预约演示
更新于:2025-07-06
University of Michigan Comprehensive Cancer Center
教育|Michigan, United States
教育|Michigan, United States
更新于:2025-07-06
概览
关联
100 项与 University of Michigan Comprehensive Cancer Center 相关的临床结果
登录后查看更多信息
0 项与 University of Michigan Comprehensive Cancer Center 相关的专利(医药)
登录后查看更多信息
720
项与 University of Michigan Comprehensive Cancer Center 相关的文献(医药)2025-06-13·CLINICAL CANCER RESEARCH
Neoadjuvant Chemotherapy and Surgery versus Surgery for Organ Preservation of T3 and T4a Nasal and Paranasal Sinus Squamous Cell Carcinoma: ECOG-ACRIN EA3163
Article
作者: Adkins, Douglas R. ; Chakravarthy, A. Bapsi ; Samuels, Michael A. ; Duan, Fenghai ; Solares, Clementino A. ; Khan, Saad A. ; Subramaniam, Rathan M. ; Ikpeazu, Chukwuemeka V. ; Lin, Derrick T. ; Axelrod, Rita S. ; Ghaly, Maged ; Cohen, Marc ; El-Sayed, Ivan H. ; Burtness, Barbara A. ; Snyderman, Carl H. ; Swiecicki, Paul L. ; Hwang, Peter H. ; Saba, Nabil F. ; Chung, Christine H. ; McDonald, Mark W. ; Flamand, Yael ; Shin, Dong M. ; Le, Christopher H. ; Flampouri, Styliani ; Hanna, Ehab Y.
Abstract:
Purpose::
Neoadjuvant chemotherapy for structure preservation (SP) in nasal and paranasal sinus squamous cell carcinoma (NPNSCC) has been described in single-institution studies but not in randomized studies. EA3163 was a randomized study investigating whether cytoreductive neoadjuvant chemotherapy would improve SP or overall survival (OS).
Patients and Methods::
Patients with T3/T4a and select T4b NPNSCC requiring orbital or base of skull (BOS) resection were randomized to surgery (arm A) versus surgery preceded by docetaxel/cisplatin for three cycles (arm B). The degree of anticipated SP (orbit and BOS) was required preoperatively and after chemotherapy. SP was noted at surgery. Co-primary objectives were the SP rate (orbit/BOS) and OS. Eighty-two patients needed to be accrued for 81% power with a 0.1 one-sided alpha using Fisher’s exact test for SP rate and 83% with a 0.1 one-sided alpha using the log-rank test for OS.
Results::
Among 23 evaluable patients, the overall SP rate was 30%: 15% in arm A (N = 2/13; 95% confidence interval (CI), 1.9%–45.4%) and 50% in arm B (N = 5/10; 95% CI, 18.7%–81.3%; P = 0.17). Among 18 patients with pathologic T3/T4a disease, the overall SP rate was 39%: 18% in arm A (N = 2/11; 95% CI, 2.3%–51.8%) and 71% in arm B (N = 5/7; 95% CI, 29.0%–96.3%; P = 0.049). Orbit and BOS-specific preservation rates were 38% (95% CI, 8.5%–75.5%) versus 83% (95% CI, 35.9%–99.6%) and 33% (95% CI, 9.9%–65.1%) versus 67% (95% CI, 29.9%–92.5%) in arm A versus B, respectively. The most common grade ≥3 toxicities included mucositis, anemia, nausea and lymphopenia (all >10%). No grade 5 events were reported.
Conclusions::
These results support neoadjuvant chemotherapy as an effective intervention for SP in T3/T4a NPNSCC and deserve further evaluation.
2025-06-13·CLINICAL CANCER RESEARCH
Comparing Durvalumab, Olaparib, and Cediranib Monotherapy, Combination Therapy, or Chemotherapy in Patients with Platinum-Resistant Ovarian Cancer with Prior Bevacizumab: The Phase II NRG-GY023 Trial
Article
作者: Nagel, Christa I. ; Rodabaugh, Kerry J. ; AlHilli, Mariam ; Rose, Peter G. ; Moore, Kathleen N. ; Liu, Joyce F. ; John, Veena S. ; Morse, Christopher B. ; Kohn, Elise C. ; Siedel, Jean ; Lee, Jung-Min ; Miller, David S. ; Miller, Austin ; Matsuo, Koji ; Bradford, Leslie S. ; Shah, Chirag A. ; Washington, Christina ; O’Shea, Andrea ; Hopp, Elizabeth E. ; Chan, John K.
Abstract:
Purpose::
We assessed the efficacy of anti–PD-L1 durvalumab in combination with olaparib and cediranib (DOC), compared with the standard-of-care chemotherapy (SOC) in patients with platinum-resistant ovarian cancer (PROC), who had prior bevacizumab.
Patients and Methods::
NRG-GY023 was the first randomized four-arm superiority phase II trial enrolling patients with high-grade serous/endometrioid or clear-cell PROC with prior bevacizumab exposure. Patients were randomized 1:2:2:2 to SOC (weekly paclitaxel, topotecan, or pegylated liposomal doxorubicin), DOC, durvalumab + cediranib (DC), or olaparib + cediranib (OC). The primary endpoint was progression-free survival (PFS). The secondary endpoints included overall survival, overall response rate, and safety. The design had 80% power to detect an HR of 0.5 using a one-sided, α = 0.1-level test for each comparison with the SOC with a preplanned interim analysis. Experimental arms with HR estimates (vs. SOC) >0.87 could be discontinued.
Results::
A total of 153 patients were enrolled between April 4, 2021, and February 1, 2023. Accrual was permanently closed on February 1, 2023, due to futility. With a data cutoff of September 9, 2024, the median PFS was 3.4, 2.9, 2.5, and 2.8 months, and median overall survival was 7.5, 8.3, 5.7, and 10.2 months for SOC, DOC, DC, and OC, respectively. The overall response rate was 4.3% [95% confidence interval (CI), 0.00–0.19], 15.9% (95% CI, 0.07–0.29), 11.9% (95% CI, 0.05–0.24), and 9.1% (95% CI, 0.03–0.20) for SOC, DOC, DC, and OC, respectively. Compared with SOC, the PFS HR estimates were 1.003 (95% CI, 0.56–1.80), 1.108 (95% CI, 0.63–1.96), and 1.021 (95% CI, 0.57–1.82) for DOC, DC, and OC, respectively. No new safety signals were observed.
Conclusions::
In patients with PROC with prior bevacizumab, all experimental arms failed to reach the primary objective of improving PFS compared with SOC.
2025-06-01·Contemporary Clinical Trials
Effectiveness of out-of-pocket cost COMmunication and financial navigation (CostCOM) in cancer patients: Study protocol for ECOG-ACRIN EAQ222CD
Article
作者: Hawley, Sarah ; Carlos, Ruth C ; Hancock, Judy ; Sadigh, Gelareh ; Duan, Fenghai ; Sicks, JoRean D ; Gareen, Ilana F ; Wagner, Lynne I ; Torres, Mylin ; Shankaran, Veena
BACKGROUND:
High out-of-pocket costs (OOPC) of cancer treatment and lost income result in financial hardship. There is compelling evidence that OOPC communication complemented by financial navigation and counseling will decrease financial hardship by enabling cancer patients to anticipate and accommodate treatment costs and proactively seek financial assistance.
METHODS:
This is a two-arm randomized controlled trial enrolling 720 patients with newly diagnosed solid tumors (stratified by non-metastatic vs. metastatic) who plan to receive anticancer systemic therapy at one of the participating NCI Community Oncology Research Practices (NCORP). Participants are randomized to receive four up to 1-h remote counseling sessions which include systemic therapy OOP cost communication, financial navigation and counseling (CostCOM intervention) vs. enhanced usual care with provision of an informational brochure for Patient Advocate Foundation (PAF), a national non-profit financial navigation organization (EUC). Patients will complete surveys at baseline, 3, 6, and 12 months after enrollment. Our goals are to compare the effectiveness of CostCOM vs. EUC at 12 months on (1) patient-reported cost-related cancer care nonadherence, defined as any self-reported incident of delay, forgo, stop or change in cancer care due to cost concerns and (2) patient-reported material financial hardship, financial worry, and quality of life; and to (3) conduct a process evaluation to examine practice providers' and CostCOM arm patients' satisfaction with the intervention and their perceptions of barriers and facilitators to CostCOM. A successful CostCOM is a scalable and financially sustainable program that can improve cancer care delivery, patients' experience, and health outcomes.
TRIAL REGISTRATION:
NCT06295367.
6
项与 University of Michigan Comprehensive Cancer Center 相关的新闻(医药)2025-03-06
A radiopharmaceutical from ITM Isotope Technologies Munich reduced the risk of disease progression or death by 33% versus Novartis' targeted molecular therapy Afinitor (everolimus) in patients with gastroenteropancreatic neuroendocrine tumours (GEP-NETs). The outcome of the Phase III COMPETE study was first top-lined in January, with the announcement marking one of only a handful of wins for a radiopharmaceutical in a head-to-head trial. Detailed results were presented Thursday at the European Neuroendocrine Tumor Society (ENETS) annual meeting.The trial compared ITM-11 (177Lu-edotreotide) with Afinitor in 309 patients with inoperable, progressive Grade 1 or 2 somatostatin receptor (SSTR)-positive GEP-NETs. According to ITM, approximately 15% of people in each trial arm were treatment naïve, with the remaining 85% or so having received one prior therapy.Results showed that median progression-free survival (PFS) for ITM's therapeutic was 23.9 months, which was significantly and clinically better than the 14.1 months for Afinitor. In comparison, in the Phase III NETTER-2 trial, Novartis' peptide receptor radionuclide therapy Lutathera (lutetium Lu 177 dotatate) reduced the risk of disease progression or death by 72% as a first-line therapy for patients with SSTR-positive well-differentiated Grade 2/3 advanced GEP-NETs versus high-dose octreotide LAR alone, with median PFS in the two arms of 22.8 months and 8.5 months, respectively.ITM told FirstWord that the choice of Afinitor as a comparator in COMPETE was "backed by scientific evidence of efficacy and high clinical acceptance after market authorisation." The company suggested that this decision set "a higher standard for meeting the primary endpoint in more advanced grade tumours," adding that it hopes "physicians will recognise the higher threshold of our study design."FDA filing this year"These successful results validate our decision to design a pivotal Phase III trial directly comparing a targeted radiopharmaceutical against a targeted molecular therapy," CEO Andrew Carey said. Based on the findings, ITM plans to seek approval of ITM-11 in the US this year; however, the company told FirstWord that it is "currently prohibited" from filing in Europe until 2029 due to orphan drug designation on Lutathera.Top-line results also showed that interim median overall survival (OS) was 63.4 months for ITM-11. That was numerically higher than the 58.7 months seen with Afinitor, but not statistically significant at the current analysis. ITM noted that patients were allowed to start an alternative therapy after disease progression, "potentially confounding" the OS data."These data show unequivocal support for [ITM-11's] potential benefit in extending PFS," remarked study investigator Jaume Capdevila, adding that the radiopharmaceutical's "convenient dosing schedule and favourable safety results reinforce its potential as a compelling new treatment option."In COMPETE, patients were treated with ITM-11 every three months for up to four cycles, or with Afinitor daily for up to 30 months, or until disease progression. Meanwhile, ITM's therapy was well tolerated, with treatment-emergent adverse events occurring at a rate of 82.5%, compared with 97% for Afinitor. However, there was one Grade 2 event of myelodysplastic syndrome in the ITM-11 arm.Growing optionsNeuroendocrine tumours are one of the few cancers that have so far benefited from the approval of radiopharmaceuticals. Novartis currently markets Lutathera as a treatment for SSTR-positive GEP-NETs, while Sanofi also has skin in the game, having reached a deal last year to join forces with RadioMedix and Orano Med on the radioligand medicine AlphaMedix (212Pb-DOTAMTATE).Something that differentiates ITM from other players, however, is that it has worked in the radiopharma space for over 20 years and has manufacturing in-house. "Together, with our global isotopes manufacturing business, robust supply chain and experienced clinical and commercial team, we believe we are uniquely positioned as a standout leader in the fast-growing radiopharmaceutical industry," Carey said.ITM-11 — which combines the therapeutic β-emitting radioisotope lutetium-177 with the synthetic SSTR agonist edotreotide — is also being investigated in the Phase III COMPOSE trial in patients with well-differentiated, aggressive Grade 2 or 3 SSTR-positive GEP-NETs.
临床3期临床结果寡核苷酸孤儿药
2023-01-11
·生物谷
莫博赛替尼获得CDE突破性疗法认定并纳入优先审评审批程序,通过全球同步开发、同步递交加速惠及中国患者。
武田中国今日宣布,旗下肺癌创新治疗药物安卫力®琥珀酸莫博赛替尼胶囊,(以下简称“莫博赛替尼”)获得国家药品监督管理局(NMPA)批准正式进入中国,适用于治疗含铂化疗期间或之后进展且携带表皮生长因子受体(EGFR)20号外显子插入突变的局部晚期或转移性非小细胞肺癌(NSCLC)成人患者。莫博赛替尼是全球首款也是目前唯一获批的治疗EGFR 20号外显子插入突变(EGFR exon20 Insertion+)晚期非小细胞肺癌的口服靶向药物,其获批标志着EGFR 20号外显子插入突变晚期非小细胞肺癌治疗史上二十年来的重大突破,宣告针对这一疾病的治疗在中国正式进入靶向治疗新纪元。
肺癌位居中国恶性肿瘤发病率及死亡率首位,其中,非小细胞肺癌(NSCLC)是肺癌最常见的类型。EGFR 20号外显子插入突变发生率约占中国所有NSCLC的2.3%,是EGFR第三大突变。对比常见EGFR突变,EGFR 20号外显子插入突变晚期非小细胞肺癌患者的生存预后更差,5年生存率仅为8%。目前临床上针对这一疾病的治疗以化疗为主,缺乏有效靶向治疗方案。根据一项真实世界数据显示,在缺乏有效针对性治疗情况下,晚期EGFR 20号外显子插入突变患者二线及后线治疗客观缓解率(ORR)低于10%,PFS仅为3.7个月,OS仅为13.6个月。
莫博赛替尼的获批打破这一治疗困境,填补了临床的治疗空白,为EGFR 20号外显子插入突变晚期非小细胞肺癌患者带来生存希望。此次获批是基于1/2期临床试验的疗效和安全性结果,研究在全球范围内纳入114例既往接受过铂类化疗的患者:
1、经独立审查委员会(IRC)评估,患者总缓解率(ORR)达到28%,研究者(INV)评估的ORR达到35%。疾病控制率(DCR)高达78%,IRC评估的中位缓解持续时间(mDoR)延长至15.8个月。
2、患者中位无进展生存期(mPFS)提高到7.3个月,患者中位总生存期(mOS)突破至20.2个月。
莫博赛替尼的成功得益于在药物结构上的创新。EGFR 20号外显子插入突变体形成的空间位阻导致药物结合口袋变小,且该突变同野生型EGFR结构高度相似,因此使得传统EGFR靶向药物结合受阻,对于研发新药的选择性和亲和力有非常高的要求。莫博赛替尼专门针对EGFR 20号外显子插入突变设计,其创新的异丙酯结构形成柔性单环核心,可以更有效地与EGFR 20号外显子插入突变有效结合,具有精准选择和高度亲和的优势,从而攻克这一临床难题。
同济大学附属上海市肺科医院肿瘤科主任、莫博赛替尼国际临床试验主要研究者周彩存教授表示:“临床研究数据让我们看到莫博赛替尼治疗铂类化疗经治人群的中位无进展生存时间超过7个月,中位总生存时间突破20个月,能取得这样的数据结果是非常令人振奋的。莫博赛替尼在国内的获批,标志着EGFR 20号外显子插入突变晚期非小细胞肺癌治疗史上二十年来的重大突破,也宣告了针对这一疾病的治疗正式进入靶向治疗新纪元。”
突破性疗法优先审批临床结果临床研究申请上市
2022-08-26
·药时代
CAR-T细胞疗法正对国内的支付能力做压力测试。单针120万元或129万元为药品费,加上配套医疗费,总价200万元左右。CAR-T商业化意义超越自身,寒蝉凄切,总要有一个勇士去摸天花板,试探环境对前沿疗法,甚至对医药行业创新探索的包容度。到本月,复星凯特阿基仑赛注射液累计治疗超过200位患者,药明巨诺瑞基奥仑赛注射液完成260位患者的回输治疗(包含临床研究及商业化阶段)。国产CAR-T商业化逾一年,完成回输的患者还不足500人,这一届富人不行。药明巨诺生产基地可满足每2500例自体CAR-T细胞治疗的需求,大部分产能闲置。在下游CAR-T厂商亏损死扛且不放量的情况下,上游CGT(细胞基因疗法)CDMO也承受着压力。细胞疗法产业链当下活在寒气中,不过未来被治愈癌症的曙光照耀着。 01 30万元支付天花板由于支付环境差异,美中药物经济学存在一个换算比例,约为1/7,CAR-T疗法在美国的定价,诺华Kymriah为47.5万美元、吉利德Yescarta为37.3万美元,疗法在中国进入47.5万~37.3万人民币区间,才能达到一个各方可以接受的均衡价位。据《international journal of cancer》文献,单人份CAR-T生产成本约为8万美元。药明巨诺瑞基奥仑赛商业化初期,毛利率仅为29.4%,单人份CAR-T生产成本约为70万人民币,加上研发、销售、管理费用,其实是亏损的。预计今年下半年成本预计能降低到50万-55万元,毛利率提升到35%以上,中期(2-3年)通过国内供应品替代进口材料,进一步降低成本到45万元左右,长期(3-5年)则实施新技术,简化/替代/合并单元操作,使得下一代CAR-T产品具有更低成本。医保支付的天花板是多少?现在医保目录中近3000个药品,医保基金最高支付额为30万元。2021年医保谈判结束后,测算专家组组长表示:“不能再高,否则,医保基金就难以承受了。”今年医保谈判一大悬念,在于30万元天花板能否被打破?美国医保是如何支持前沿疗法的?CMS(美国医疗保险与医疗服务中心)通过医疗保险B部分,为接受吉利德CAR-T治疗的患者支付40万美元,为接受诺华CAR-T治疗的患者支付50万美元。CAR-T已纳入超过国内30个城市惠民保。沪惠保最高赔付金额50万元,不限既往症人群。今年3月到5月,4位CAR-T疗法患者通过浙江宁波惠民保产品“天一甬宁保”,分别获赔50.8万元、100万元、94.4万元和47.2万元。杭州市惠民保产品“西湖益联保”、重庆渝快保和北京京惠保也分别完成一次CAR-T疗法患者的理赔,金额分别为50万元、36万元和100万元。商保有崛起之势,大为缓解支付焦虑,但上述患者仍需自费100万元以上,对普通家庭是不可承受之重。细胞疗法的效果又是如此惊艳。截至7月,上海瑞金医院有超过30位患者接受复星凯特CAR-T治疗,其中22位患者已完成首次疗效评估,客观缓解率(ORR)高达95.5%,完全缓解率(CR)高达68.1%,即其中有15位患者获得完全缓解。 02 国内细胞疗法企业全景破解可及性问题,需要支付环境和技术迭代共同努力。自体CAR-T高度定制化,局限性愈发明显。第一款CAR -T疗法诺华Kymriah上市5年,已经触到自己的天花板,今年上半年销售额2.63亿美元,同比下降近12%。据密歇根大学综合癌症中心Samuel Silver博士介绍,美国CAR-T疗法的总费用至少为75万美元,非药品的费用为40万美元至45万美元,与药品费用大致相当。通用型CAR-T(UCAR-T)可实现生产流程的规模化和标准化,有望将生产成本降低90%。国产主要厂家为亘喜生物、北恒生物、科济生物,传奇生物、邦耀生物、安科生物参股公司博生吉、茂行生物、克睿基因、森朗生物对通用型CAR-T也有布局。亘喜生物UCAR-T管线有3个。靶向CD19的细胞疗法GC007g使用供者来源CAR技术,是国内第一款进入临床阶段的通用型CAR-T疗法,已在国内完成IIT临床试验。GC502是靶向CD19/CD7的双靶向UCAR-T产品,用于治疗急性B淋巴细胞白血病。GC027是靶向CD7的UCAR-T产品,用于治疗急性T淋巴细胞白血病。北恒生物UCAR-T管线达到7个,进度最快的TA101今年3月获得CDE临床试验默示许可,是国内首个基于CRISPR基因编辑技术的免疫细胞治疗产品,也是第二款进入临床阶段的通用型CAR-T疗法。科济生物UCAR-T管线有3个,KJ-C2111靶向BCMA,用于治疗多发性骨髓瘤(MM),目前处于IIT实验阶段,KJ-C2114目前还在临床前研究阶段。实体瘤CAR-T疗法覆盖面更广,也可通过规模化生产降低成本。2019年,全球癌症患者有1850万人,其中1730万是实体瘤患者,占比高达93%。科济药业核心产品CT041靶向Claudin18.2,用于治疗胃癌/食管胃结合部腺癌及胰腺癌,是全球首个且唯一进入到关键2期临床试验的实体瘤CAR-T,计划于2024年上半年向国内提交NDA,并计划今年下半年在北美启动一项2期临床试验。科济药业上半年亏损3.76亿元,现金储备27.4亿元,可支持4年以上的研发活动,控制成本能力比传奇生物更强。从市场表现看,其国内一线CAR-T企业的地位已得到认同。相比成熟的CAR-T疗法,NK细胞疗法还在早期阶段,但潜在优势突出,工业化量产潜力更大,适应症范围更广,安全性更好,成本更低,杀伤速度快,且可作为通用型现货产品。国内企业进行布局的有百济神州、优凯瑞、呈诺医学、重庆精准生物、阿思科力、科伦博泰、英百瑞、博生吉、再凌生物、星奕昂、贝斯生物、启函生物、恩凯赛药、景达生物、河络新图、昕传生物和济因生物。2021年11月,国家药监局审批通过国健呈诺现货型同种异体CAR-NK细胞产品的临床试验申请,为国内第一款进入临床阶段的NK细胞疗法。英百瑞用ADC思路开发细胞免疫疗法,在今年上半年NK细胞疗法领域融资金额以2.3亿元位列第一,2款产品即将进入IND。03 CGT
CDMO等待爆发契机下游CAR-T商业化缓慢,上游CGT CDMO仍处于培育期,需等到通用型CAR-T上市才能实现工业化放量。和元生物可能是国内唯一盈利的CGT CDMO,一度受到质疑,被担忧上市后财务数据变脸。今年Q2营收6178万元,同比增长17.9%,环比下降15.6%,净利润796万元,环比下降34%,虽受疫情影响,但业绩与二级市场的炒作热度严重不匹配。和元生物半年报也在淡化细胞疗法的概念,更突出自身聚焦基因治疗的定位,主要客户深圳亦诺微、上海复诺健、康华生物、北恒生物中,仅有一家是CAR-T企业。上半年CDMO业务累计新增订单超1.3亿元,在手未执行订单超3.5亿元,开拓干细胞、NK细胞和mRNA新型业务种类。博腾股份上半年CGT CDMO收入1127万元,同比增长80%,是唯一增速较快的,但规模尚小。服务客户32家,同比增长167%;新项目31个,同比增长244%;新签订单约9208万元,同比增长68%。博腾生物B轮融资5.2亿元,现有4000平方米的研发与生产基地稳健运营中,今年Q4预计新增16000平方米的大规模产业化基地,将拥有10条GMP病毒载体生产线、10条GMP细胞治疗生产线以及上百个洁净车间。启动海外市场拓展,部署在北美的工艺开发和分析检测实验室能力。药明康德上半年CGT CDMO收入6.15亿元,同比增长35.7%,经调整Non-IFRS毛利-0.43亿元,毛利率为-6.9%,处于亏损状态。毛利下跌主要由于新启用的上海临港运营基地较低的利用率导致。拥有51个临床前和I期临床试验项目,9个II期临床试验项目,7个III期临床试验项目(其中4个项目处于上市申请准备阶段)。康龙化成CGT CDMO处于整合和投入阶段,海外运营成本过高,暂时亏损。金斯瑞生物科技CGT CDMO平台(蓬勃生物)接近盈亏平衡,2021年新增6400平方米质粒GMP厂房,2022年、2023年国内分别新增6400平方米,2024年美国生产基地将增加3.1万平方米质粒及病毒GMP厂房。质粒方面,蓬勃生物是国内最大的质粒CDMO供应商,有9个中国、美国、韩国IND申报成功经验,超过70个IND申报用质粒CMC项目进行中;病毒载体方面,成功为多个细胞治疗以及Genetherapy提供慢病毒及AAV载体,累计有3个中国、美国IND申报成功经验,超过20个IND申报用病毒载体CMC项目进行中;mRNA质粒方面,几乎与国内所有的mRNA疫苗企业建立合作,与韩国和美国公司合作的mRNA疫苗项目也相继在韩国和日本获临床批件;DNA疫苗方面,提供质粒的CMC研究。药明生基、蓬勃生物是领先优势较大的国际化CGT CDMO龙头。封面图来源:123rf版权声明/免责声明本文为授权转载文章,版权归拥有者。仅供感兴趣的个人谨慎参考,非商用,非医用、非投资用。欢迎朋友们批评指正!衷心感谢!文中图片、视频为授权正版作品,或来自微信公共图片库,或取自公司官网/网络根据CC0协议使用,版权归拥有者。任何问题,请与我们联系(电话:13651980212。微信:27674131。邮箱:contact@drugtimes.cn)。衷心感谢!推荐阅读优时比就左乙拉西坦注射用浓溶液暂停进口进行回应眼内给药迎来新格局|脉络膜上腔微注射开启糖尿病性黄斑水肿治疗新时代谢雨礼博士 | 药物创新:more is different罗氏旗下基因泰克首次从中国创新药企获得潜在药物全球开发及商业化权益海阔凭药去,大道创新行! 2022第三届中国新药CMC高峰论坛与您再约上海!(第一轮通知)半年营收超10亿,复宏汉霖半年报业绩亮眼,彰显Biopharma实力中国需要自己的Flagship,多玛医药能做到吗?——专访多玛医药首席运营官黄蕤博士手握创新药项目的你,需要帮助吗?诺和诺德携手ATLATL为你点亮「星起点」...云顶退货,里面的「热闹」与「门道」在雷尼替丁的相关争议中,GSK放弃与Ideaya的一项实体瘤合作点击这里,报名参加第三届中国新药CMC高峰论坛!
免疫疗法细胞疗法基因疗法信使RNA合作
100 项与 University of Michigan Comprehensive Cancer Center 相关的药物交易
登录后查看更多信息
100 项与 University of Michigan Comprehensive Cancer Center 相关的转化医学
登录后查看更多信息
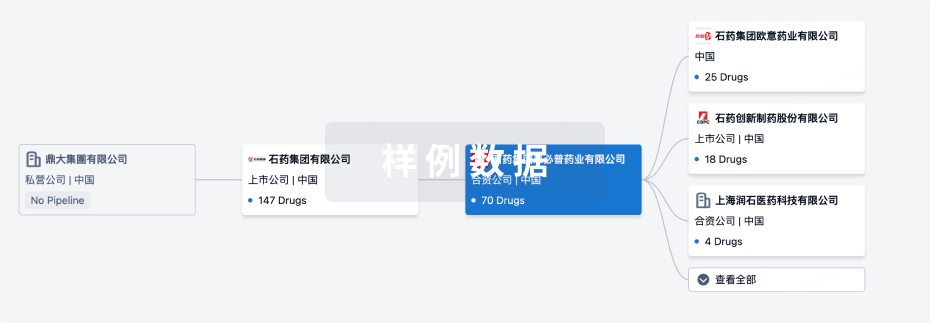
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年07月18日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
其他
3
登录后查看更多信息
当前项目
| 药物(靶点) | 适应症 | 全球最高研发状态 |
|---|---|---|
NSC-631939 ( RASGRP3 ) | 肿瘤 更多 | 无进展 |
Tasadenoturev ( Bcl-2 x TIM3 ) | 卵巢癌 更多 | 无进展 |
NSC 631941 ( RASGRP3 ) | 肿瘤 更多 | 无进展 |
登录后查看更多信息
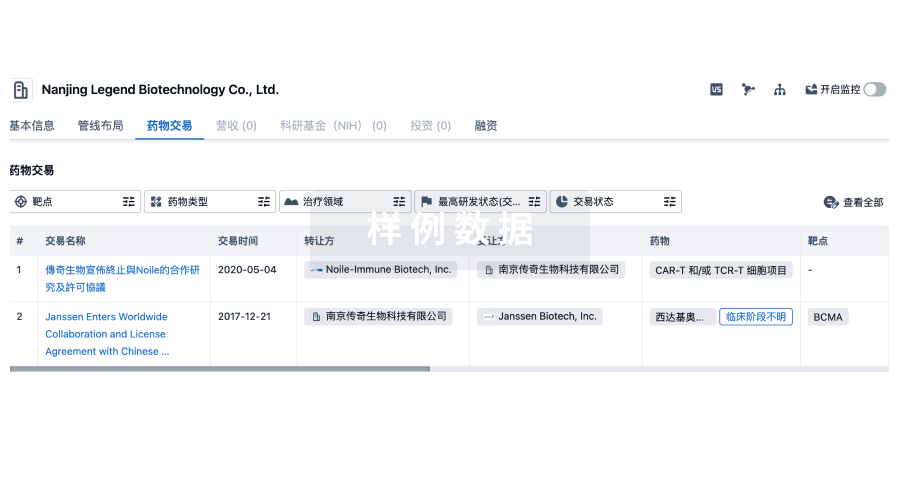
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
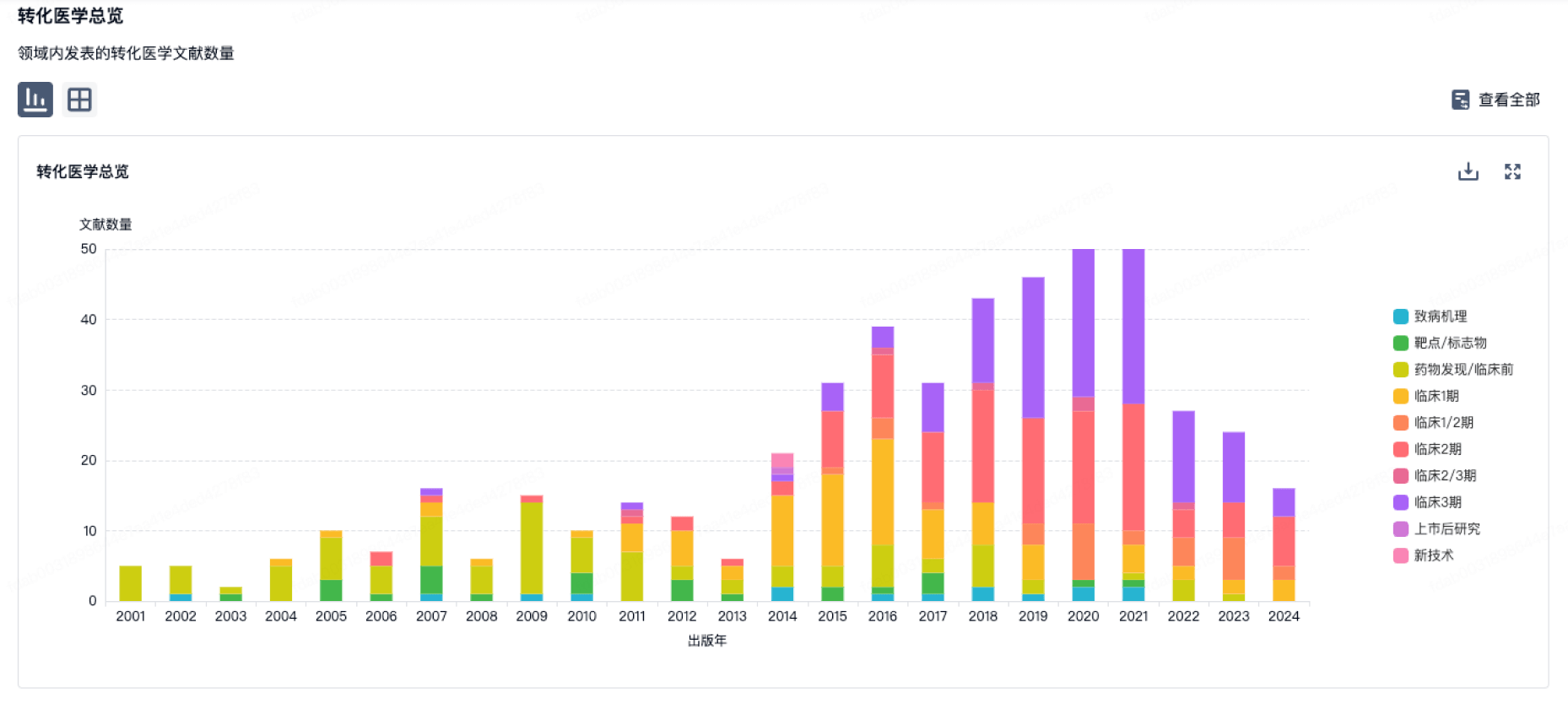
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
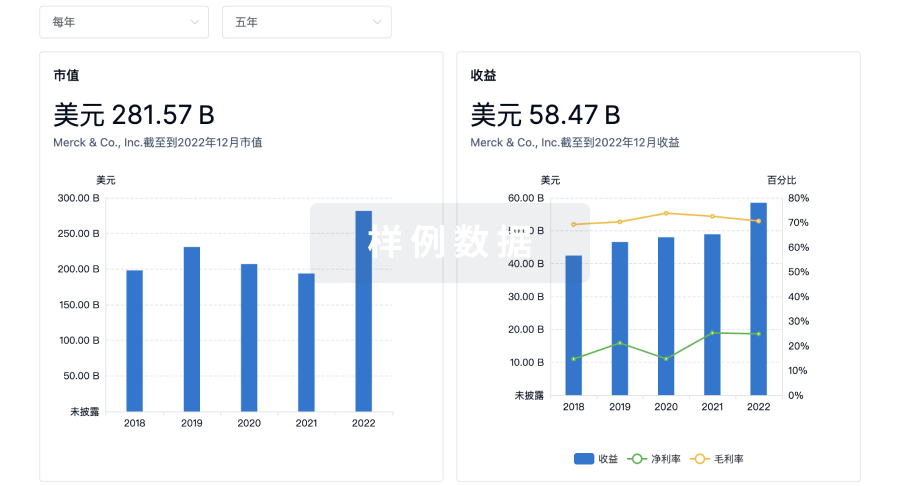
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用