预约演示
更新于:2025-05-24
L1CAM-directed CAR T(University of Bern)
更新于:2025-05-24
概要
基本信息
非在研机构- |
权益机构- |
最高研发阶段临床前 |
首次获批日期- |
最高研发阶段(中国)- |
特殊审评- |
关联
100 项与 L1CAM-directed CAR T(University of Bern) 相关的临床结果
登录后查看更多信息
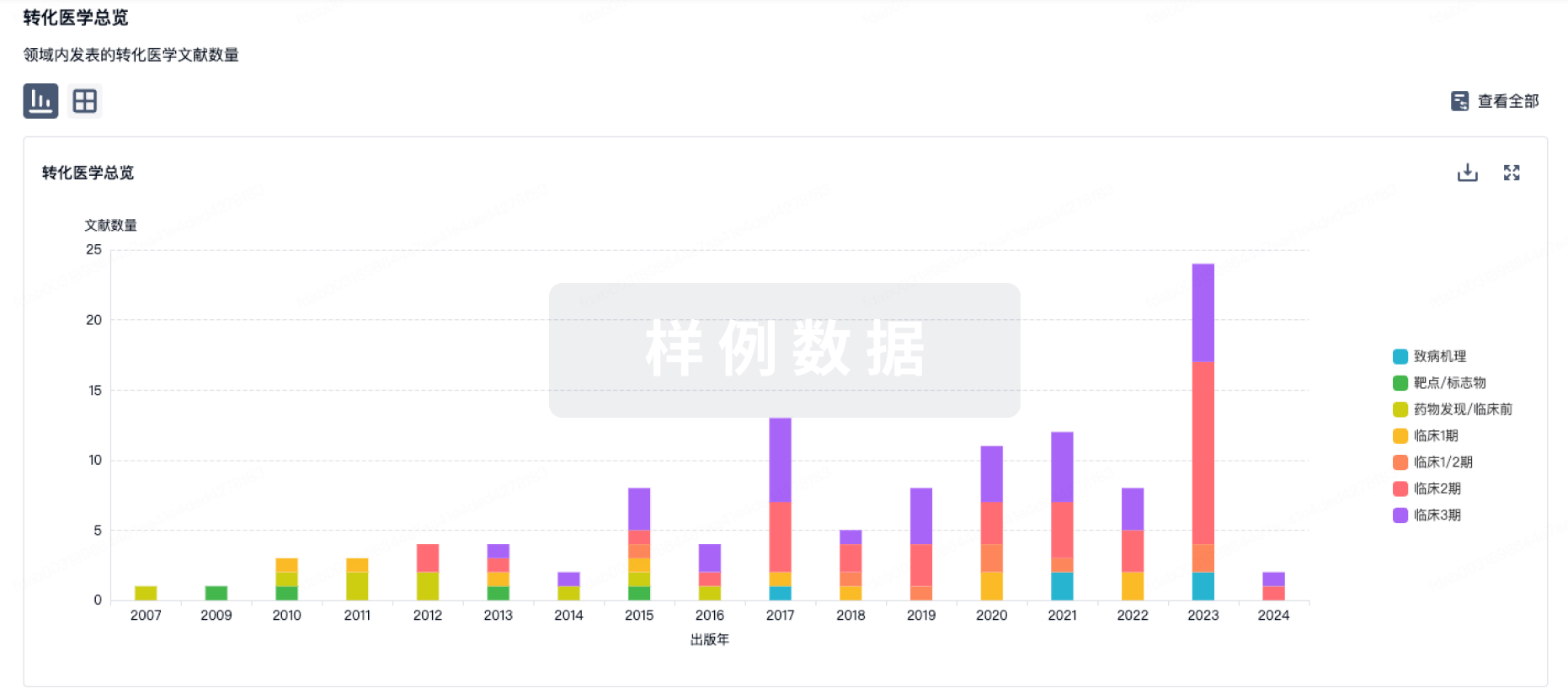
100 项与 L1CAM-directed CAR T(University of Bern) 相关的转化医学
登录后查看更多信息
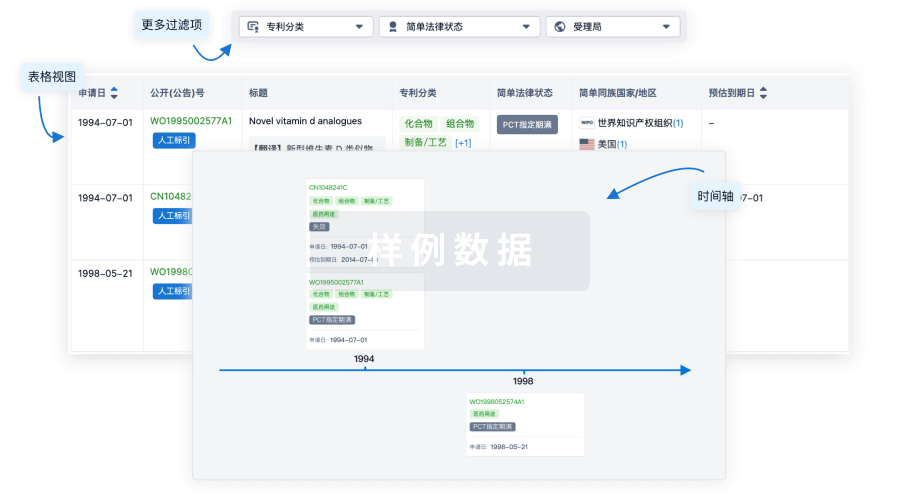
100 项与 L1CAM-directed CAR T(University of Bern) 相关的专利(医药)
登录后查看更多信息
2
项与 L1CAM-directed CAR T(University of Bern) 相关的文献(医药)2025-02-01·PHARMACOLOGICAL RESEARCH
Targeting MYCN upregulates L1CAM tumor antigen in MYCN-dysregulated neuroblastoma to increase CAR T cell efficacy
Article
作者: Westermann, Frank ; Astrahantseff, Kathy ; Helmsauer, Konstantin ; Caramel, Carlotta ; Büchel, Gabriele ; Klaus, Anika ; Fuchs, Steffen ; Andersch, Lena ; Vitali, Alice ; Lodrini, Marco ; Schwiebert, Silke ; Blankenstein, Thomas ; Künkele, Annette ; Henssen, Anton G ; Höpken, Uta E ; Wicha, Sebastian G ; Anders, Kathleen ; Schulte, Johannes H ; Straka, Teresa ; Eggert, Angelika ; Eilers, Martin ; Hertwig, Falk ; Grunewald, Laura
Current treatment protocols have limited success against MYCN-amplified neuroblastoma. Adoptive T cell therapy presents an innovative strategy to improve cure rates. However, L1CAM-targeting CAR T cells achieved only limited response against refractory/relapsed neuroblastoma so far. We investigated how oncogenic MYCN levels influence tumor cell response to CAR T cells, as one possible factor limiting clinical success. A MYCN-inducible neuroblastoma cell model was created. L1CAM-CAR T cell effector function was assessed (activation markers, cytokine release, tumor cytotoxicity) after coculture with the model or MYCN-amplified neuroblastoma cell lines. RNA sequencing datasets characterizing the model were compared to publicly available RNA/proteomic datasets. MYCN-directed L1CAM regulation was explored using public ChIP-sequencing datasets. Synergism between CAR T cells and the indirect MYCN inhibitor, MLN8237, was assessed in vitro using the Bliss model and in vivo in an immunocompromised mouse model. Inducing high MYCN levels in the neuroblastoma cell model reduced L1CAM expression and, consequently, L1CAM-CAR T cell effector function in vitro. Primary neuroblastomas possessing high MYCN levels expressed lower levels of both the L1CAM transcript and L1CAM tumor antigen. MLN8237 treatment restored L1CAM tumor expression and L1CAM-CAR T cell effector function. Combining MLN8237 and L1CAM-CAR T cell treatment synergistically enhanced MYCN-overexpressing tumor cytotoxicity in vitro and in vivo concomitant with severe in vivo toxicity. We identify target antigen downregulation as source of resistance against L1CAM-CAR T cells in MYCN-driven neuroblastoma cells. These data suggest that L1CAM-CAR T cell therapy combined with pharmacological MYCN inhibition may benefit patients with MYCN-amplified neuroblastoma.
2020-07-01·MOLECULAR CARCINOGENESIS
Central memory phenotype drives success of checkpoint inhibition in combination with CAR T cells
Article
作者: Schulte, Johannes H. ; Klaus, Anika ; Schwiebert, Silke ; Ochsenreither, Sebastian ; Toews, Karin ; Astrahantseff, Kathy ; Deubzer, Hedwig E. ; Zirngibl, Felix ; Winkler, Annika ; Wagner, Dimitrios L. ; Künkele, Annette ; Henssen, Anton G. ; Ali, Solin ; Grunewald, Laura ; Eggert, Angelika
Abstract:
The immunosuppressive microenvironment in solid tumors is thought to form a barrier to the entry and efficacy of cell‐based therapies such as chimeric antigen receptor (CAR) T cells. Combining CAR T cell therapy with checkpoint inhibitors has been demonstrated to oppose immune escape mechanisms in solid tumors and augment antitumor efficacy. We evaluated PD‐1/PD‐L1 signaling capacity and the impact of an inhibitor of this checkpoint axis in an in vitro system for cancer cell challenge, the coculture of L1CAM‐specific CAR T cells with neuroblastoma cell lines. Fluorescence‐activated cell sorting‐based analyses and luciferase reporter assays were used to assess PD‐1/PD‐L1 expression on CAR T and tumor cells as well as CAR T cell ability to kill neuroblastoma cells. Coculturing neuroblastoma cell lines with L1CAM‐CAR T cells upregulated PD‐L1 expression on neuroblastoma cells, confirming adaptive immune resistance. Exposure to neuroblastoma cells also upregulated the expression of the PD‐1/PD‐L1 axis in CAR T cells. The checkpoint inhibitor, nivolumab, enhanced L1CAM‐CAR T cell‐directed killing. However, nivolumab‐enhanced L1CAM‐CAR T cell killing did not strictly correlate with PD‐L1 expression on neuroblastoma cells. In fact, checkpoint inhibitor success relied on strong PD‐1/PD‐L1 axis expression in the CAR T cells, which in turn depended on costimulatory domains within the CAR construct, and more importantly, on the subset of T cells selected for CAR T cell generation. Thus, T cell subset selection for CAR T cell generation and CAR T cell prescreening for PD‐1/PD‐L1 expression could help determine when combination therapy with checkpoint inhibitors could improve treatment efficacy.
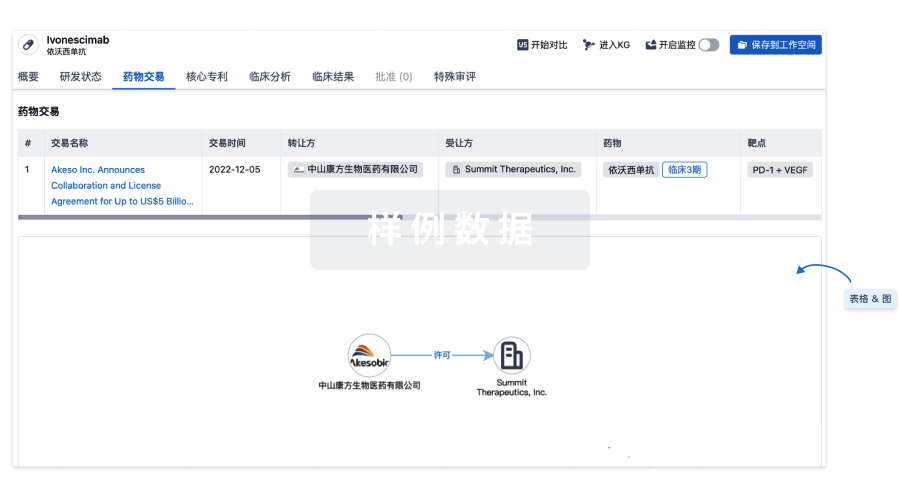
100 项与 L1CAM-directed CAR T(University of Bern) 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 横纹肌肉瘤 | 临床前 | 瑞士 | 2025-04-29 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
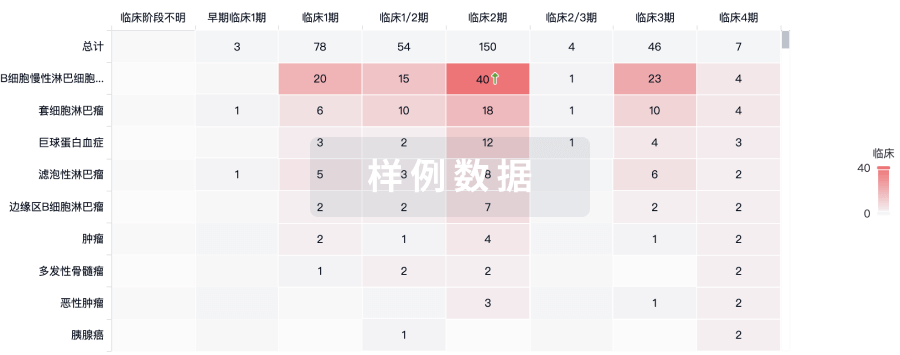
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
