预约演示
更新于:2025-05-16
Herpes zoster vaccine (SK Chemicals)
更新于:2025-05-16
概要
基本信息
非在研机构- |
权益机构- |
最高研发阶段批准上市 |
首次获批日期 韩国 (2017-09-29), |
最高研发阶段(中国)- |
特殊审评- |
登录后查看时间轴
关联
5
项与 Herpes zoster vaccine (SK Chemicals) 相关的临床试验NCT03114943
A Multi-national, Multi-center, Randomized, Double Blinded, Parallel-group Study to Assess the Immunogenicity and Safety of NBP608 Compared to Varivax in Healthy Children 12 Months to 12 Years of Age
This study assesses non-inferiority by comparing seroconversion rate of NBP608 to Varivax which are indicated for active immunization for prevention of varicella. Total of 488 subjects (244 subjects per treatment arm) of 12 months to 12 years of age are enrolled, and each subject is administered with single dose of vaccine which is randomly assigned.
开始日期2016-07-14 |
申办/合作机构 |
NCT03114982
Randomized, Double-blinded, Parallel-group, Exploratory Study to Assess The Immunogenicity and Safety of NBP608 and Varivax in Healthy Children
This study evaluates the immunogenicity and safety of three different potencies of NBP608 and Varivax which are indicated for active immunization for the prevention of varicella. Total of 152 subjects (38 subjects per each treatment arm) of 12 months to 12 years of age are enrolled, and each subject is administered with single dose of vaccine which is randomly assigned.
开始日期2016-05-01 |
申办/合作机构 |
NCT03120364
A Randomized, Double Blinded, Multi-center Phase III Confirmatory Study to Assess the Immunogenicity and Safety of NBP608 Compared to Zostavax in Healthy Adult Aged 50 and Over
This study assesses non-inferiority by comparing GMR(Geometric Mean Ratio) of NBP608 to Zostavax which are evaluated by gpELISA (Glycoprotein Enzyme Linked Immunosorbent Assay). Total of 824 healthy subjects (412 subjects per treatment arm) aged 50 and over are enrolled, and each subject is administered with single dose of vaccine which is randomly assigned.
开始日期2015-09-09 |
申办/合作机构 |
100 项与 Herpes zoster vaccine (SK Chemicals) 相关的临床结果
登录后查看更多信息
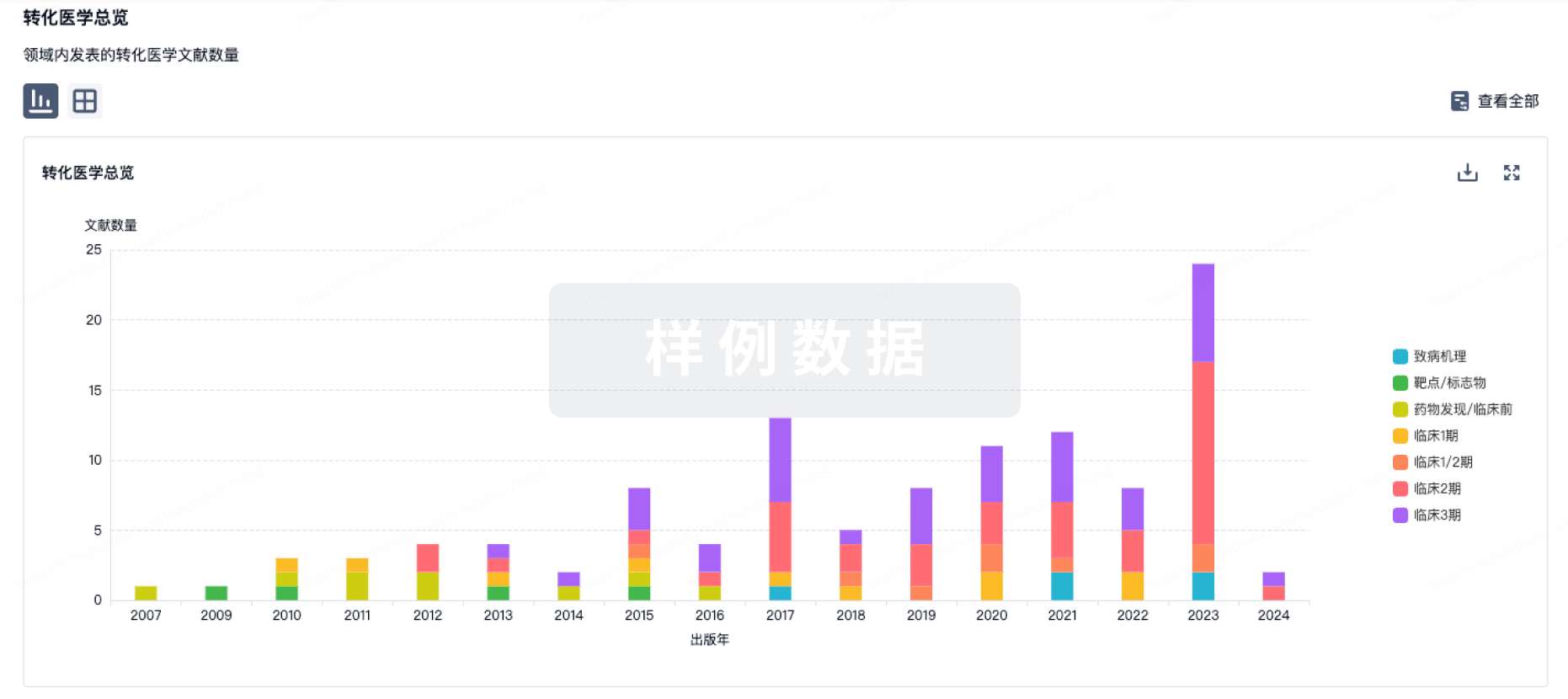
100 项与 Herpes zoster vaccine (SK Chemicals) 相关的转化医学
登录后查看更多信息
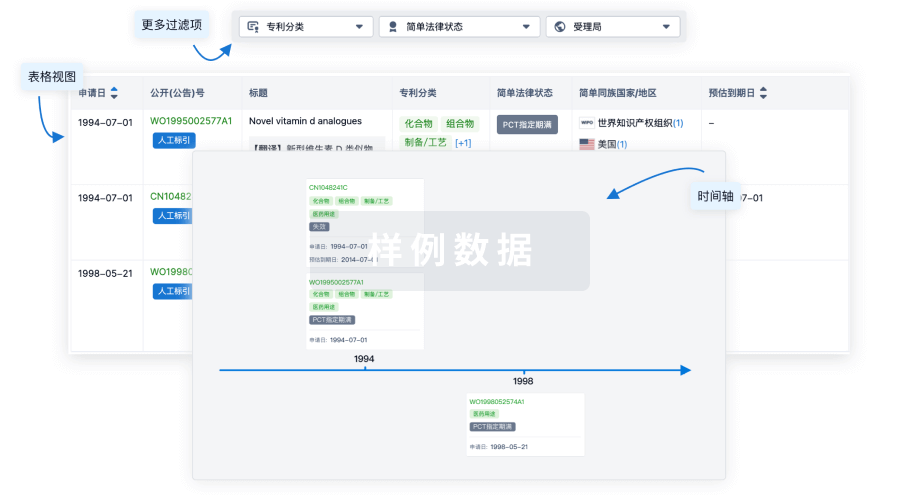
100 项与 Herpes zoster vaccine (SK Chemicals) 相关的专利(医药)
登录后查看更多信息
3
项与 Herpes zoster vaccine (SK Chemicals) 相关的文献(医药)2023-08-24·Vaccines
Immunogenicity and Safety of a Newly Developed Live Attenuated Varicella Vaccine in Healthy Children: A Multi-National, Randomized, Double-Blinded, Active-Controlled, Phase 3 Study.
Article
作者: Lee, Su Jeen ; Ryu, Ji Hwa ; Kobashi, Ilya Angelica Rochin ; Capeding, Maria Rosario ; Choi, Young Youn ; Cho, Hye-Kyung ; Park, Ho Keun ; Kim, Ki Hwan ; Choi, Ui Yoon ; Kim, Hun ; Kim, Chun Soo ; Kim, Dong Ho ; Kim, Jong-Hyun ; Ma, Sang Hyuk
Korean manufacturers have developed a new varicella vaccine, NBP608. This phase 3, randomized, double-blind, multicenter study aimed to compare the immunogenicity and safety of NBP608 in healthy children to those of VarivaxTM (control). Children aged 12 months to 12 years were randomized in a ratio of 1:1 to receive either NBP608 or the control vaccine. Serum samples were obtained before vaccination and within six to eight weeks after vaccination. In total, 499 participants (NBP608, n = 251; control, n = 248) were enrolled. The seroconversion rate (SCR) measured using a FAMA assay was 99.53% in the NBP608 group, and the lower limit of the 95% confidence interval (95% LCL) for the SCR difference (NBP608 minus the control) was 0.52%. This 95% LCL for the difference was higher than the specified non-inferiority margin of -15%. In an assessment using gpELISA, the SCR was 99.53% in the NBP608 group, and the 95% LCL for the SCR difference was 6.5%, which was higher than the specified non-inferiority margin of -15%. There were no significant differences between the NBP608 and control group with respect to the proportions of participants who demonstrated local and systemic solicited AEs. This study indicated that NBP608 had a clinically acceptable safety profile and was not immunologically inferior to VarivaxTM.
2023-02-01·American journal of epidemiology
Sequential Data-Mining for Adverse Events After Recombinant Herpes Zoster Vaccination Using the Tree-Based Scan Statistic
Article
作者: Kulldorff, Martin ; Dashevsky, Inna ; Yih, W Katherine ; Maro, Judith C
Abstract:
Tree-based scan statistics have been successfully used to study the safety of several vaccines without prespecifying health outcomes of concern. In this study, the binomial tree-based scan statistic was applied sequentially to detect adverse events in days 1–28 compared with days 29–56 after recombinant herpes zoster (RZV) vaccination, with 5 looks at the data and formal adjustment for the repeated analyses over time. IBM MarketScan data on commercially insured persons ≥50 years of age receiving RZV during January 1, 2018, to May 5, 2020, were used. With 999,876 doses of RZV included, statistically significant signals were detected only for unspecified adverse effects/complications following immunization, with attributable risks as low as 2 excess cases per 100,000 vaccinations. Ninety percent of cases in the signals occurred in the week after vaccination and, based on previous studies, likely represent nonserious events like fever, fatigue, and headache. Strengths of our study include its untargeted nature, self-controlled design, and formal adjustment for repeated testing. Although the method requires prespecification of the risk window of interest and may miss some true signals detectable using the tree-temporal variant of the method, it allows for early detection of potential safety problems through early initiation of ongoing monitoring.
2019-06-01·Vaccine3区 · 医学
Immunogenicity and safety of a new live attenuated herpes zoster vaccine (NBP608) compared to Zostavax® in healthy adults aged 50 years and older
3区 · 医学
Article
作者: Lee, Jacob ; Choi, Won Suk ; Jung, Dong Sik ; Choi, Hee Jung ; Park, Jun-Sik ; Shin, Eui-Cheol ; Jang, Hee-Chang ; Choi, Jung Hyun ; Cheong, Hee Jin ; Kim, Hun ; Kim, Yeon-Sook
A multi-centre, randomised, double-blinded, active-controlled, parallel-group clinical trial was carried out to assess the immunogenicity and safety of NBP608-a newly developed live-attenuated zoster vaccine in Korea-relative to Zostavax® in healthy adults aged 50 years or older. Immune responses to the vaccine were evaluated by glycoprotein enzyme-linked immunosorbent assay (gpELISA) and enzyme-linked immunosorbent spot (ELISPOT) assays using the interferon (IFN)-γ and interleukin (IL)-2 FluoroSpot kit 6 weeks after vaccination. Safety was monitored for 26 weeks based on subjects' diaries, spontaneous reports from subjects, and history taking by the investigators. A total of 845 subjects participated in the screening, and 823 received the vaccination (413 in the NBP608 group and 411 in the comparator group). The gpELISA-determined geometric mean fold rise from baseline to post NBP608 vaccination was 2.75 [95% confidence interval, CI (2.57, 2.94)]. The gpELISA-determined adjusted geometric mean titers (GMTs) of NBP608 and the comparator were 1346.37 [95% CI (1273.99, 1422.87)] and 1674.94 [95% CI (1585.35, 1769.58)], respectively. The adjusted GMT ratio of NBP608 to the comparator was 0.80 [95% CI (0.75, 0.87)]. There was no statistically significant difference between two groups in terms of the geometric mean spot numbers determined by IFN-γ and IL-2 ELISPOT assays at 6 weeks post vaccination (P = 0.7232, 0.3844). The incidence of adverse events (AEs) within 6 weeks post vaccination was 49.82% overall (410/823, 941 cases), 50.73% (209/412, 474 cases) in the NBP608 group, and 48.91% (201/411, 467 cases) in the comparator group. The difference in AE rate between the two groups was not statistically significant (P = 0.6010). Most AEs were mild, with a rate of 83.12% in the NBP608 group and 75.37% in the comparator group. Thus, NBP608 is non-inferior to Zostavax® in terms of inducing the immune response and can be safely administered to adults aged 50 years or older. ClinicalTrials.gov Identifier: NCT03120364.
13
项与 Herpes zoster vaccine (SK Chemicals) 相关的新闻(医药)2024-09-17
摘要:慢性传染病是指从发病到治愈或死亡需要较长时间的疾病,最近出现了使用治疗性疫苗来根除疾病。目前,基于各种疫苗配方开发慢性传染病治疗性疫苗的临床研究正在进行中,信使RNA疫苗平台最近的成功以及将其应用于治疗性疫苗的努力正在对征服慢性传染病产生积极影响。然而,与预防性疫苗相比,治疗性疫苗开发的研究仍然相对缺乏,因此需要更多地关注治疗性疫苗的开发,以克服慢性传染病对人类健康造成的威胁。为了加快未来慢性传染病治疗性疫苗的开发,有必要建立适合每种慢性传染病特点的治疗性疫苗的明确概念,以及标准化疫苗有效性评估方法、安全标准/参考物质和简化疫苗审批程序。1.背景
尽管许多传染病是急性的,但当今世界上由感染引起的大多数死亡和疾病都是由慢性感染引起的。全球有许多人患有慢性传染病,且人数不断增加,因此制定有效的慢性传染病应对策略迫在眉睫。由于慢性传染病具有潜伏感染和复发的潜力,因此针对大量已感染的携带者开发治疗方法而不是针对健康人群进行预防尤为重要。由于致病病原体持续存在于体内,慢性传染病往往难以通过单一治疗治愈,长期治疗可能导致对治疗耐药的突变株的发展。事实上,有报道称在许多慢性传染病中存在多重耐药病原体,这表明了药物治疗在慢性传染病治疗中的局限性。
在这种情况下,使用“治疗性”疫苗作为慢性传染病的治疗策略的方法最近受到了关注。“治疗性”疫苗利用机体的免疫机制来缓解感染引起的症状或防止感染病原体的再激活,因此治疗效果无需担心耐药性或副作用。同时,使用治疗性疫苗来应对慢性传染病将克服现有药物治疗的局限性,并实现更有效的治疗。为了在未来制定有效的慢性传染病应对策略,有必要准确了解治疗性疫苗的研发趋势。这篇综述研究了临床需求高的、主要慢性传染病的治疗性疫苗开发的现状,也涵盖在此基础上当前应考虑的问题和解决这些问题的改进策略。2.人乳头瘤病毒
已知人乳头瘤病毒(人乳头瘤病毒)会感染粘膜鳞状细胞或皮肤,并导致生殖器附近的疣或乳头瘤,或子宫、肛门和生殖器的恶性肿瘤。据统计,全球4.5%的癌症与人乳头瘤病毒感染有关,其中约80%已知是宫颈癌。Gardasil(Merck&Co.Inc.,Rahway,NJ,USA)和Cervarix(GlaxoSmithKline,London,UK)目前被用作HPV预防性疫苗,但这些疫苗在治疗已经感染该病毒的患者方面效果甚微,目前还没有疫苗被批准用于治疗。众所周知,潜伏HPV感染期间表达的E6和E7蛋白分别通过抑制p53和pRB的活性来诱导肿瘤发生。因此,肿瘤蛋白E6和E7被认为是HPV治疗性疫苗的两种最重要的目标抗原,并被广泛用作大多数正在开发的HPV治疗性疫苗的靶点。目前,正在努力基于各种疫苗制剂开发用于治疗由HPV感染引起的宫颈癌的疫苗(表1)。
表1.针对HPV的治疗性疫苗临床试验现状
HPV,人乳头瘤病毒;信使RNA。
a)代表性临床研究的ClinicalTrials.gov注册号。3.EB病毒
EB病毒(EBV)感染是人类最常见的感染之一,主要通过唾液传播。大多数感染患者没有任何特殊症状,但在免疫功能低下的患者中,它可以引起恶性肿瘤,如淋巴瘤、胃癌和鼻咽癌。因此,国际癌症研究机构将这种病毒归类为明显对人类致癌的第1组危险因素。截至2017年,全球约报告了265,000例(18%)和164,000例死亡(17%),由EBV相关淋巴瘤、霍奇金淋巴瘤、鼻咽癌和胃癌导致。
在EBV潜伏感染期间表达的潜伏蛋白,如EBNA1、LMP1和LMP2,在EBV相关肿瘤的癌变中起着重要作用。因此,目前正在研究和开发的用于治疗EBV慢性感染的疫苗主要使用EBV潜伏蛋白作为靶抗原,并且基于这些抗原的各种候选疫苗目前正在进行早期临床研究(表2)。
表2.EBV治疗性疫苗临床试验现状
EBV,EB病毒;信使RNA。
a)代表性临床研究的ClinicalTrials.gov注册号。4.巨细胞病毒
巨细胞病毒(CMV)主要以人和非人灵长类动物为宿主,普遍感染各年龄段人群。一旦被感染,它会终生潜伏,当宿主免疫力下降时会发生反应,引起各种症状。它可以感染大多数消化器官,包括食道、胃、肝脏、胰腺和大肠,当它发展为严重疾病时,会导致溃疡、肝炎、肠梗阻和结肠炎。此外,CMV肺部感染引起的肺炎可能危及生命,CMV眼部感染引起的视网膜炎有时会导致失明。
由于CMV的慢性感染在潜伏感染期间很少表现出症状,病毒的再感染和再激活会引起临床上重要的问题,因此目前正在开发主要靶向可中和病毒颗粒的包膜蛋白的治疗性疫苗(表3)。
表3.巨细胞病毒治疗性疫苗临床试验现状
CMV,巨细胞病毒;信使RNA。
a)代表性临床研究的ClinicalTrials.gov注册号。5.水痘带状疱疹病毒
水痘带状疱疹病毒(VZV)是一种根据感染类型引起两种疾病的病原体。由VZV引起的原发性感染表现为水痘(水痘),但在受感染的病毒仍然潜伏在背根神经节中,主要在免疫功能低下的患者或50多岁或以上的患者中重新激活,导致带状疱疹。全世界带状疱疹的年发病率为每1000人1.2至3.4例,已知75岁以上的人超过每1000人10例。患带状疱疹的终生风险估计为10%-20%。带状疱疹的临床症状范围很广,从无皮疹的疼痛到轻度皮疹,再到有播散的重度皮疹。在免疫功能低下的患者中,它会导致严重的神经系统疾病,如导致视力丧失的外视网膜坏死、胃肠道疾病和血管病。此外,带状疱疹后神经痛(PHN)是带状疱疹的代表性后遗症,是一种发生在带状疱疹发作后约一个月的神经病理性疼痛综合征。PHN通常很严重,已知发病率随着年龄的增长而增加。
水痘和带状疱疹是由同一病原体感染引起的,所以基本上每次感染都可以使用相同的疫苗。为了抑制引起带状疱疹的病毒复发,必须使用比预防初始感染高得多的抗原剂量。因此,有必要区分水痘和带状疱疹疫苗。目前批准的带状疱疹疫苗(治疗性疫苗)显示的剂量水平比带状疱疹疫苗(预防性疫苗)高约14倍。
目前,两种减毒活疫苗(ZOSTAVAX; Merck & Co. Inc. and SKYZoster; SK Bioscience, Seongnam, Korea)和一种重组疫苗(SHINGRIX; GlaxoSmithKline)是最广泛使用的被批准的带状疱疹疫苗。由于安全性问题,对使用亚单位疫苗如SHINGRIX的需求正在增加,使用各种亚单位制剂的其他带状疱疹疫苗正在临床试验中(表4)。
表4.针对VZV的治疗性疫苗的临床试验现状
VZV,水痘带状疱疹病毒;信使RNA。
a)代表性临床研究的ClinicalTrials.gov注册号。b)自扩增RNA疫苗。6.单纯疱疹病毒
单纯疱疹病毒(HSV)主要感染皮肤和粘膜,分为1型(HSV-1)和2型(HSV-2)。因此,HSV-1通常与口腔和眼部疾病有关,但由HSV-1引起的性传播疾病的比例趋于增加。另一方面,HSV-2是世界上最广泛的性传播疾病之一,每年约有2300万新感染病例。根据世界卫生组织(世卫组织)的数据,2016年估计有多达1.92亿人感染了生殖器HSV-1病毒,多达4.91亿人感染了HSV-2病毒。由于生殖器疱疹的临床治疗需求高于其他疱疹,与HSV-1相比,开发靶向HSV-2的治疗性疫苗的需求往往更受重视。
初次感染后,HSV在宿主的神经节中保持休眠或潜伏,并可周期性地重新激活以引起慢性感染。由于HSV在潜伏感染期间不表现出任何特殊的临床症状,因此有可能开发出与预防性疫苗基本靶向相同抗原的HSV治疗性疫苗。为了有效地抑制HSV的再激活,许多研究正在进行中,以发现可以诱导强中和免疫应答的靶抗原。此外,由于病毒的性质感染粘膜、可诱导粘膜免疫的特定制剂和接种途径也被认为是重要因素。目前,用于开发靶向HSV的治疗性疫苗的几项临床试验正在进行中(表5)。
表5.针对单纯疱疹病毒的治疗性疫苗临床试验现状
HSV,单纯疱疹病毒;信使RNA。
a)代表性临床研究的ClinicalTrials.gov注册号。7.乙型肝炎病毒
乙型肝炎病毒(HBV)是一种引起急性和慢性乙型肝炎的病毒,通过受感染的血液或体液传播。据估计,全球有超过20亿人感染HBV病毒,其中约2.5亿人慢性感染乙型肝炎。
慢性HBV感染定义为HBV持续超过6个月,在血液中检测到乙型肝炎表面抗原(HBsAg)。在慢性感染HBV的情况下,感染者的免疫反应(尤其是T细胞反应)减弱,出现功能障碍,因此认为慢性HBV患者的HBV基因组完全清除是不可能的。因此,针对慢性HBV感染的治疗性疫苗的最终目标被提出为克服慢性携带者中HBV特异性T细胞功能下降的“功能性治疗”。目前,一种作为病毒样颗粒制剂开发的用于慢性HBV患者的治疗性疫苗已被批准在古巴使用,其他几种候选疫苗目前正在进行临床试验(表6)。
表6.HBV治疗性疫苗临床试验现状
HBV,乙型肝炎病毒;HBsAg,乙型肝炎表面抗原;HBcAg,乙型肝炎核心抗原。
a)代表性临床研究的ClinicalTrials.gov注册号。8.结核分枝杆菌
结核病(TB)是由结核分枝杆菌感染引起的代表性细菌性慢性传染病。它主要感染肺部并引起呼吸系统疾病。此外,细菌侵入其他器官可引起脑膜炎、胸膜炎和腹膜炎。在潜伏感染状态下,没有症状,但当感染患者免疫力减弱时,感染的病原体进展为活动性结核病。根据世卫组织的数据,2022年全球结核病患者人数为1060万,与上一年(1010万)相比增加了4.5%。此外,死于结核病的人数为160万,比前一年(150万)增加了6.7%。
结核病治疗需要相当长期的抗生素管理,但抗生素耐药菌株的出现变得越来越频繁,这对治疗慢性结核病构成了主要障碍。此外,据报道唯一批准的结核病疫苗BCG(卡介苗)疫苗对青少年或成人不是很有效,因此非常需要开发一种适用于治疗慢性结核病的新疫苗。因此,正在继续努力开发针对慢性和潜伏性结核病感染的新型治疗性疫苗(表7)。
表7.结核病治疗性疫苗临床试验现状
rBCG,重组卡介苗;LLO,李斯特菌溶血素O。
a)代表性临床研究的ClinicalTrials.gov注册号。9.结论
治疗性疫苗是一个相对较新的概念,到目前为止,有一种趋势是专注于靶向恶性肿瘤的新抗原而不是传染病的癌症治疗(治疗性癌症疫苗)。另一方面,与预防性疫苗相比,针对传染病的治疗性疫苗的研发趋势仍然相对不足。许多预防性疫苗已经被批准使用,许多候选疫苗的临床试验正在进行中。然而,目前还没有治疗慢性传染病的疫苗,带状疱疹疫苗除外,进入临床试验的开发研究数量非常有限。
有几个因素导致相对缺乏针对慢性传染病的治疗性疫苗的开发。首先,在慢性感染性疾病的情况下,慢性感染性疾病的临床表现因病原体的特性而异,因此治疗性疫苗的主要靶标也因受试者而表现出非常不同的方面。因为真空-不同治疗靶点的电影不可避免地需要不同的开发策略、疫苗疗效评估技术和临床审批标准等因素,治疗性疫苗应根据疫苗的靶点症状和作用机制进行分组。因此,有必要对适合每种慢性感染特点的疫苗开发和评价方法进行研究。本研究中提出的治疗性疫苗组如下:(1)用于对症治疗的疫苗,(2)用于预防复发的疫苗,和(3)用于缓解(消除)感染因子的疫苗。治疗性疫苗缺乏标准化免疫原性分析技术是另一个需要解决的因素。已经转变为慢性感染的疾病的适当治疗需要一种可以直接杀死感染细胞的方法。由于细胞免疫在其中起主要作用,为了开发治疗性疫苗,有必要标准化T细胞免疫应答的评估方法。然而,与人类免疫不同,细胞免疫的测量需要实验上复杂的过程和设备,并且因为细胞免疫的活性对于每个个体/时期/组织显示出非常大的变化,所以仍然没有明确的标准方案和程序。
然而,已经证实,全球正在努力开发基于各种制剂的治疗性疫苗,用于具有高临床需求的代表性慢性传染病。特别是,由于信使RNA(mRNA)疫苗最近在2019年冠状病毒病大流行的成功,针对长期以来被认为无法治愈的各种传染病的疫苗开发的新可能性正在出现,并且正在尝试通过将mRNA制剂应用于治疗性疫苗来开发。基于mRNA平台的治疗性疫苗的研究目前正在进行本研究中调查的大多数慢性传染病的临床试验,预计这种新型平台可以在未来治疗性疫苗的开发中发挥积极作用。
为了开发成功的治疗性疫苗,随着疫苗配方技术和免疫治疗技术的进步,测试方法的标准化和验证疫苗物质功效的评价标准的建立是必须建立的附加要素。为了实现这一目标,对病理的研究每种慢性传染病的逻辑特征和对防御/治疗每种慢性感染所需的免疫因素的准确理解是先决条件。还包括努力发现潜在感染和再激活特异性抗原,开发细胞介导的免疫原性测量技术,并建立标准/参考材料。如果在国家层面与学术界和工业界分享这些当前的问题,并在必要的领域集中和支持研究能力,预计未来将有可能通过治疗性疫苗有效应对慢性传染病。
参考文献:Park PG, Fatima M, An T, Moon YE, Woo S, Youn H, Hong KJ. Current development of therapeutic vaccines for the treatment of chronic infectious diseases. Clin Exp Vaccine Res. 2024 Jan;13(1):21-27. doi: 10.7774/cevr.2024.13.1.21. Epub 2024 Jan 31. PMID: 38362373; PMCID: PMC10864879.
识别微信二维码,添加生物制品圈小编,符合条件者即可加入
生物制品微信群!
请注明:姓名+研究方向!
版
权
声
明
本公众号所有转载文章系出于传递更多信息之目的,且明确注明来源和作者,不希望被转载的媒体或个人可与我们联系(cbplib@163.com),我们将立即进行删除处理。所有文章仅代表作者观点,不代表本站立场。
疫苗信使RNA临床研究
2024-03-25
·药智网
后疫情时代的第一年,国内疫苗行业可谓惨淡。不仅是新冠疫苗需求降至冰点,非新冠疫苗也受到波及。A股12家疫苗公司2023年前三季度只有4家实现营收正增长,包括智飞生物、华兰疫苗、百克生物和康乐卫士。近日,4家之一的百克生物发布2023年年报。年报显示,2023年实现营业收入18.25亿元,同比增长70.3%;归母净利润5.01亿元,同比增长175.98%。萧条环境下,百克生物业绩逆势增长,背后的玄机是什么?01百亿蓝海市场,双雄争霸开启带状疱疹是一种疼痛性、传染性神经皮肤疾病,由潜伏性水痘-带状疱疹病毒(VZV)再激活引起。根据血清学证据,成人VZV感染的患病率超过90%,当人体免疫力下降时,VZV病毒就可能重新激活引发带状疱疹。带状疱疹随着年龄增长,发病率显著增加。在中国,每年约有565万人患上带状疱疹,随着人口老龄化的加剧,带状疱疹发病率将不断上升。带状疱疹愈后仍会引起疼痛,接种疫苗是最好的预防措施。然而除了美国以外,多数国家带状疱疹疫苗接种率还处于很低水平。弗若斯特沙利文报告显示,2021年美国50岁及以上人口的带状疱疹接种率为26.8%,而中国和欧盟分别为0.1%和5.2%。在百克生物的疫苗上市之前,全球共有三款带状疱疹疫苗获批,分别是默沙东的Zostavax、葛兰素史克(GSK)的Shingrix、SK化工株式会社的SkyZoster(仅在韩国销售),其中Zostavax由于保护效力较低已于2020年11月在美国停产。因此,GSK的Shingrix几乎占据100%带状疱疹疫苗市场,2022年销售额达36.46亿美元,同比增长58.79%,是仅次于HPV疫苗和13价肺炎疫苗的全球第三大畅销疫苗。2019年5月,Shingrix在国内获批上市,成为国内唯一上市的带状疱疹疫苗。但上市后的Shingrix恰逢新冠疫情爆发,疫苗销量受到影响。2023年1月,百克生物的带状疱疹减毒活疫苗“感维”在国内获批上市,成为国内第二款获批的带状疱疹疫苗。与GSK的Shingrix相比,技术路线上,百克生物感维是减毒疫苗,保护效力低于Shingrix,但在不良反应发生率方面带状疱疹减毒活疫苗更具优势,安全性更好。在价格方面,感维是1384元/剂,需接种一次;Shingrix是1608元/剂,需接种两次。此外,感维获批用于40岁以上人群,相对于Shingrix接种人群(50岁及以上)更加广泛。占据了价格和覆盖面优势的百克生物,在新产品上市的第一年,就在30个省、自治区、直辖市完成准入,并拿下了8.8亿元的销售额,产品毛利率高达97.5%,成为其最重要收入来源之一。同时,由于国内的带状疱疹疫苗尚处于起步阶段,市场渗透率极低。未来随着人口老龄化程度加深、带状疱疹患病率不断上升、公众接种意识的提高,国内带状疱疹疫苗市场规模将迅速扩张,预计2025年将增加至108亿元,2030年将达到281亿元。国内带状疱疹疫苗市场规模图片来源:参考资料3巨大的市场潜力让GSK也开始加大销售力度。2023年10月,与智飞生物签署联合推广协议,并定下三年最低采购采购金额共计206.4亿元。二者站在同一起跑线上,国内带状疱疹疫苗市场双雄争霸才刚刚开始。02背靠长春高新,基本盘稳固百克生物敢于与GSK、智飞生物争雄的底气来自长春高新。百克生物的前身是2004年成立的百克药物研究所,由长春高新与其控股子公司百克药业共同投资设立。2021年百克生物在科创板挂牌上市。截至目前,长春高新直接持有公司41.54%的股份。在母公司支持下,成立以来,百克生物陆续获批了水痘疫苗、狂犬疫苗、鼻喷流感疫苗以及带状疱疹减毒活疫苗4种疫苗产品,其中狂犬疫苗从2018年下半年起陆续停产进行技术升级。除2023年刚获批的带状疱疹疫苗外,水痘疫苗、鼻喷流感疫苗分别获批于2008年及2020年,是百克生物的三大基本盘。水痘疫苗一直都是百克生物最主要的营收来源,在2023年之前,水痘疫苗的收入比重稳定在75%以上。即使在2023年,水痘疫苗的收入占比依旧达到44.93%。百克生物的水痘疫苗是世界上首个有效期为36个月的水痘减毒活疫苗,市场占有率常年稳定在20%以上,部分年份市场排名第一。在满足国内市场的前提下,百克生物积极推动水痘疫苗出口,目前已出口至印度、加纳等国家,并与俄罗斯签署合作协议,提升水痘疫苗在俄罗斯等地的可及性。国内水痘疫苗市场格局图片来源:参考资料4百克生物的鼻喷流感疫苗是三价减毒活疫苗,适用于3-17岁人群,是国内独家经鼻喷方式接种的流感减毒活疫苗。与传统注射疫苗相比,鼻喷疫苗通过鼻黏膜途径进行免疫接种,可诱导局部黏膜免疫、中和抗体以及细胞免疫等。2023年,百克生物鼻喷流感疫苗销售收入1.2亿元,同比增长6.85%。带状疱疹疫苗、水痘疫苗和鼻喷流感疫苗成为共同驱动百克生物业绩增长的三大引擎。03研发持续推进,布局MRNA疫苗虽然在2023年实现了历史性的突破,但百克生物面临的竞争压力一点都不小。人口出生率下滑,水痘疫苗和流感疫苗接种人群减少,存量市场竞争加剧;拳头产品带状疱疹疫苗也有多家企业在研,进展最快的绿竹生物重组带状疱疹疫苗,已于2023年9月启动III期临床研究,预计最快将在2026年前后获批上市。为了进一步扩充产品管线,近年来百克生物持续加大研发投入。研发费用从2019年的6516万元,增长至2023年的1.98亿元,年复合增长率高达32.05%。研发投入增长下,百克生物疫苗研发多点开花。截至目前,百克生物已拥有14款在研疫苗和2款在研全人源单克隆抗体,处于已获批临床试验及申请注册阶段的项目6项。其中液体鼻喷流感疫苗即将申请上市许可;百白破疫苗(三组分)已完成Ⅰ期临床试验,正在进行Ⅲ期临床试验的准备工作;狂犬单抗正在进行I期临床研究;冻干狂犬疫苗(人二倍体细胞)以及破伤风单抗的临床试验申请已获得批准,即将开展Ⅰ期临床研究。此外,百克生物还布局了包括RSV疫苗及抗体、阿尔茨海默病治疗性疫苗等在内极具市场潜力的产品管线。近些年极为火热的MRNA疫苗赛道,百克生物也在加大投入布局。2023年6月,与传信生物签订投资协议,拟分步对其进行增资及股权收购,并最终持有其100%股权。2021年4月成立的传信生物,拥有进全球领先的LNP递送技术,以及完整的mRNA药物研发和规模化生产体系,并以此开发新型传染病和肿瘤mRNA疫苗。百克生物收购传信生物后,有利于其加快建设mRNA技术平台,全面快速推进多种mRNA疫苗的研发。在新疫苗研发上,百克生物研发管线的多元化和差异性较国内同行有明显优势。随着未来产品不断丰富,将为业绩增长寻找新的增长点,并可以有效抵御经济环境及行业政策给企业带来的不利影响。04结语政策指引下,国内疫苗产业正在发生质的变化。百克生物凭借前瞻性的布局,在未来的市场盛宴中必将占据一席之地。参考资料1.百科生物年报,官网2.《带状疱疹疫苗市场迎来蓬勃发展,行业迎来黄金时期》,生物报,2023-09-173.《带状疱疹疫苗行业专题:竞争格局良好,带状疱疹疫苗大单品未来可期》,民生医药,2023-10-274.《百战克疫稳增长,带疱疫苗再争锋》,国投证券,2024-01-08声明:本内容仅用作医药行业信息传播,为作者独立观点,不代表药智网立场。如需转载,请务必注明文章作者和来源。对本文有异议或投诉,请联系maxuelian@yaozh.com。责任编辑 | 金银花转载开白 | 马老师 18996384680(同微信)商务合作 | 王存星 19922864877(同微信) 阅读原文,是受欢迎的文章哦
财报疫苗上市批准
2023-10-27
·药智网
“天下武功,唯快不破”,只有先于竞争对手获批新产品,取得先发制人的竞争优势,才能得到市场的高度认可。这点可以在百克生物身上得到验证。近日,百克生物公布了亮眼的“成绩单”:凭借带状疱疹疫苗先发优势实现快速放量,2023年前三季度实现总营收12.43亿元,超过去年全年,同比增长43.6%,归母净利润为3.31亿元,同比增长56.31%。百克生物正式开启「带状疱疹疫苗」时代。01百克生物的“三驾马车”此前,贡献公司业绩的核心产品主要为水痘疫苗和鼻喷流感减毒活疫苗,直到新产品带状疱疹疫苗于2023年1月获批上市,百克生物迎来了拉动业绩增长的“第三驾马车”。从业绩表现看,2023年前三季度单季分别实现总营收1.79亿元(+30.21%)、3.8亿元(+25.44%)、6.8亿元(+60.91%),归母净利润为1838万元(6.15%)、9300万元(+65.32%)、2.2亿元(+58.92%)。第三季度业绩实现高速增长,主要由带状疱疹疫苗加速放量贡献。根据百克生物发布的最新投资者关系活动记录表,目前带状疱疹疫苗已有30个省、自治区、直辖市完成准入,并已获得23批批签发。另外,据华鑫证券预计,该产品今年可贡献6-8亿元的营收。数据来源:根据百克生物财报、同花顺财经整理得益于核心产品实现快速增长,百克生物的盈利能力持续提升,其中毛利率实现连续四个季度大幅爬升,从2022年第四季度单季的84.6%提升至2023年第三季度单季的89.48%,净利率也实现连续三个季度上行,从10.24%攀升至26.63%。不过,虽然百克生物已有“三驾马车”拉动业绩,但市场竞争较为激烈的水痘疫苗仍是主要收入来源,最近两年总营收占比高达80%以上。正如百克生物在财报中所言,“水痘疫苗市场已有包括公司在内的5个厂家的产品上市,公司水痘疫苗虽然目前市场份额占据领先地位,但伴随出生率下降导致的市场容量萎缩,不排除未来产品销量下降的风险。”另外,国内还有多款竞品即将入场竞争,目前万泰生物的冻干水痘减毒活疫苗(1-50岁)已处于报产阶段,针对12月龄-12岁的疫苗已处于Ⅱb期临床;科兴疫苗和上海所的水痘减毒活疫苗(13岁及以上)已处于Ⅲ期临床,市场竞争激烈程度可见一斑。国内水痘疫苗研发进展图片来源:华鑫证券流感疫苗市场的竞争更为激烈。2022年,百克生物的鼻喷流感疫苗实现收入1.14亿元,总营收占比为10.64%,对业绩贡献较小,这其中也有疫情影响的因素。作为国内独家经鼻喷接种的流感减毒活疫苗,鼻喷流感疫苗的接种对象为3-17岁人群,相较大多数针对6月龄-3岁儿童的流感疫苗产品,具备一定的差异化优势。正因如此,新产品带状疱疹疫苗成为了百克生物必须拿下的重要阵地。02带状疱疹疫苗:必须拿下的百亿赛道庞大的目标人群叠加蓝海赛道,让带状疱疹疫苗呈现出巨大的市场潜力。带状疱疹疫苗是用于预防中老年人发生带状疱疹的疫苗,而我国40岁以上的中老年人高达上亿。在百克生物获批之前,全球仅有默沙东的Zostavax、SK Bioscience的SkyZoster和葛兰素史克(GSK)的Shingrix获批上市,但市场份额主要被GSK占据。Shingrix在上市后首个完整销售年即突破10亿美元销售额,2022年实现收入近30亿英镑,预计2026年将超过40亿英镑,是全球名列前茅的畅销疫苗品种。中国带状疱疹疫苗市场规模高达百亿,目前仅有GSK的Shingrix上市销售。根据国信证券研报测算(按中性估计),国内带状疱疹疫苗市场空间将分别于2025年、2027年达到132亿元、247亿元。此外,目前布局带状疱疹疫苗的国产企业较少,而且大多仍处于临床早期阶段。最接近上市的是绿竹生物的重组带状疱疹疫苗(CHO细胞),已于2023年Q3进入Ⅲ期,预计2025年Q4实现商业化。这意味着,百克生物和GSK将在未来几年形成相对稳定的双寡头竞争格局。国内各技术路线带状疱疹疫苗研发进度图片来源:国信证券对比来看,GSK的Shingrix为重组蛋白疫苗,针对的是50岁以上人群,注射剂次为2针,价格为3216元;百克生物的技术路线为减毒活疫苗,适用于40岁及以上成人,受众人群更大,且仅需注射1针,价格优势显著(1369元/针),副作用发生率也相对较低。从销售策略看,百克生物在国内采用直销模式,由公司自有营销团队制定市场推广策略,包括区域销售督导、市场医学督导等,同时聘请专业市场服务商(CSO公司)开展具体的市场推广活动,目前已有约80家带状疱疹疫苗推广商。GSK则选择与具有丰富疫苗销售经验的智飞生物合作,根据双方签署的独家经销和联合推广协议:协议期限为2023年10月8日起至2026年12月31日止,2024-2026年年度最低采购金额分别为34.4亿元、68.8亿元、103.2亿元。尽管当前国内带状疱疹疫苗市场尚处蓝海阶段,但百克生物面对的竞争压力也不小。03后备研发管线丰富,流感疫苗能否撑起大旗?俗语说,“不要把所有的鸡蛋放进一个篮子。”深谙多元化增长策略的百克生物,布局了丰富的研发管线。目前,百克生物拥有13项在研疫苗和3项在研的用于传染病防控的单克隆抗体,主要包括百白破疫苗(三组分)、液体鼻喷流感疫苗、狂犬单抗、破伤风单抗等,4个在研项目已处于临床研究阶段,12个在研项目处于临床前研究阶段。百克生物主要在研产品研发进展图片来源:华鑫证券在流感疫苗管线方面,百克生物已完成液体鼻喷流感疫苗Ⅱ期临床研究,并向国家药监局药品审评中心提交沟通交流会申请,同时计划于2024年申请佐剂流感疫苗临床研究。为了丰富流感疫苗产品系列,百克生物于10月23日发布了一项高达8.05亿元的投产计划:投资年产1000万人份流感病毒裂解疫苗(BK-01佐剂)项目(目前处于临床前阶段)。据公告显示,此次流感病毒裂解疫苗(BK-01剂)项目适用人群为6月龄及以上人群,进而实现覆盖全人群的流感疫苗产品组合;同时,通过佐剂能够更好地刺激免疫反应,佐剂流感疫苗预计可在60岁及以上老年人群中产生较高抗体水平,达到良好的保护效果。处于临床研究阶段的管线中,百白破疫苗(三组分)已完成Ⅰ期临床研究,正在进行Ⅲ期临床试验的准备工作;狂犬单抗已进入I期临床研究阶段。另外,破伤风单抗的临床试验申请已受理,冻干狂苗(MRC-5细胞)已完成pre-IND,重组带状疱疹疫苗计划于2024年申请临床研究,阿尔茨海默病治疗性疫苗和HSV-2疫苗等多个研发项目处于临床前研究阶段。除此以外,百克生物还布局了新兴技术,于2023年上半年与传信生物签订投资协议,对后者进行增资及股权收购,以加快搭建mRNA疫苗技术平台,进一步丰富公司研发管线。04结语不难看出,尚处于蓝海阶段、市场潜力更大的带状疱疹疫苗,已成为拉动百克生物业绩快速增长的主力军。后续研发管线也具备差异化特点,其中能够覆盖全人群的流感疫苗也是一大看点,但未来能否撑起业绩大旗,值得持续关注。参考资料:1.百克生物财报、公告2.《疫苗行业系列报告(5):带状疱疹疫苗是全球重磅品种,国内商业化空间广阔》,国信证券3.《主营业务稳步回升,带状疱疹疫苗注入新活力》,华鑫证券声明:本内容为作者独立观点,不代表药智网立场。如需转载,请务必注明文章作者和来源。对本文有异议或投诉,请联系maxuelian@yaozh.com。责任编辑 | 巴巴转载开白 | 马老师 18996384680(同微信)商务合作 | 王存星 19922864877(同微信) 阅读原文,是昨天最受欢迎的文章哦
财报疫苗临床3期上市批准
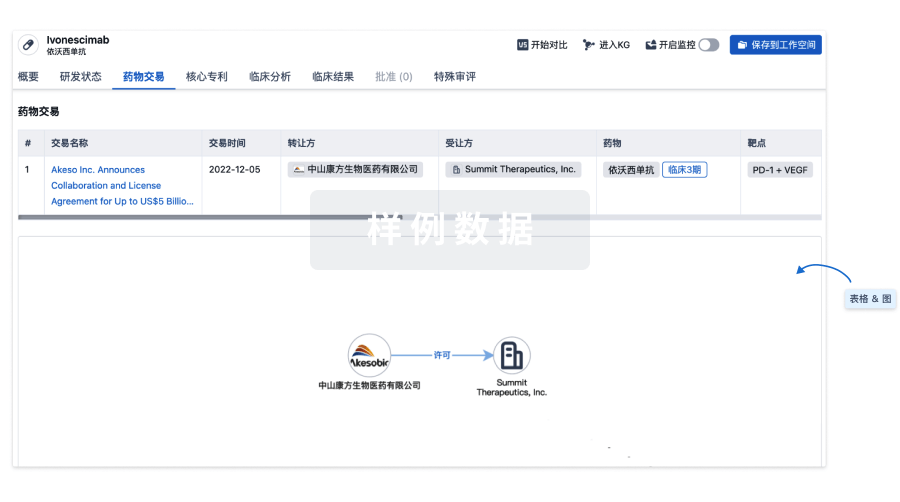
100 项与 Herpes zoster vaccine (SK Chemicals) 相关的药物交易
登录后查看更多信息
外链
| KEGG | Wiki | ATC | Drug Bank |
|---|---|---|---|
| - | - | - |
研发状态
批准上市
10 条最早获批的记录, 后查看更多信息
登录
| 适应症 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|
| 带状疱疹 | 韩国 | 2017-09-29 |
未上市
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 水痘 | 临床3期 | 菲律宾 | 2016-07-14 | |
| 接种疫苗 | 临床1期 | 美国 | 2012-11-01 |
登录后查看更多信息
临床结果
临床结果
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
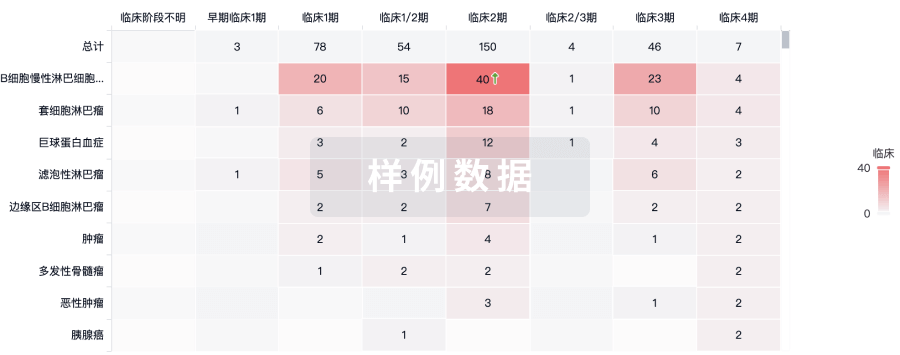
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用

