂等。每个细分领域都有着一份独属于自身的发展历程,虽然如今表面上NaV1.8抑制剂似乎在新机制止痛药层面已然拔得头筹,不过未来谁敢保证上述细分领域就不会迎来爆发?小结总结来看,疼痛管理的爆发逻辑已清晰可见:庞大患者基数、长周期用药属性叠加强大的支付意愿,使其市场黏性媲美减重赛道,加之现有药物(阿片类成瘾、非甾体药效弱)存在明显临床局限性与未满足需求,千亿替代空间,怎能不让人异常兴奋。而事实上,过去20年,疼痛管理新药研发屡屡碰壁,MNC药企无一不在该领域栽过跟头,但2025年Nav1.8抑制剂VX-548的获批却给行业注入一剂强心针,也让非阿片止痛药市场成为新的市场热点。展望未来,随着靶点迭代能力持续加强(从第一代到第三代Nav1.8抑制剂)、适应症差异化布局(聚焦口服制剂,专注癌痛、慢性痛)等竞争要素的细分。更关键的是,国内药企在疼痛管理新药研发层面投入强劲,尽管短期来看,在各细分领域均无任何一款新药占据头部优势,但如恒瑞、海思科与一众Biotech企业仍有望给行业带来新的惊喜。可以预见,疼痛管理新药市场,即将迎来百年时代变革,这场从精准机制打破阿片依赖的变革,或将重塑人类对抗疼痛的终极范式。来源 | 博药(药智网获取授权转载)撰稿 | 博药内容中心责任编辑 | 八角声明:本文系药智网转载内容,图片、文字版权归原作者所有,转载目的在于传递更多信息,并不代表本平台观点。如涉及作品内容、版权和其它问题,请在本平台留言,我们将在第一时间删除。合作、投稿 | 马老师 18323856316(同微信) 阅读原文,是受欢迎的文章哦
上市批准临床研究
分析
对领域进行一次全面的分析。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
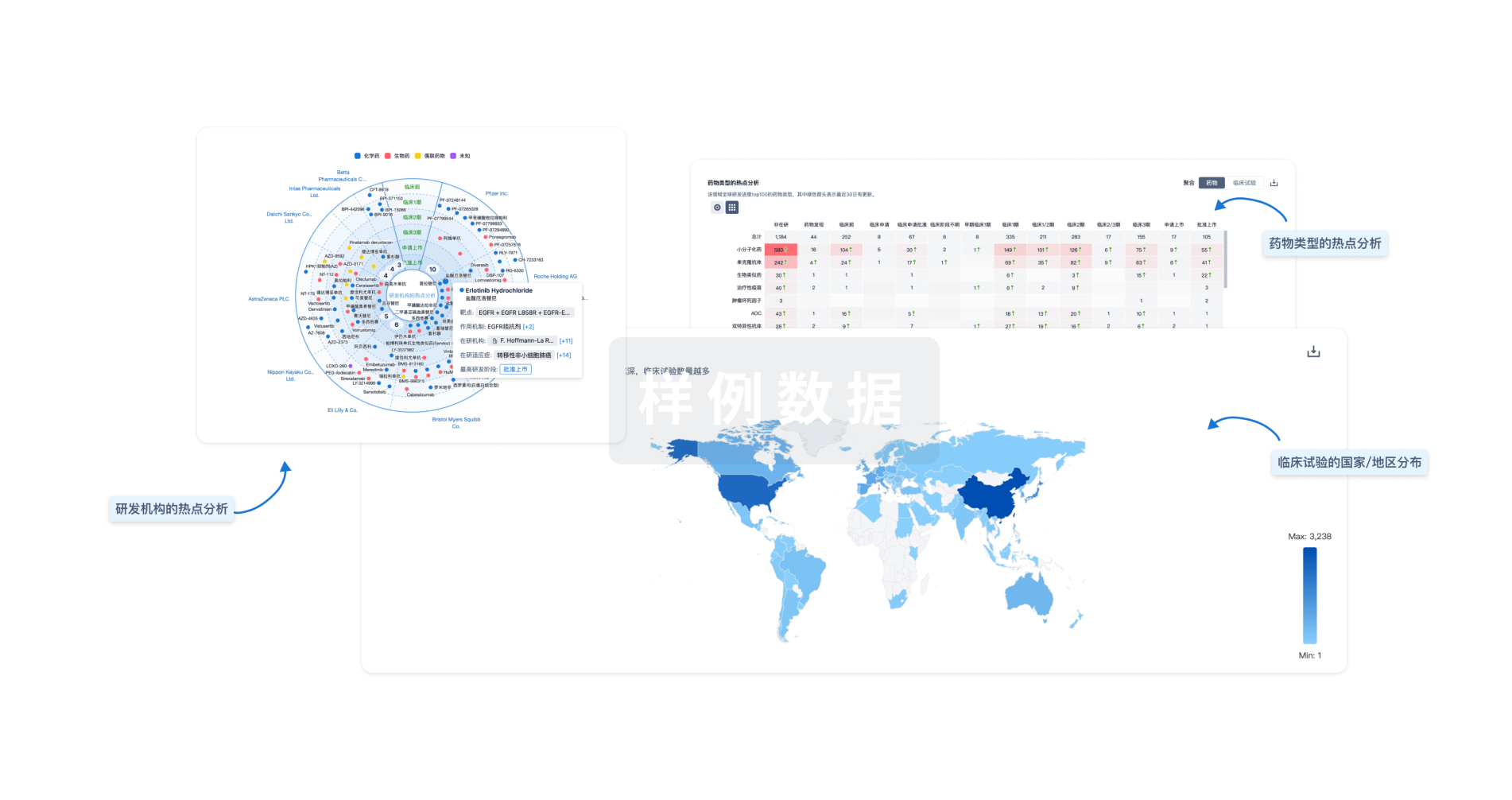
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用