预约演示
更新于:2025-05-07
Lais
更新于:2025-05-07
概要
基本信息
原研机构 |
在研机构 |
非在研机构- |
权益机构- |
最高研发阶段批准上市 |
首次获批日期 意大利 (2001-05-17), |
最高研发阶段(中国)- |
特殊审评- |
登录后查看时间轴
关联
7
项与 Lais 相关的临床试验EUCTR2019-001532-65-IT
A prospective, multicenter, double-blind, placebo-controlled randomized study to assess efficacy and safety of LAIS® Grass pollen tablets in patients with seasonal grass pollen-induced allergic rhinoconjunctivitis - LAIS® Grass pollen tablets in seasonal grass pollen-induced allergic rhinoconjunctivitis
开始日期2019-09-12 |
申办/合作机构- |
EUCTR2017-005079-21-DE
A Prospective, Multicenter, Double-Blind, Placebo-Controlled, Dose-Finding Phase-II Study for the Efficacy and Safety of LAIS® House Dust Mites Sublingual Tablets in Patients with Mite-Induced Allergic RhinoConjunctivitis Without or With Controlled Asthma using a Titrated Nasal Provocation Test model.
开始日期2018-08-23 |
申办/合作机构- |
EUCTR2016-003439-39-DE
A Prospective, Multicenter, Double-Blind, Placebo-Controlled, Dose-Finding Phase-II Study for the Efficacy and Safety of LAIS® House Dust Mites Sublingual Tablets in Patients with Mite-Induced Allergic Rhino-Conjunctivitis Without or With Controlled Asthma in an Allergen Exposure Chamber (AEC)
开始日期2017-05-22 |
申办/合作机构- |
100 项与 Lais 相关的临床结果
登录后查看更多信息
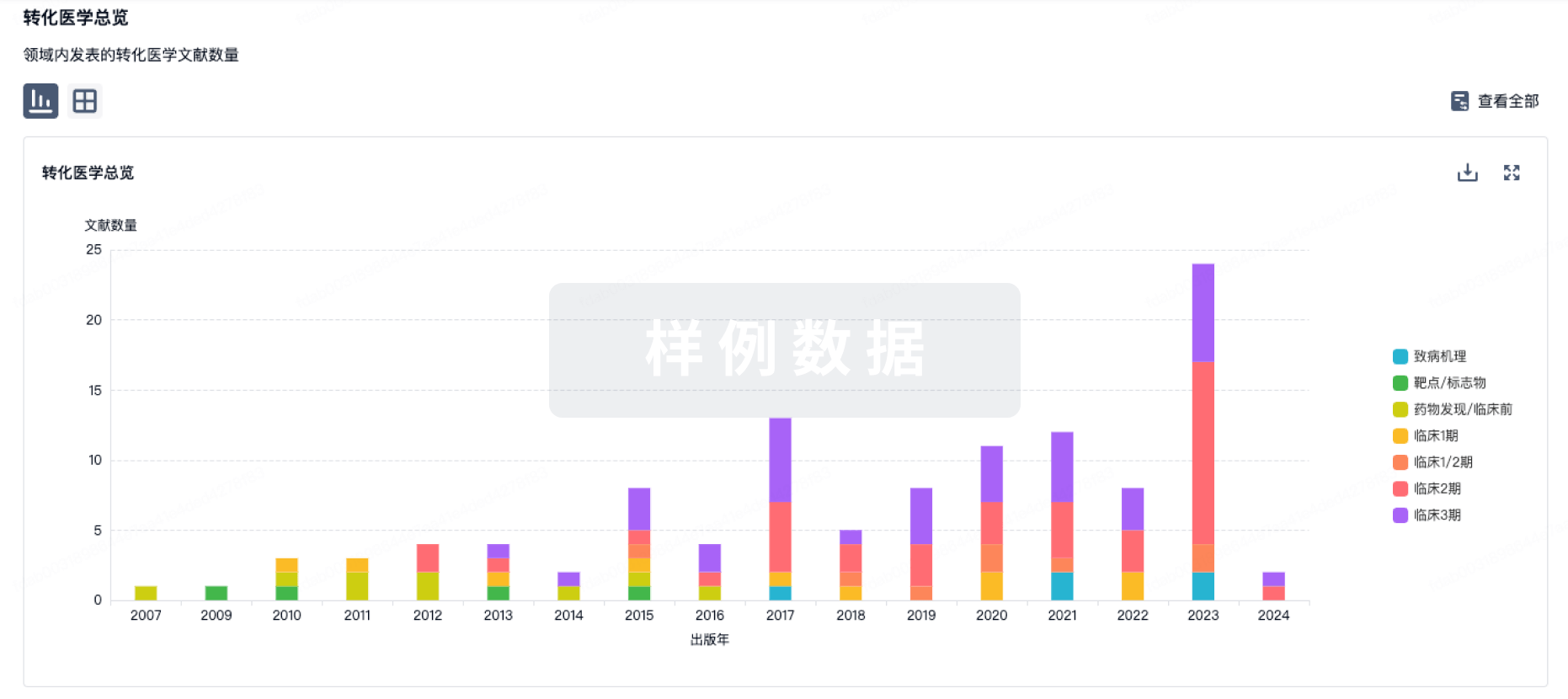
100 项与 Lais 相关的转化医学
登录后查看更多信息
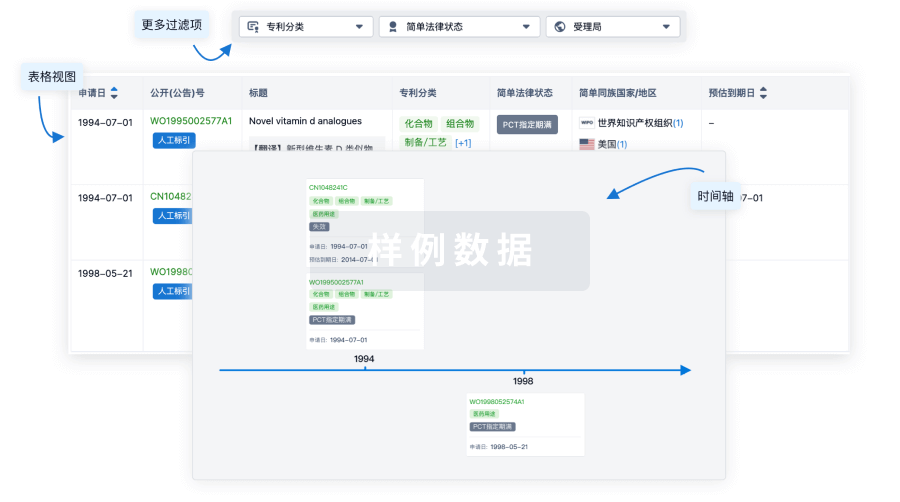
100 项与 Lais 相关的专利(医药)
登录后查看更多信息
153
项与 Lais 相关的文献(医药)2025-06-01·Psychiatry Research
Real-world outcomes and practice patterns among patients with schizophrenia when switched from oral antipsychotics to long-acting injectable formulations after hospitalization
Article
作者: Casciano, Julian ; Thompson, Stephen ; Kane, John M ; Dotiwala, Zenobia ; Philbin, Michael J ; Franzenburg, Kelli R ; Iii, Rolf T Hansen ; Rubio, Jose M
2025-04-01·Psychiatry Research
Latent variable analysis of adherence to antipsychotics among South Carolina medicaid beneficiaries with schizophrenia or schizoaffective disorder
Article
作者: Benson, Carmela ; Cai, Chao ; Patel, Charmi ; Kozma, Chris ; Yunusa, Ismaeel ; Zhao, Pujing ; Reeder, Gene
2025-03-01·Journal of Child and Adolescent Psychopharmacology
Long-Acting Injectable Antipsychotic Medication Use in Youth: A Systematic Review of the Literature Along with MedWatch Safety Data and Prescriber Attitudes
Review
作者: Sieracki, Rita ; Mireski, Sarah J. ; Scharko, Alexander M.
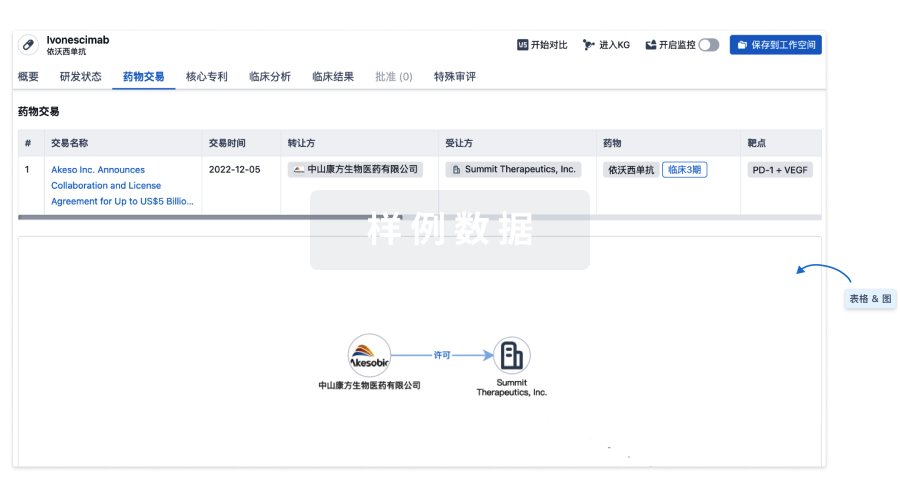
100 项与 Lais 相关的药物交易
登录后查看更多信息
研发状态
10 条最早获批的记录, 后查看更多信息
登录
| 适应症 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|
| 超敏反应 | 意大利 | 2001-05-17 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或

批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
