预约演示
更新于:2025-01-23
NSAID(University of Turin)
更新于:2025-01-23
概要
基本信息
非在研机构- |
最高研发阶段临床前 |
首次获批日期- |
最高研发阶段(中国)- |
特殊审评- |
关联
100 项与 NSAID(University of Turin) 相关的临床结果
登录后查看更多信息
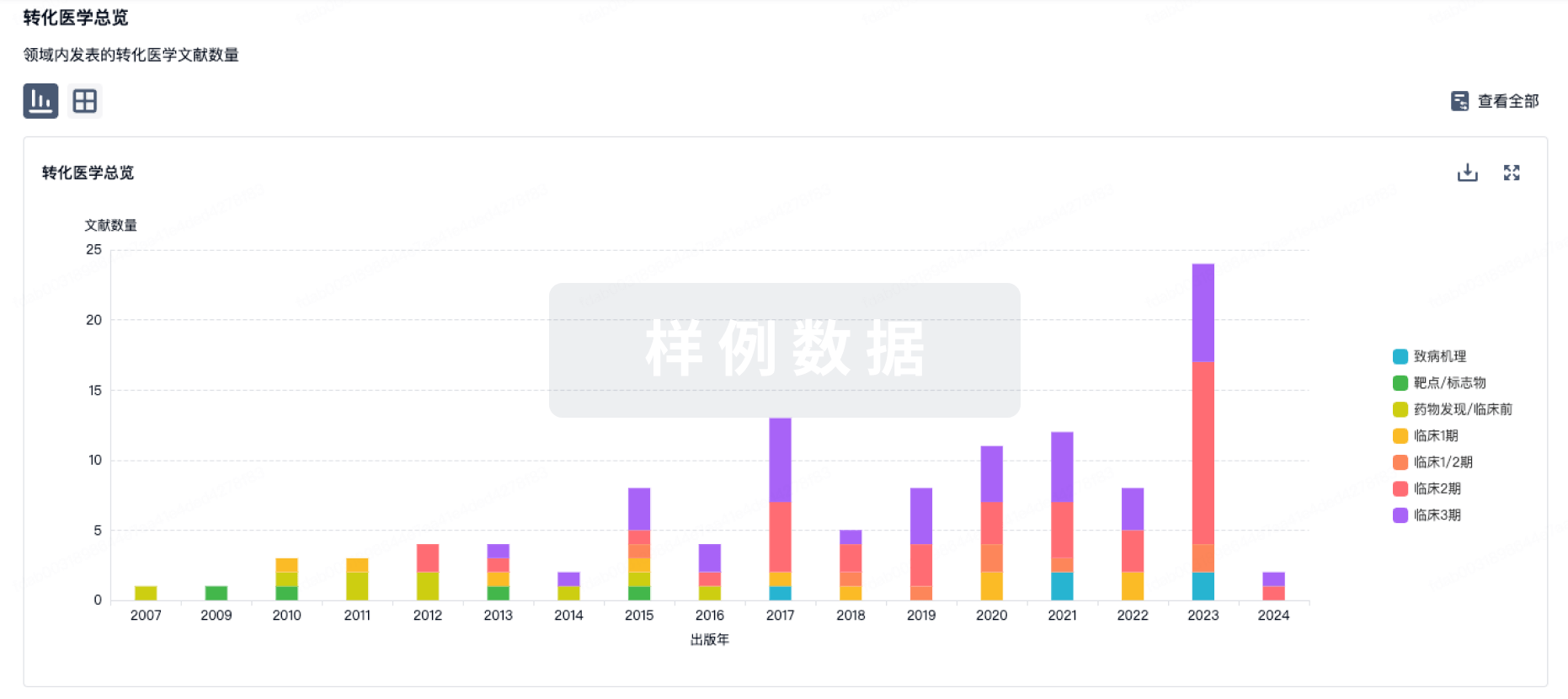
100 项与 NSAID(University of Turin) 相关的转化医学
登录后查看更多信息
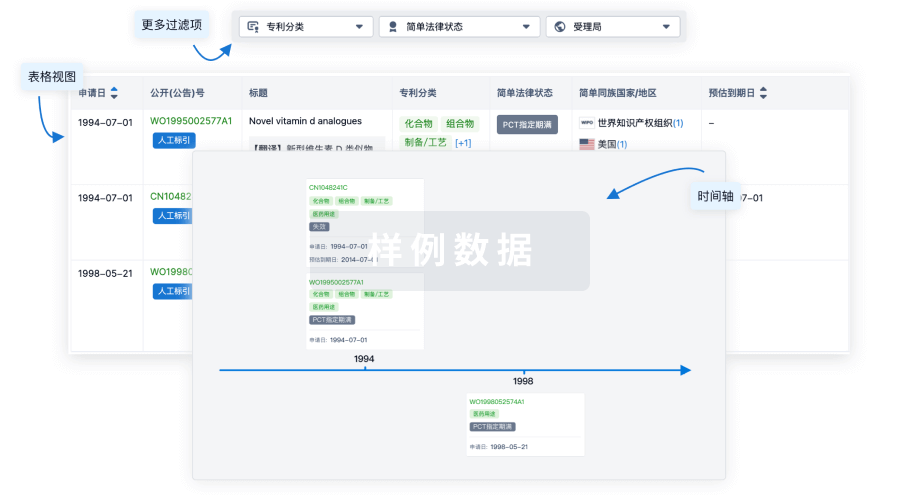
100 项与 NSAID(University of Turin) 相关的专利(医药)
登录后查看更多信息
12
项与 NSAID(University of Turin) 相关的文献(医药)2025-01-01·Medicine & Science in Sports & Exercise
Nonsteroidal Anti-Inflammatory Drugs Do Not Affect the Bone Metabolic Response to Exercise
Article
作者: GWIN, JESS A. ; GEDDIS, ALYSSA V. ; HUGHES, JULIE M. ; SCZUROSKI, CARA E. ; ROBERTS, BRANDON M. ; STAAB, JEFFERY S.
2024-11-01·International Journal of Pharmaceutics
Formulation, optimization and evaluation of ibuprofen loaded menthosomes for transdermal delivery
Article
作者: Gopinathan, Adarsh ; Rathnanand, Mahalaxmi ; John, Jeena ; Halagali, Praveen ; Shetty, Manisha M ; Nayak, Devika ; Krishna Tippavajhala, Vamshi
2024-09-01·The Journal of Arthroplasty
The Use of Tranexamic Acid for Primary Prophylaxis of Heterotopic Ossification Following Total Hip Arthroplasty
Article
作者: King, Paul J ; Johnson, Andrea H. ; Turcotte, Justin J ; Brennan, Jane C ; Brennan, Jane C. ; Turcotte, Justin J. ; Johnson, Andrea H ; King, Paul J. ; Rana, Parimal
100 项与 NSAID(University of Turin) 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 炎症 | 临床前 | 意大利 | 2001-10-11 |
登录后查看更多信息
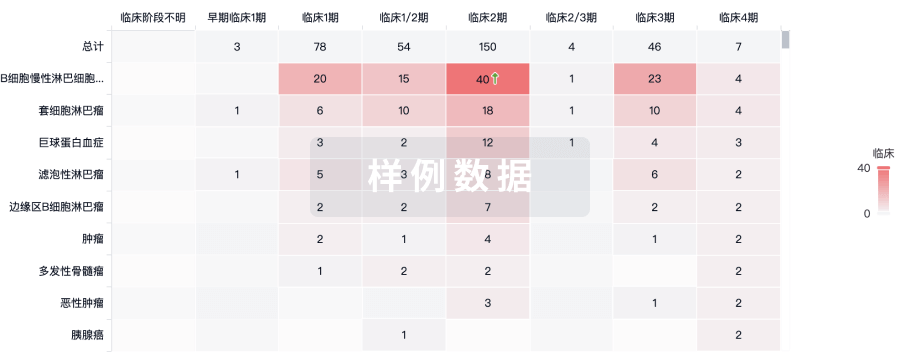
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或

核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

来和芽仔聊天吧
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
