预约演示
更新于:2025-05-07

Blue Cross & Blue Shield of North Carolina
更新于:2025-05-07
概览
关联
1
项与 Blue Cross & Blue Shield of North Carolina 相关的临床试验NCT05048836
Healthy Food First
Socioeconomic barriers to healthy eating, particularly food insecurity, are a major reason for poor blood pressure control and hypertension complications. Healthy diet patterns have been shown to improve health. Unfortunately, food insecurity makes it difficult for individuals to maintain healthy diet patterns. This pragmatic randomized trial will compare two food insecurity interventions (a healthy food subsidy versus a delivered food box), with or without lifestyle support delivered by community health workers, for 6 versus 12 months duration. Key outcomes include blood pressure, food insecurity, and other patient reported outcomes.
开始日期2021-10-07 |
申办/合作机构 |
100 项与 Blue Cross & Blue Shield of North Carolina 相关的临床结果
登录后查看更多信息
0 项与 Blue Cross & Blue Shield of North Carolina 相关的专利(医药)
登录后查看更多信息
35
项与 Blue Cross & Blue Shield of North Carolina 相关的文献(医药)2025-03-01·Journal of managed care & specialty pharmacy
Evaluating the uptake of a Global Initiative for Asthma guideline update in a commercially insured, value-based care population.
Article
作者: Smith, Spenser ; McInturff, Lindsey M
2024-02-01·The Gerontologist
Implementation Lessons Learned: Distress Behaviors in Dementia Intervention in Veterans Health Administration
Article
作者: Wray, Laura O ; Karel, Michele J ; Curyto, Kim ; Jedele, Jenefer M ; Sullivan, Jennifer L ; Minor, Lisa ; McConnell, Eleanor S
2023-12-26·Journal of the Pediatric Infectious Diseases Society
Trends in Pediatric Emergency and Inpatient Healthcare Use for Mental and Behavioral Health Among North Carolinians During the Early COVID-19 Pandemic
Article
作者: Brookhart, M Alan ; Zimmerman, Kanecia O ; CoyneSmith, Taran ; Charles, Catherine O ; Darden, Toni ; Benjamin, Daniel K ; Sielaty, Rachel ; Boutzoukas, Angelique E ; Overman, Robert A ; Caison, Bria
1
项与 Blue Cross & Blue Shield of North Carolina 相关的新闻(医药)2024-01-17
Tunde Sotunde, Blue Cross NC’s CEO: “With approximately half of FastMed’s clinics located in rural areas of our state with limited access to health care resources, I believe this is a vital investment in North Carolina.”
Blue Cross and Blue Shield of North Carolina has closed a deal to scoop up 55 FastMed urgent care clinics operating in the Tarheel State.
The insurer said that a dearth of providers in rural areas spurred it to acquire the clinics in that state, which are location in 34 counties in the state, according to an announcement. FastMed offers preventive care, telehealth, primary care and occupational care.
Blue Cross NC previously unveiled plans to buy the clinics in October.
"As I’ve traveled across North Carolina and listened, it is clear that access to basic primary care services is a critical need," said Tunde Sotunde, CEO of Blue Cross NC, in a press release. "With approximately half of FastMed’s clinics located in rural areas of our state with limited access to health care resources, I believe this is a vital investment in North Carolina.”
One of Blue Cross NC's first priorities is to address the staffing challenges and scaled-back service hours caused by pressures on the health care workforce statewide, according to plan officials. Blue Cross NC and FastMed will collaborate on ways to further enhance the patient experience, improve dependability for our members and communities, and stabilize the existing health are workforce.
Blue Cross NC said it wants to spread a wide net, saying that FastMed locations will offer treatment to any North Carolinian or visitors to the state regardless of what insurance they may have.
The company also wasted no time in choosing who will lead the effort, appointing Jim Moffett as FastMed’s CEO. The press release says that Moffett has a background in leading ambulatory providers, including primary care and urgent care businesses.
Moffett has more than two decades in an executive capacity with various mission-driven and customer-focused organizations, according to the release.
"Under the leadership of Jim Moffett, I am confident our two organizations, Blue Cross NC and FastMed, can realize our commitment to improving access to quality care for all North Carolinians," Sotunde said.
The COVID-19 pandemic led to a significant thinning of the ranks of providers nationwide. North Carolina, for example, lost about 9% of its direct care workforce between 2016 and 2021. Blue Cross NC said in the release that building up FastMed's capabilities is a key focus.
“As the health care industry continues to change rapidly, new partnerships and affiliations to improve patient health and lower health care costs are more commonplace,” the press release said. “Blue Cross NC’s short-term plans for FastMed include returning to pre-pandemic service operations and investing in ways to further enhance the patient experience.”
Acquiring FastMed's urgent care clinics is just one of the recent moves Blue Cross NC has made to attempt to expand the reach of its services. Earlier this month, the health plan announced that it will allow early prescription refills in anticipation of severe weather conditions to ensure that members have access to needed medications. That effort will be in effect until February 7, 2024.
Blue Cross NC also decreased the cost of premiums for its Affordable Care Act plans by 4%. The cuts are expected to lower total premiums for those plans by about $130 million this year.
高管变更
100 项与 Blue Cross & Blue Shield of North Carolina 相关的药物交易
登录后查看更多信息
100 项与 Blue Cross & Blue Shield of North Carolina 相关的转化医学
登录后查看更多信息
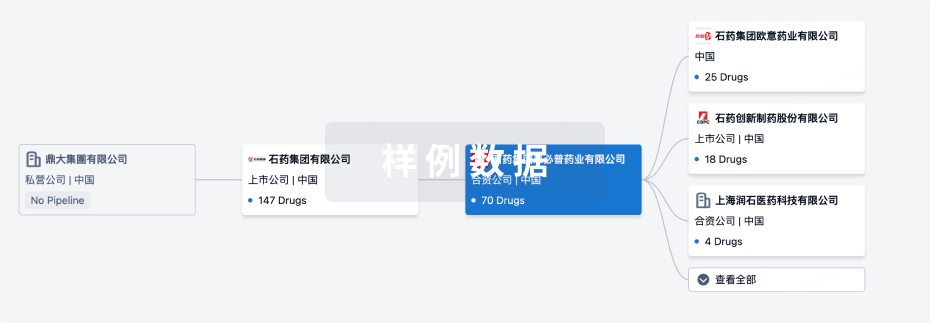
组织架构
使用我们的机构树数据加速您的研究。
登录
或
管线布局
2025年07月06日管线快照
无数据报导
登录后保持更新
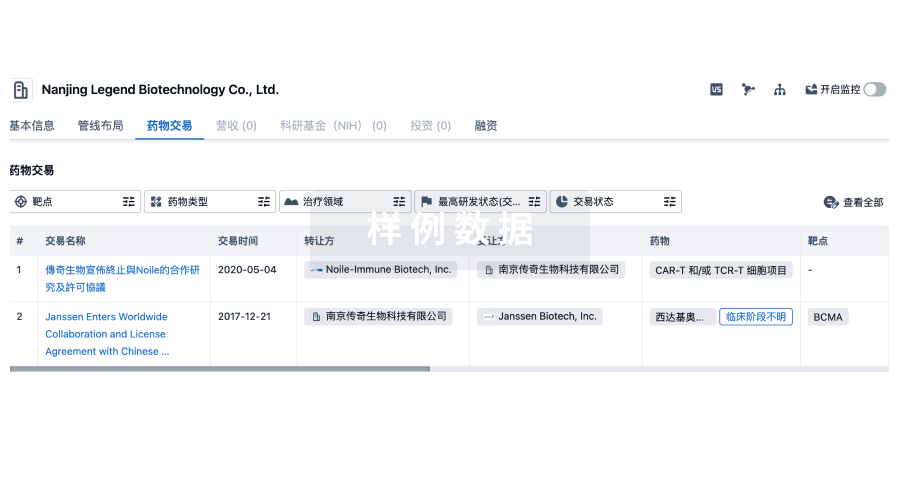
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
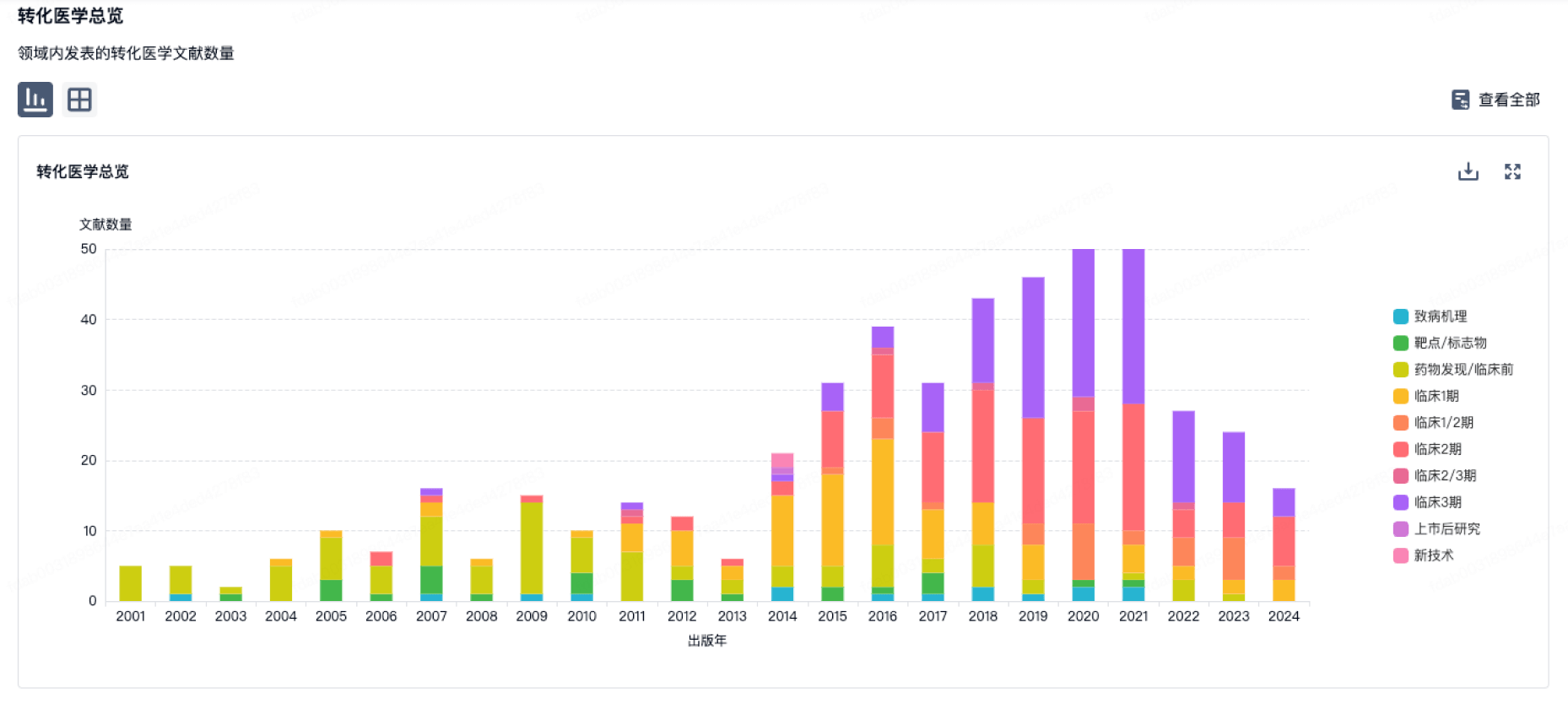
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
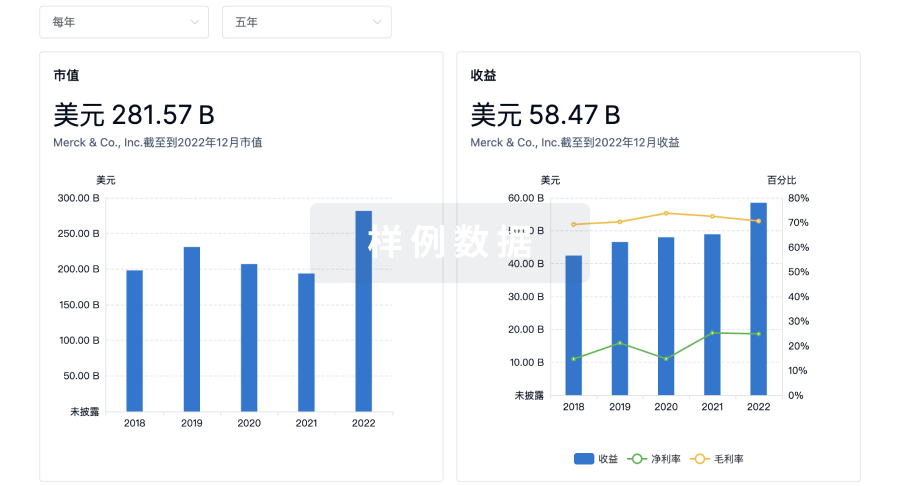
营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或
科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

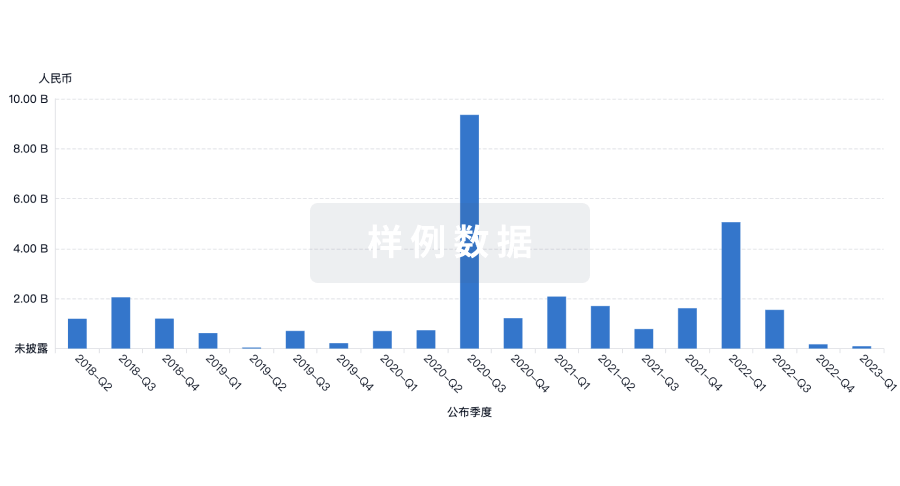
投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或
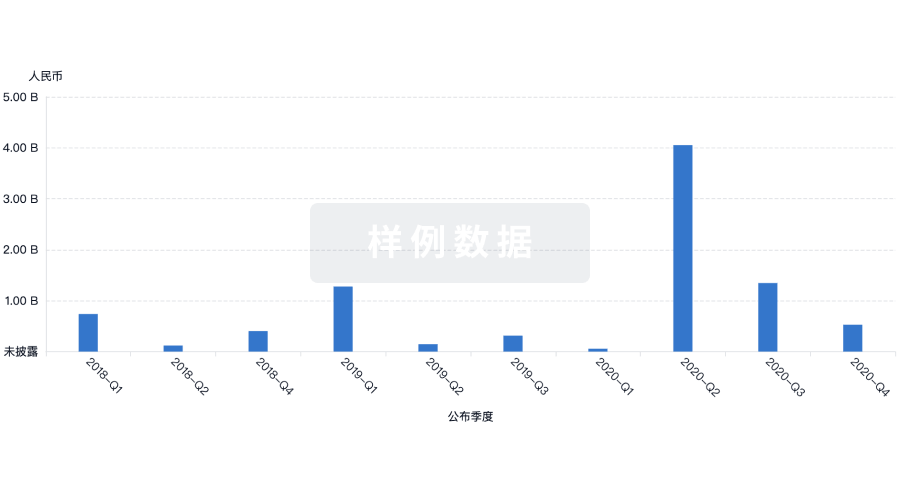
融资
发掘融资趋势以验证和推进您的投资机会。
登录
或
Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用