预约演示
更新于:2024-12-26
GliomaGlioblas peptide vaccine(Glioma Actively Personalized Vaccine Consortium)
更新于:2024-12-26
概要
基本信息
非在研机构- |
最高研发阶段临床1期 |
首次获批日期- |
最高研发阶段(中国)- |
特殊审评- |
登录后查看时间轴
关联
1
项与 GliomaGlioblas peptide vaccine(Glioma Actively Personalized Vaccine Consortium) 相关的临床试验NCT02149225
A Phase I Trial of Actively Personalized Peptide Vaccinations Plus Immunomodulators in Patients With Newly Diagnosed Glioblastoma Concurrent to First Line Temozolomide Maintenance Therapy
The primary objective of this study is to assess the safety and tolerability, feasibility and biological activity (immunogenicity) of the actively personalized vaccination (APVAC) concept in newly diagnosed glioblastoma (GB) patients.
开始日期2014-10-01 |
申办/合作机构 |
100 项与 GliomaGlioblas peptide vaccine(Glioma Actively Personalized Vaccine Consortium) 相关的临床结果
登录后查看更多信息
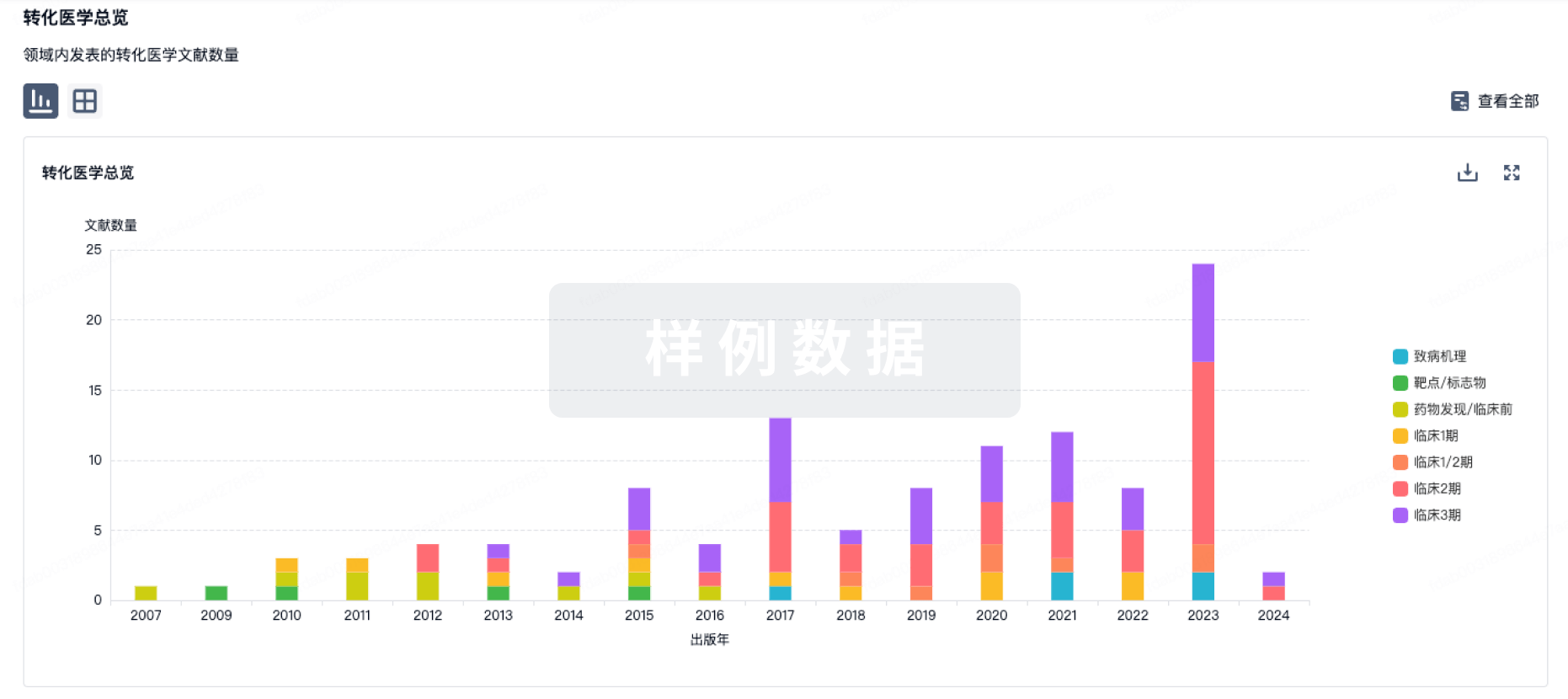
100 项与 GliomaGlioblas peptide vaccine(Glioma Actively Personalized Vaccine Consortium) 相关的转化医学
登录后查看更多信息
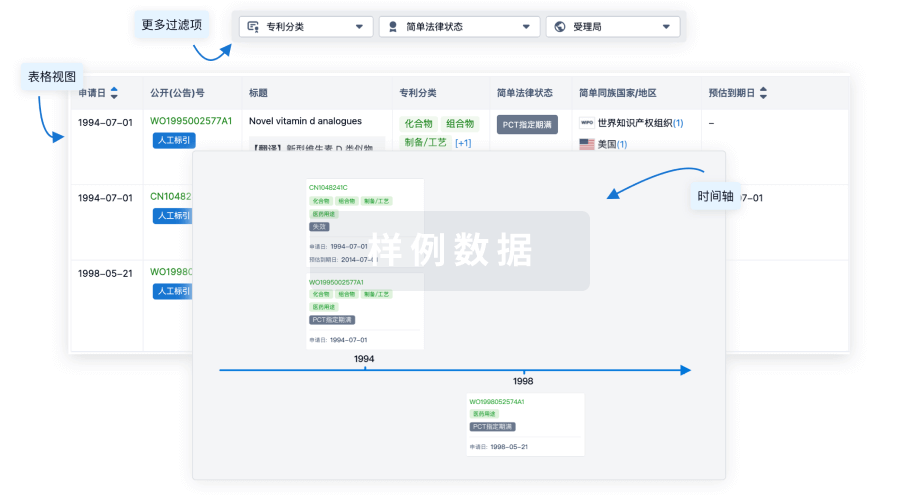
100 项与 GliomaGlioblas peptide vaccine(Glioma Actively Personalized Vaccine Consortium) 相关的专利(医药)
登录后查看更多信息
3
项与 GliomaGlioblas peptide vaccine(Glioma Actively Personalized Vaccine Consortium) 相关的文献(医药)2019-01-10·Nature
Actively personalized vaccination trial for newly diagnosed glioblastoma
Article
作者: Green, Edward ; Derhovanessian, Evelyna ; von Deimling, Andreas ; Ulges, Alexander ; Okada, Hideho ; Gouttefangeas, Cécile ; Kroep, Judith R ; Ponsati, Berta ; Singh-Jasuja, Harpreet ; Shraibman, Bracha ; Reinhardt, Carsten ; Huber, Christoph ; Kiesel, Katharina ; Migliorini, Denis ; Bukur, Valesca ; Sahuquillo, Juan ; Hoffgaard, Franziska ; Wick, Wolfgang ; Lassen, Ulrik ; Stevanović, Stefan ; Castle, John C ; Kemmer-Brück, Alexandra ; Dorner, Sonja ; Dietrich, Pierre-Yves ; Ottensmeier, Christian H ; Sahin, Ugur ; van der Burg, Sjoerd H ; Capper, David ; Tabatabai, Ghazaleh ; Britten, Cedrik M ; Kreiter, Sebastian ; Tadmor, Arbel D ; Dutoit, Valerie ; Admon, Arie ; Poulsen, Hans S ; Rusch, Elisa ; Rammensee, Hans-Georg ; Heesch, Sandra ; Fritsche, Jens ; Platten, Michael ; Piró, Jordi ; Bunse, Lukas ; Song, Colette ; Martínez-Ricarte, Francisco ; Hilf, Norbert ; Skardelly, Marco ; Frenzel, Katrin ; Stieglbauer, Monika ; Idorn, Manja ; Ludwig, Jörg ; Thor Straten, Per ; Welters, Marij J P ; McCann, Katy ; Maurer, Dominik ; Mendrzyk, Regina ; Meyer, Miriam ; Kuttruff-Coqui, Sabrina ; Rössler, Bernhard ; Rodon, Jordi ; Wagner, Claudia ; Weinschenk, Toni ; Schoor, Oliver ; Löwer, Martin ; Pawlowski, Nina
Patients with glioblastoma currently do not sufficiently benefit from recent breakthroughs in cancer treatment that use checkpoint inhibitors1,2. For treatments using checkpoint inhibitors to be successful, a high mutational load and responses to neoepitopes are thought to be essential3. There is limited intratumoural infiltration of immune cells4 in glioblastoma and these tumours contain only 30-50 non-synonymous mutations5. Exploitation of the full repertoire of tumour antigens-that is, both unmutated antigens and neoepitopes-may offer more effective immunotherapies, especially for tumours with a low mutational load. Here, in the phase I trial GAPVAC-101 of the Glioma Actively Personalized Vaccine Consortium (GAPVAC), we integrated highly individualized vaccinations with both types of tumour antigens into standard care to optimally exploit the limited target space for patients with newly diagnosed glioblastoma. Fifteen patients with glioblastomas positive for human leukocyte antigen (HLA)-A*02:01 or HLA-A*24:02 were treated with a vaccine (APVAC1) derived from a premanufactured library of unmutated antigens followed by treatment with APVAC2, which preferentially targeted neoepitopes. Personalization was based on mutations and analyses of the transcriptomes and immunopeptidomes of the individual tumours. The GAPVAC approach was feasible and vaccines that had poly-ICLC (polyriboinosinic-polyribocytidylic acid-poly-L-lysine carboxymethylcellulose) and granulocyte-macrophage colony-stimulating factor as adjuvants displayed favourable safety and strong immunogenicity. Unmutated APVAC1 antigens elicited sustained responses of central memory CD8+ T cells. APVAC2 induced predominantly CD4+ T cell responses of T helper 1 type against predicted neoepitopes.
OncoTargets and therapy4区 · 医学
<p>A Hybrid Glioma Tumor Cell Lysate Immunotherapy Vaccine Demonstrates Good Clinical Efficacy in the Rat Model</p>
4区 · 医学
ArticleOA
作者: Chen, Li-Gang ; Peng, Li-Lei ; Zeng, Shan ; He, Hai-Ping ; Zeng, Xu ; Li, Xin-Long
BACKGROUND:
Conventional immunotherapy for glioma is not only expensive but also demonstrates less-than-desired clinical efficacy. In this study, we evaluated the immunotherapeutic efficacy of a tumor cell lysate-based hybrid glioma vaccine developed using a molecular-based approach.
METHODS:
First, the ability of the autologous (9L-cell lysate) and allogeneic (C6-cell lysate) vaccines against glioma, individually and in combination, to activate Fischer344 rat dendritic cells (DCs) was determined. Next, the activated DCs were co-cultured with T lymphocytes and screened for the optimal DC-to-T-cell ratio. The in vitro efficacy of the DC/T-cell vaccine formulations subjected to different immunogen treatments and co-cultured with glioma cells was evaluated based on glioma cell viability and monocyte chemoattractant protein (MCP)-2 and interferon (IFN)-γ secretion. Subsequently, the efficacy of the 9L + C6 hybrid vaccine was evaluated in 32 glioma rat models, randomly allocated to the following five treatment groups: blank control, tumor, vaccine treatment, thymosin treatment, and vaccine + thymosin treatment (combined treatment). Changes in survival duration, intracranial tumor volume, peripheral blood immune-cell (CD4+ T, CD8+ T, and natural killer [NK] cell) count, and serum cytokine (interleukin [IL]-2, IL-10) levels were assessed in these groups.
RESULTS:
The hybrid vaccine demonstrated the highest glioma cell apoptosis and the lowest cell viability and promoted MCP-2 and IFN-γ secretion in vitro. The vaccine treatment and combined treatment groups demonstrated longer survival duration, lower intracranial tumor volume, and higher immune cell glioma tissue infiltration and IL-2 secretion than the untreated tumor group, indicating the vaccine's good in vivo efficacy. Thymosin treatment had minimal effect in enhancing anti-glioma immunity.
CONCLUSION:
We demonstrated the feasibility of combining autologous and allogeneic tumor cell lysates to stimulate specific host cell immune response against glioma cells. The good clinical efficacy of our developed glioma hybrid vaccine in rat models suggests its potential clinical application.
International journal of general medicine4区 · 医学
Efficacy and Safety of Actively Personalized Neoantigen Vaccination in the Management of Newly Diagnosed Glioblastoma: A Systematic Review
4区 · 医学
ReviewOA
作者: Li, Zihuang ; Yang, Hongli ; Khan, Muhammad ; Liao, Guixiang ; Yan, Maosheng ; Li, Xianming
PURPOSE:
Glioblastoma (GBM) shows frequent relapse and is highly resistant to treatment; therefore, it is considered fatal. Various vaccination protocols that have been tested in patients with GBM, which is the most common and aggressive primary brain tumor, have indicated safety and efficacy, to some extent, when used alone or in combination with standard of care. Recently, neoantigen-based personalized vaccines have shown tremendous immunogenicity and safety in GBM. We aimed to systematically review the medical literature for clinical trials to evaluate the efficacy and safety of neoantigen-based personalized vaccines for newly diagnosed GBM.
METHODS:
We conducted a literature search for clinical trials on PubMed, Cochrane Library, China National Knowledge Infrastructure, and ClinicalTrials.gov until March 20, 2021. The primary outcomes of interest were immunogenicity and safety of the therapy. Efficacy outcomes, such as progression-free survival and overall survival, were secondary outcomes of interest.
RESULTS:
Two clinical trials involving 24 patients were included in this review. High immunogenicity was observed in both studies. The GAPVAC-101 trial reported 50% APVAC1-induced and 84.7% APVAC2-induced immunogenicity with CD8+ and CD4+ T cell responses in 92% (12/13) and 80% (8/10) immune responders, respectively. Two out of five patients showed CD4+ and CD8+ T cell responses in the study by Keskin et al. Dexamethasone use had limited immunogenicity in a trial by Keskin et al (6/8). No serious treatment-related adverse events were reported.
CONCLUSION:
Actively personalized vaccines aimed at unmutated peptides and neoantigens for patients with GBM are safe and highly immunogenic, particularly when administered in combination. Larger studies are warranted to investigate the role.
1
项与 GliomaGlioblas peptide vaccine(Glioma Actively Personalized Vaccine Consortium) 相关的新闻(医药)2022-06-19
一直以来,癌症疫苗经历了屡败屡战的漫长经历。其中原因可能在于早期的治疗性疫苗接种策略集中于在肿瘤中异常表达或过表达的自身抗原,称为肿瘤相关抗原(TAAs )。然而这些抗原在产生临床有效的抗肿瘤免疫反应方面很大程度上是不成功的,这可能是由于TAA特异性T细胞受到中枢或外周耐受性的影响。此外,这种TAAs也可以在一定程度上在非恶性组织中表达,这增加了疫苗诱导的自身免疫毒性的风险。既然这条路暂时可能走不通,从另外一个方向转变策略或许能让肿瘤疫苗走向成功之路。肿瘤细胞中发生的突变可以产生新的自身抗原表位,称为新表位或新抗原。而新一代测序技术,MHC I类(MHC I)结合表位预测算法等技术的出现提供了及时和经济有效地识别个体患者中这些肿瘤特异性突变的机会,针对个体患者肿瘤量身定制的癌症疫苗得以产生。事实上在个性化时代到来下,诸如CAR-T,基因治疗等治疗方式为个性化治疗手段早已付诸实践,而不少肿瘤疫苗也采取了相似的思路,为患者量身定做出个性化的癌症疫苗,他们通过与各种形式逐步推进其独有的临床进程,并逐渐开枝散叶,通过各种技术和联用手段为这种形式疫苗的未来发展方向奠定了基础。个性化DC疫苗从个性化癌症疫苗的发展历史来看,最开始应用于个性化癌症疫苗的可能是宾夕法尼亚大学的成熟树突细胞疫苗(NCT00683670)。当时这一研究发表文章的署名上甚至能看到免疫细胞疗法的鼻祖Steven A. Rosenberg的大名。黑色素瘤由于暴露于紫外线等诱变剂条件下,往往会产生大量突变,这些突变会导致肿瘤细胞产生与人体自身细胞非常不同的蛋白质。而疫苗中使用的这些蛋白质可能会诱导强烈的免疫反应,这可能有助于参与者的身体对抗任何可能导致黑色素瘤在未来复发的肿瘤细胞。为了识别与人类肿瘤排斥反应相关的黑色素瘤抗原,宾大的团队首先获得了在转移性黑色素瘤结节上生长的肿瘤浸润淋巴细胞(tTILs)并将其过继性转移到自体黑色素瘤患者。那些与体内肿瘤衰退相关的TILs被用来筛选来自肿瘤的cDNA文库,以鉴定它们识别的抗原。他们最终获得了多达10种用编码患者特异性肿瘤新表位的HLA-A*02:01特异性肽和来自黑色素瘤相关抗原gp100的2种肽组成的自体树突细胞疫苗,并将其注输给事先服用环磷酰胺清除调节性T细胞的患者。这项研究首次揭示了新抗原治疗性疫苗接种可以增加T细胞反应的多样性和广度。此后,除了树突细胞疫苗,更多种类的疫苗技术形式逐步迈入个性化癌症疫苗的大框架下。值得一提的是将TAAs疫苗与个性化癌症疫苗联合作用也是可行的方法之一。此外,个性化癌症疫苗也不再局限于黑色素瘤一个癌种,获得了更广阔的的应用空间,例如,另外一项关于胶质母细胞瘤患者的个性化DC疫苗临床(NCT03548571)就正在展开。而随后,个性化癌症疫苗使得8位晚期黑色素瘤的平均生存时间长达四年的优异疗效更是为个性化癌症疫苗的前景铺平了道路。与TAAs联用高肿瘤突变负荷(TMB)的患者可能对于受到个性化癌症疫苗治疗效果更为显著,尽管这些新抗原疫苗有许多优点,但将TAAs疫苗联用可能是低TMB患者更适合的选择。例如,胶质母细胞瘤是一种典型的突变负荷低的癌症类型,常被认为是一种免疫“冷”肿瘤。在一项使用TAAs与个性化癌症疫苗联用的研究中,通过APVAC1及APVAC2两条途径,分别通过GB相关抗原非突变肽和突变肽肽库中筛选查找抗原肽,这项研究初步的数据证明了其安全性和可行性,有待后续研究披露跟进一步的疗效数据。与免疫检查点抑制剂联用肿瘤微环境中的效应T细胞获得的免疫检查点分子使它们逐渐耗尽,不能杀死肿瘤细胞。这导致了近年来免疫检查点抑制剂ICB的发展,它现在被用于治疗多种类型的癌症。基于ICB的疗法已经在多种癌症中获得了成功,但肿瘤耐药性,冷肿瘤等肿瘤微环境等因素使其受到了一定局限。因此,将ICB与增加浸润性肿瘤特异性T细胞数量的疗法(如疫苗接种)相结合的基本原理经常受到强调。而临床试验已经测试了这种组合方法在癌症患者中的功效:例如:GVAX疫苗是同种异体的巨噬细胞-粒细胞集落刺激因子(GM-CSF)转基因疫苗。将切除的肿瘤细胞分离培养后,导入GM-CSF基因进行修饰,其表达产物GM-CSF可刺激免疫系统对疫苗的反应。通过将这些细胞进行辐射处理,制成疫苗。在Ib期研究中,在胰腺癌患者中测试了ipilimumab与GVAX疫苗的组合。与单独使用ipilimumab相比,疫苗与抗CTLA-4疗法的组合改善了OS。在同一作者的另一项研究中,他们表明抗体介导的CTLA-4阻断增强了一些先前接种了GVAX疫苗的肿瘤免疫。此外,mRNA疫苗中展开的多项临床也采用了与免疫检查点抑制剂联用的方式。mRNA个性化疫苗技术的验证可行性作为mRNA疫苗的先行者,BioNTech和Moderna公司都在个性化mRNA疫苗的赛道中eran(前名RO7198457)是基于BNT的iNeST技术平台开发的个体化mRNA疫苗。iNeST技术平台使得该个性化癌症疫苗能够搭载至多20个能让免疫系统最可能识别的突变抗原。BioNTech此前在美国临床肿瘤学会(ASCO)年会上报告了其个体化mRNA癌症疫苗Autogene Cevumeran与罗氏PD-L1检查点抑制剂atezolizumab和化疗在接受手术切除导管的腺癌患者中联合应用的第一阶段初步数据。结果显示,来自16名手术后接受疫苗接种的患者数据表明,这一疗法耐受性良好,只有一名患者出现了疫苗相关的3级发热和高血压。该疗法在一半的患者中诱导了新抗原特异性T细胞反应。而与以前检测不到的水平相比,针对新抗原的T细胞水平上升到了总水平的2.9%。此外,在18个月的早期中位随访中,与没有疫苗诱导的免疫反应的患者相比,有重新免疫反应的患者显示出显著更长的无复发生存期(RFS)。相比BNT的20种新抗原,Moderna的数量一下子加到了34种。Moderna关于个体化肿瘤疫苗mRNA-4157的I期临床研究(NCT03313778 & NCT03480152)表明:在切除黑色素瘤、结肠癌和肺癌等原发肿瘤后,接受mRNA-4157作为单药辅助治疗的13名患者中,11名患者在研究中保持无病状态长达75周。在联合K药治疗不可切除实体瘤的10名HPV阴性的头颈鳞状细胞癌患者和17名微卫星稳定型(MSS)结直肠癌患者中:有一半的HPV阴性的头颈鳞状细胞癌患者肿瘤缩小,且其中2名患者肿瘤完全消失,疾病控制率高达90%,在安全性方面来看,没有发现与疫苗相关的严重不良事件;但在MSS结直肠癌中并没有观察到肿瘤缩小,可能由于MSS结直肠癌属于“冷”肿瘤,肿瘤免疫微环境中缺少T细胞浸润。与抗血管生成治疗药物(AATs)联用在癌症的疾病发展过程中,肿瘤会增加促血管生成分子的表达,如血管内皮生长因子(VEGF),它参与肿瘤血管生成。另一方面,异常的肿瘤脉管系统通过为T细胞浸润提供物理屏障而主动抑制抗肿瘤反应,并由于对肿瘤的不良递送而限制治疗药物的功效。肿瘤血管生成通过其免疫抑制作用也有助于免疫逃逸。因此将抗血管生成治疗药物与个性化肿瘤疫苗联用也是未来的可能方向之一。例如:舒尼替尼与基于DC的个性化疫苗AGS-003联合使用,该疫苗由用总自体肿瘤RNA和CD40L RNA转染的单核细胞衍生的树突状细胞组成。舒尼替尼第二周期开始时开始接种疫苗。联合治疗诱导了免疫反应并延长了生存期。这些令人鼓舞的结果导致了三期临床试验,但AGS-003未能改善OS。总的来说,尽管在了解AATs对于肿瘤疫苗的影响方面取得了进展,但癌症疫苗的组合方法未能证明临床疗效。仍然需要更进一步的研究其中机理机制和临床设计。小编总结随着技术的越发进步,可能可以看到越来越多的基于个性化癌症疫苗的新抗原,将个性化癌症疫苗与更丰富的治疗方式联合使用也是未来的证明效果的途径之一,这也对个性化疫苗的临床设计和评估标准提出了挑战。此外,从患者样本数量来看,个性化癌症疫苗似乎并没有得到大规模的临床应用,这可能让人担忧其成本负担过高,生产产能有限等问题,因此或许Zolgensma的单价地位将受到挑战,这有可能无法惠及更多的患者,因此个性化癌症疫苗的商业化可能仍然要受限于技术与工艺限制。参考来源:1.Blass, Eryn, and Patrick A Ott. “Advances in the development of personalized neoantigen-based therapeutic cancer vaccines.” Nature reviews. Clinical oncology vol. 18,4 (2021): 215-229. doi:10.1038/s41571-020-00460-22.Shemesh CS, Hsu JC, Hosseini I, et al. Personalized Cancer Vaccines: Clinical Landscape, Challenges, and Opportunities. Mol Ther. 2021;29(2):555-570. doi:10.1016/j.ymthe.2020.09.0383.Mougel A, Terme M, Tanchot C. Therapeutic Cancer Vaccine and Combinations With Antiangiogenic Therapies and Immune Checkpoint Blockade. Front Immunol. 2019;10:467. Published 2019 Mar 14. doi:10.3389/fimmu.2019.004674.Carreno, Beatriz M et al. “Cancer immunotherapy. A dendritic cell vaccine increases the breadth and diversity of melanoma neoantigen-specific T cells.” Science (New York, N.Y.) vol. 348,6236 (2015): 803-8. doi:10.1126/science.aaa38285.Le DT, Lutz E, Uram JN, Sugar EA, Onners B, Solt S, et al.. Evaluation of ipilimumab in combination with allogeneic pancreatic tumor cells transfected with a GM-CSF gene in previously treated pancreatic cancer. J Immunother. (2013) 36:382–9. 10.1097/CJI.0b013e31829fb7a2
疫苗信使RNA免疫疗法抗体基因疗法
100 项与 GliomaGlioblas peptide vaccine(Glioma Actively Personalized Vaccine Consortium) 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 胶质母细胞瘤 | 临床2期 | 瑞士 | 2014-09-30 |
登录后查看更多信息
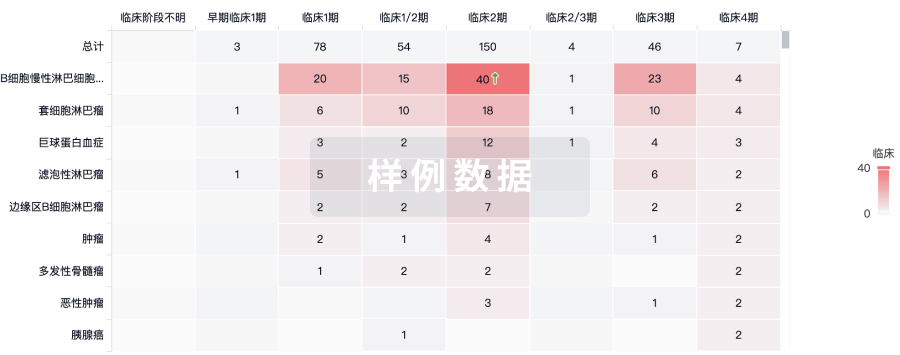
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或

核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

来和芽仔聊天吧
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用

