预约演示
更新于:2025-05-07
Albumin (Human)(Octapharma)
更新于:2025-05-07
概要
基本信息
非在研机构- |
最高研发阶段批准上市 |
首次获批日期 美国 (2006-10-17), |
最高研发阶段(中国)批准上市 |
特殊审评- |
登录后查看时间轴
关联
100 项与 Albumin (Human)(Octapharma) 相关的临床结果
登录后查看更多信息
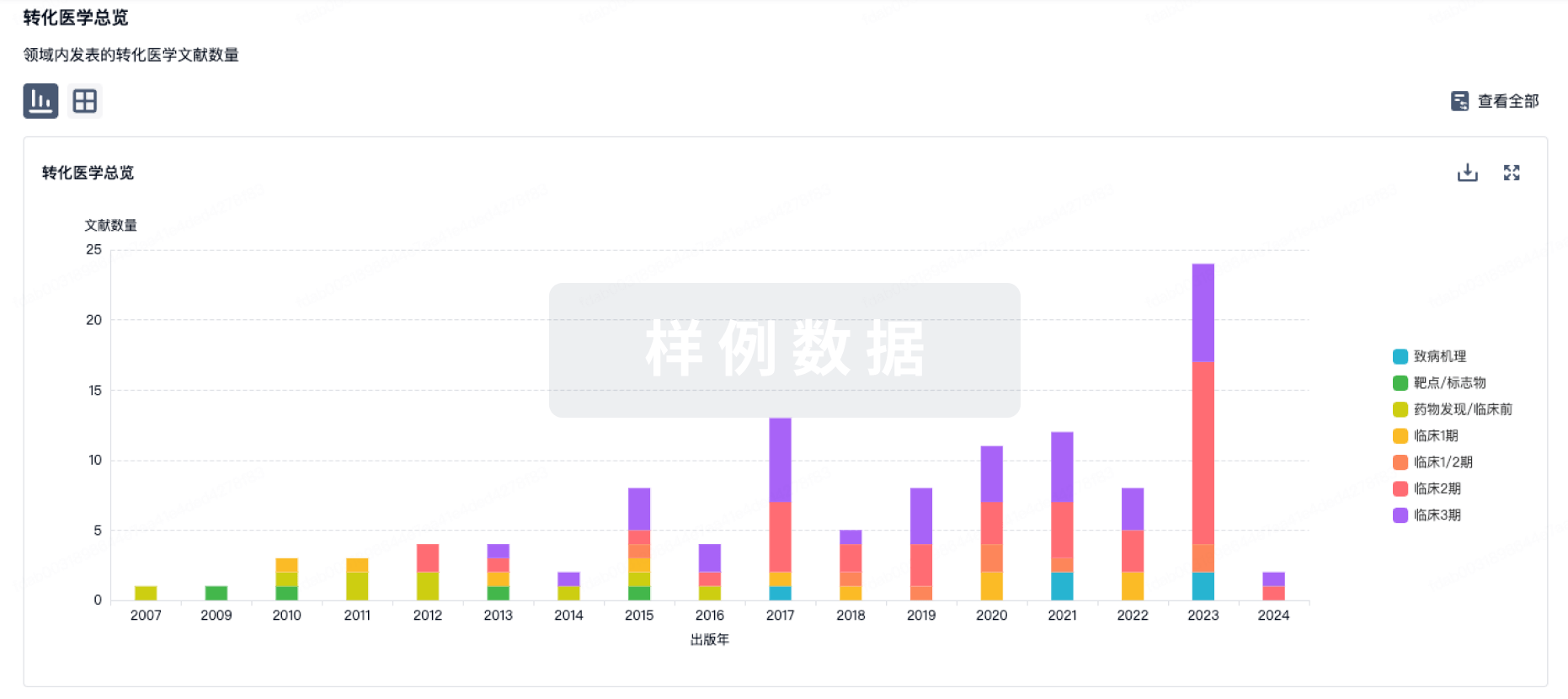
100 项与 Albumin (Human)(Octapharma) 相关的转化医学
登录后查看更多信息
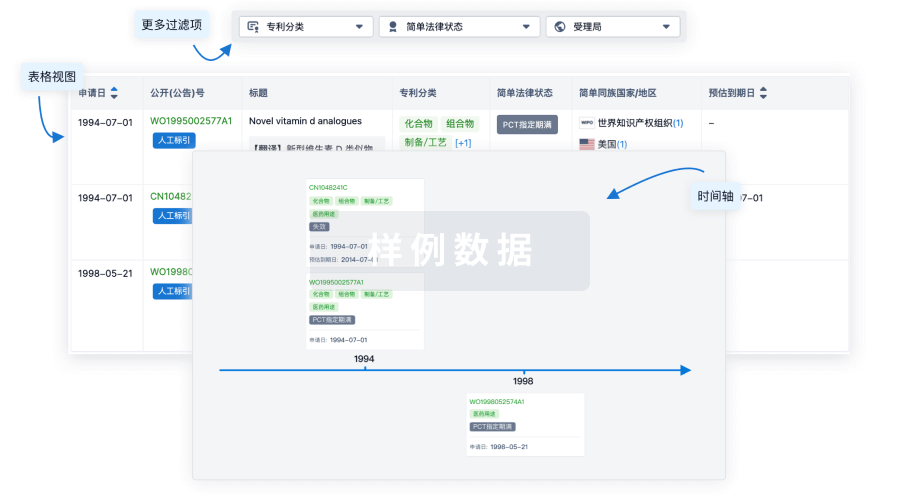
100 项与 Albumin (Human)(Octapharma) 相关的专利(医药)
登录后查看更多信息
1
项与 Albumin (Human)(Octapharma) 相关的文献(医药)Transfusion Medicine and Hemotherapy
Effect of Selected Crystalloid and Colloid Solutions on Coagulation Status Evaluated by Rotational Thromboelastometry and Platelet Function Analyser: An in vitro Study
Article
作者: Jonas, Jakub ; Vymazal, Tomas ; Durila, Miroslav
49
项与 Albumin (Human)(Octapharma) 相关的新闻(医药)2025-03-08
·药闻康策
☝ 点击上方 一键预约 ☝
最新最热的医药健康新闻政策
本共识以规范临床用药行为、促进合理用药为工作目标,对纳入《目录》中的奥美拉唑、人血白蛋白、左氧氟沙星、法莫替丁等30种药品中常见的超说明书用药情况进行评估,明确临床应用条件和原则,以利于加强合理用药监管,促进临床合理用药水平持续提高。
01
质子泵抑制剂
推荐意见1:治疗伴胃黏膜糜烂和(或)以反酸、上腹痛等症状为主的慢性胃炎。证据质量:B;推荐等级:强推荐。
《中国慢性胃炎共识意见(2017年,上海)》推荐有胃黏膜糜烂和(或)以上腹痛和上腹烧灼感等症状为主的慢性胃炎患者,可根据病情或症状严重程度选用胃黏膜保护剂、抗酸剂、H2受体抑制剂或PPIs(推荐等级:强;证据质量:A)。包括奥美拉唑、艾司奥美拉唑、雷贝拉唑、兰索拉唑、泮托拉唑和艾普拉唑等在内的PPIs抑酸作用强而持久,可根据病情或症状严重程度选用。
《质子泵抑制剂优化应用专家共识》中建议有黏膜糜烂和(或)酸相关症状的慢性胃炎患者,可根据病情酌情选用PPIs,推荐常规剂量每日1次PPIs,疗程4~6周(推荐等级:强;证据质量:B)。
推荐意见2:以上腹痛、灼烧感为主要症状的功能性消化不良 本条中:奥美拉唑说明书有消化不良适应症,其他PPI(证据质量:艾司奥美拉唑A,兰索拉唑A,雷贝拉唑A,泮托拉唑B;推荐等级:强推荐)。
推荐意见3:用于长期治疗病理性胃酸分泌过多症(如卓-艾综合征)(证据质量:艾司奥美拉唑A;推荐等级:强推荐)。其他PPIs说明书有卓-艾综合征的适应症。
推荐意见4:与抗菌药物联合,根除Hp感染 (证据质量:兰索拉唑A;推荐等级:强推荐)。其他PPIs说明书中有该适应症。
推荐意见5:与阿莫西林联合,大剂量二联方案根除Hp感染 (证据质量:艾司奥美拉唑A,雷贝拉唑A;推荐等级:强推荐)。
《2022中国幽门螺杆菌感染治疗指南》中提出铋剂四联方案和大剂量双联方案均可用于Hp感染初次和再次根除治疗(弱推荐,低质量),大剂量阿莫西林(≥3g·d-1,如每次1g、tid,或每次0.75 g、qid)联合PPIs,如艾司奥美拉唑或雷贝拉唑(双倍标准剂量,bid;或标准剂量,qid)。
《2017ACG临床指南:幽门螺杆菌感染的治疗》中也建议大剂量二联方案(PPIs和阿莫西林联合使用14d)可作为挽救方案,PPIs(标准剂量或双倍剂量,tid或qid)+阿莫西林(1g,tid或0.75g,qid)。
推荐意见6:用于治疗GERD相关的咽喉反流性疾病患者(证据质量:奥美拉唑B、兰索拉唑B、艾司奥美拉唑B、雷贝拉唑B;推荐等级:强推荐)。
《咽喉反流性疾病诊断与治疗专家共识》提出药物治疗是治疗LPRD的主要方法,包括PPIs、钾离子竞争性酸拮抗剂、H2受体阻断剂、促胃肠动力药和胃黏膜保护剂等(中等质量证据,强推荐)。
推荐意见7:用于治疗儿童Hp感染 (证据质量:奥美拉唑A,艾司奥美拉唑B;推荐等级:强推荐)。
推荐意见8:儿童胃食管反流病 (所有PPIs证据质量:A;推荐等级:强推荐)。
推荐意见9:儿童功能性消化不良 (证据质量:奥美拉唑C;推荐等级:弱推荐)。
推荐意见10:儿童消化道出血 (证据质量:奥美拉唑C;推荐等级:弱推荐)。
推荐意见11:儿童消化性溃疡 (证据质量:奥美拉唑B;推荐等级:强推荐)。
02
抗菌药物
推荐意见12:头孢他啶用于治疗类鼻疽 (证据质量:A级;推荐等级:强推荐)。
推荐意见13:美罗培南用于感染诱发的老年多器官功能障碍综合征的经验性抗感染治疗 (证据质量:B级;推荐等级:强推荐)。
推荐意见14:
(1)左氧氟沙星用于感染性腹泻的经验性治疗 (证据质量:B;推荐等级:强推荐)。
(2)利福平耐药、异烟肼耐药或异烟肼和利福平耐药结核病治疗的长程治疗 (证据质量:B;推荐等级:强推荐)。
(3)高危的粒细胞缺乏患者的感染预防 (证据质量:A;推荐等级:强推荐)。
(4)Hp感染初次和再次根除治疗的四联方案 (证据质量:B;推荐等级:强推荐)。
03
糖皮质激素
推荐意见15:雾化吸入布地奈德可作为慢性阻塞性肺疾病急性加重住院患者的全身性糖皮质激素的替代治疗(证据质量:A;推荐等级:强推荐)。
推荐意见16:雾化吸入布地奈德在某些特定人群中可在支气管舒张剂基础上联合治疗慢阻肺急性加重的住院患者(证据质量:B;推荐等级:强推荐)。
推荐意见17:患新型冠状病毒感染(COVID-19)的儿童,若合并急性喉炎或喉气管炎者,可给予布地奈德2mg雾化吸入(证据质量:A;推荐等级:强推荐)。
推荐意见18:患COVID-19的儿童,若存在喘息、肺部哮鸣音:可在综合治疗的基础上加用布地奈德2mg雾化吸入(证据质量:A;推荐等级:强推荐)。
推荐意见19:患COVID-19的高风险人群(老年人及合并有并发症人群)可使用吸入布地奈德进行治疗(证据质量:B;推荐等级:强推荐)。
推荐意见20:COVID-19患者在发病早期可使用吸入布地奈德进行治疗(证据质量:B;推荐等级:强推荐)。
推荐意见21:吸入布地奈德可用于治疗成人和青少年患者非哮喘性嗜酸性支气管炎引起慢性咳嗽(证据质量:B;推荐等级:强推荐)。
推荐意见22:雾化布地奈德(2mg)用于严重儿童喉炎患者的辅助治疗(证据质量:B;推荐等级:强推荐)。
推荐意见23:用于儿童急性鼻窦炎的辅助治疗(证据质量:B;推荐等级:强推荐)。
推荐意见24:布地奈德可用于合并相关疾病的ICU患者有气道炎症时机械通气雾化吸入治疗(证据质量:D;推荐等级:弱推荐)。
推荐意见25:布地奈德雾化吸入可用于肺部手术围术期缓解气道炎症,加快手术康复(证据质量:D;推荐等级:弱推荐)。
04
其他临床治疗药物
推荐意见26:罂粟碱用于男子勃起功能障碍的替代治疗(证据质量:B级;推荐等级:弱推荐)
推荐意见27:罂粟碱用于治疗急性肠系膜缺血(证据质量:B级;推荐等级:强推荐)
推荐意见28:前列地尔用于勃起功能障碍的诊断和治疗(证据质量:A;推荐等级:强推荐)。
推荐意见29:前列地尔用于治疗糖尿病足(证据质量:A;推荐等级:强推荐)。
推荐意见30:法莫替丁用于治疗以上腹痛、烧灼感为主要症状的功能性消化不良(证据质量:A;推荐等级:强推荐)。
推荐意见31:法莫替丁用于治疗伴胃黏膜糜烂和(或)以反酸、上腹痛等症状为主的慢性胃炎(证据质量:B;推荐等级:强推荐)。
《中国慢性胃炎共识意见(2017年,上海)》推荐有胃黏膜糜烂和(或)以上腹痛和上腹烧灼感等症状为主的慢性胃炎患者,可根据病情或症状严重程度选用胃黏膜保护剂、抗酸剂、H2受体拮抗剂或PPIs(推荐等级:强;证据质量:高)。
推荐意见32:人血白蛋白用于卵巢过度刺激综合征(证据质量:A;推荐等级:强推荐)。
推荐意见33:人血白蛋白用于预防成人腹腔穿刺大量放液后的循环功能障碍(证据质量:A;推荐等级:强推荐)。
推荐意见34:人血白蛋白用于联合抗菌药物减少自发性细菌性腹膜炎后的肾损害(证据质量:B;推荐等级:强推荐)。
推荐意见35:人血白蛋白用于肝脏功能衰竭患者人工肝支持系统(证据质量:B;推荐等级:强推荐)
(来源: 医药 ZS 公众号)
药闻康策
新媒体矩阵微信公众号
点击下方 一键关注
【免责声明】
1.“药闻康策”部分文章信息来源于网络转载是出于传递更多信息之目的,并不意味着赞同其观点或证实其内容的真实性。如对内容有疑议,请及时与我司联系。2.“药闻康策”致力于提供合理、准确、完整的资讯信息,但不保证信息的合理性、准确性和完整性,且不对因信息的不合理、不准确或遗漏导致的任何损失或损害承担责任。3.“药闻康策”所有信息仅供参考,不做任何商业交易或医疗服务的根据,如自行使用“药闻康策”内容发生偏差,我司不承担任何责任,包括但不限于法律责任,赔偿责任。
欢迎转发分享、点赞、点在看
临床结果临床2期
2024-11-08
编辑:子非鱼
江苏第5轮集采发布1号公告,75个西药、9组中成药纳入。拟中选规则主要依据在外省集采是否中选,其中选价与本省挂网价比价,就低不就高;对于流标非独家品种,增加一轮竞价迫使其再次降价,或暂停挂网;采购量分配也体现了量价挂钩原则。本次集采周期为2年。
11月8日,江苏省医保局发出《江苏省第五轮药品集中带量采购公告(一)》(以下称为《1号公告》),正式标着个该第五轮药品集采正式启动,75个西药、9个中成药纳入集采。(名单见文末)。资质材料、省级集采最低价申报时间:2024年11月8日—14日17:00。逾期申报不予受理。
采购品种
通过对江苏省药品和医用耗材招采管理系统(以下简称“省招采子系统”)已挂网药品采购数据的梳理,经专家论证,从未纳入国家组织药品集中带量采购但已在外省集采降价的药品中,筛选确定省第五轮药品带量采购品种,详见文末表格。共75个西药(包括人血白蛋白等生物药)、9组中成药。
《1号公告》在报名资格方面,特别指出:
(1)申报企业应如实申报省级挂网最低价和省级集采最低价,并按照本公告和省招采子系统的要求提交申报材料,申报材料应对本公告提出的要求和条件做出响应。若申报企业未如实申报省级挂网最低价和省级集采最低价,或不具备申报资格中规定必须满足的全部要求,或涉嫌提供虚假证明材料,一经确认,将被视为无效申报;情节严重的,列入“违规名单”,并作出相应处理。
(2)申报企业、药品生产企业和药品上市许可持有人,当前在我省医药价格和招采信用评价失信等级为“特别严重”的,不得参与本次采购申报。
(3)申报企业、药品生产企业和药品上市许可持有人,当前在我省医药价格和招采信用评价失信等级为“严重”的,其涉案产品不得参与本次采购申报。
(4)申报企业、药品生产企业和药品上市许可持有人,当前在我省医药价格和招采信用评价失信等级为“中等”及以上的,不参与优先量分配。
(5)除血液制品外,其余品种同品种申报企业中,存在企业负责人为同一人或存在直接控股、管理关系的不同企业,或为同一集团内企业的,视为存在关联关系。关联关系企业,可自愿组成联合体,授权其中一家企业为代表进行联合申报,否则仅报价最低的一家企业(报价最低的企业出现2家及以上时,以挂网价格低的优先)视为有效申报。如联合体内被授权企业中选,联合体内所有企业同时中选;如联合体内被授权企业未中选,联合体内所有企业同时未中选。
(6)本次药品集中采购供应的药品,应包含临床常用包装。注射剂供应产品的包装材料应与报价代表品一致。
(7)申报企业中选后,须按要求签订购销协议。
(8)中选药品在履行协议中如遇不可抗力,直接影响协议履行的,由签订购销协议中的各方协商解决。
意向采购量和采购周期
原则上以各品种全省公立医疗机构(含军队驻苏医疗机构,下同)申报的下一采购年度需求量的80%(抗生素类、国家重点监控品种为50%)为意向采购量(见附件1)。
本次药品集中带量采购周期为2年,必要时可延长。采购周期内若提前完成任务,超出部分的用药需求,中选企业应按中选价继续进行供应,直至采购周期届满。采购周期内,如中选药品纳入国家集采,执行国家集采结果。
中选规则
(一)西药中选规则
根据申报企业同品种(指同通用名同医保合并归类剂型,下同)在外省集采中是否有中选(备选)记录,按如下规则确定拟中选企业(不同规格包装产品,挂网价和集采最低价均取按差比价规则换算后最低值):
1.有外省(区、市,以下简称“外省”,下同)集采中选(备选)记录产品。报价不高于本产品我省挂网价(无我省挂网价产品,取该产品外省挂网最低价和同品种省招采子系统挂网最低价两者中的低值;下同)和外省集采最低中选(备选)价的,拟中选。
2.无外省集采中选(备选)记录产品。报价不高于本产品我省挂网价且不高于同品种其他产品外省集采最低中选价中最高值的,拟中选。
(二)中成药中选规则
根据申报企业同品种在外省集采中是否有中选(备选)记录,按如下规则确定拟中选企业,涉及不同剂型规格包装价格比较时,换算成日均治疗费用后再进行价格比较:
1.有外省集采中选(备选)记录产品。报价不高于本产品我省挂网价和外省集采最低中选(备选)价的,拟中选。
2.无外省集采中选(备选)记录产品。
(1)同品种有外省集采中选记录的,报价不高于本产品我省挂网价且不高于同品种其他产品外省集采最低中选价中最高值的,拟中选。
(2)同品种无外省集采中选记录的,报价不高于本产品我省挂网价且不高于同采购组其他产品外省集采最低中选价中最高值。
(3)本次中选产品,如在执行期内出现省级集采中选价或省级挂网价低于本次中选价格的,企业应在上述省级集采中选价或省级挂网价执行后20个工作日内,主动申请就低调整中选价格,否则取消中选资格。
异常采购情况处理
1. 独家品种流标。流标独家品种将在平台予以单独标识,其采购情况纳入重点监测范围并定期通报。公立医疗机构采购流标品种时应予以报告说明,对采购流标独家品种金额排名靠前的将予以约谈。
2. 非独家品种流标。对流标的非独家品种,增加一轮竞价,同品种所有参与企业合为一组进行竞价,由专家研究制定最高有效申报价,有效报价中价格最低的1家企业拟中选,最低报价企业2家及以上时,2023年度省招采子系统采购量大的企业优先。对重新竞价后仍然流标的非独家品种,同品种近1个月有省招采子系统采购验收记录的挂网企业中,价格最低的1家拟中选,其余企业在采购周期内暂停挂网。
3. 对在省招采子系统有多家企业挂网的品种,如在本次集采中出现最终有效参与企业仅1或有效报价企业仅家1的,或出现其他导致竞争不充分情况的,视为异常采购情形,由专家根据历史采购情况和挂网情况等研究处置。
意向采购量分配
坚持带量采购、量价挂钩,在中选产品确定后,将意向采购量按以下规则分配给中选企业:
1. 独家品种的意向采购量按以下规则进行分配:在省级集采最低价省份中选的,带同品种意向采购量;在省级集采最低价省份备选的,仅中选不带量,在此基础上继续降价,降幅达到所有独家品种拟中选企业平均降幅的,带意向采购量。
2. 非独家品种的意向采购量按以下规则进行分配:
第一步,中选价格由低至高排名前50%(四舍五入取整)的企业,获得医疗机构对其所报意向采购量作为优先量。在确定获得优先量的企业时,如价格由低至高排名前50%企业中,末位价格相同的企业数超过剩余优先量企业名额时,按以下次序确定优先量企业:(1)上一年度省招采子系统验收量大的优先;(2)省招采子系统挂网价低(无挂网价的,取其外省挂网最低价)的优先。
第二步,医疗机构对未中选企业和其余中选企业所报意向采购量作为剩余量,由医疗机构结合临床需求,分配给同品种中质优价宜的中选产品,但中选价格由高至低排名前20%(向上取整,末位价格出现2家及以上的全部纳入)的企业(中选价格不高于同品种最低中选价1.3倍的企业除外),获得的量不可超过医疗机构对其所报意向采购量的70%。如同一品种的优先量企业与中选价格排名由高至低排名前20%企业出现重叠的,以优先量企业身份为准。
关注公众号,获取可靠、专业的资讯和分析内容
带量采购
2024-11-08
·药筛
刚刚,江苏公布5批集采目录,75个西药,9个中药,很多重磅爆品,如:人血白蛋白、乙酰半胱氨酸、肾康注射液、四磨汤等。
这次江苏动真格的了。
我会持续更进,尽快跟新相关数据到药数包微信服务号。
十批国采分享微信群已建,欢迎企业和代理商入群,对接资源,先到先得了。
加客服小狐微信,拉你入群!
带量采购
100 项与 Albumin (Human)(Octapharma) 相关的药物交易
登录后查看更多信息
研发状态
10 条最早获批的记录, 后查看更多信息
登录
| 适应症 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|
| 血容量不足 | 美国 | 2006-10-17 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或

核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

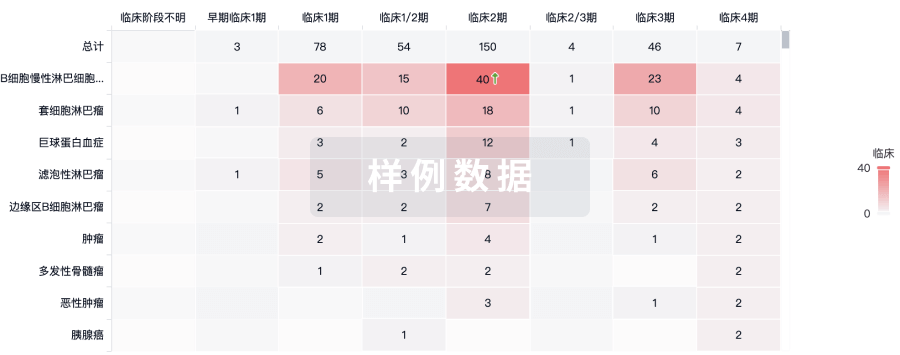
生物类似药
生物类似药在不同国家/地区的竞争态势。请注意临床1/2期并入临床2期,临床2/3期并入临床3期
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用

