更新于:2024-11-21
Loncastuximab
更新于:2024-11-21
概要
基本信息
非在研机构- |
最高研发阶段药物发现 |
首次获批日期- |
最高研发阶段(中国)- |
特殊审评- |
序列信息
Sequence Code 315596552L
来源: *****
Sequence Code 315596551H
来源: *****
关联
100 项与 Loncastuximab 相关的临床结果
登录后查看更多信息
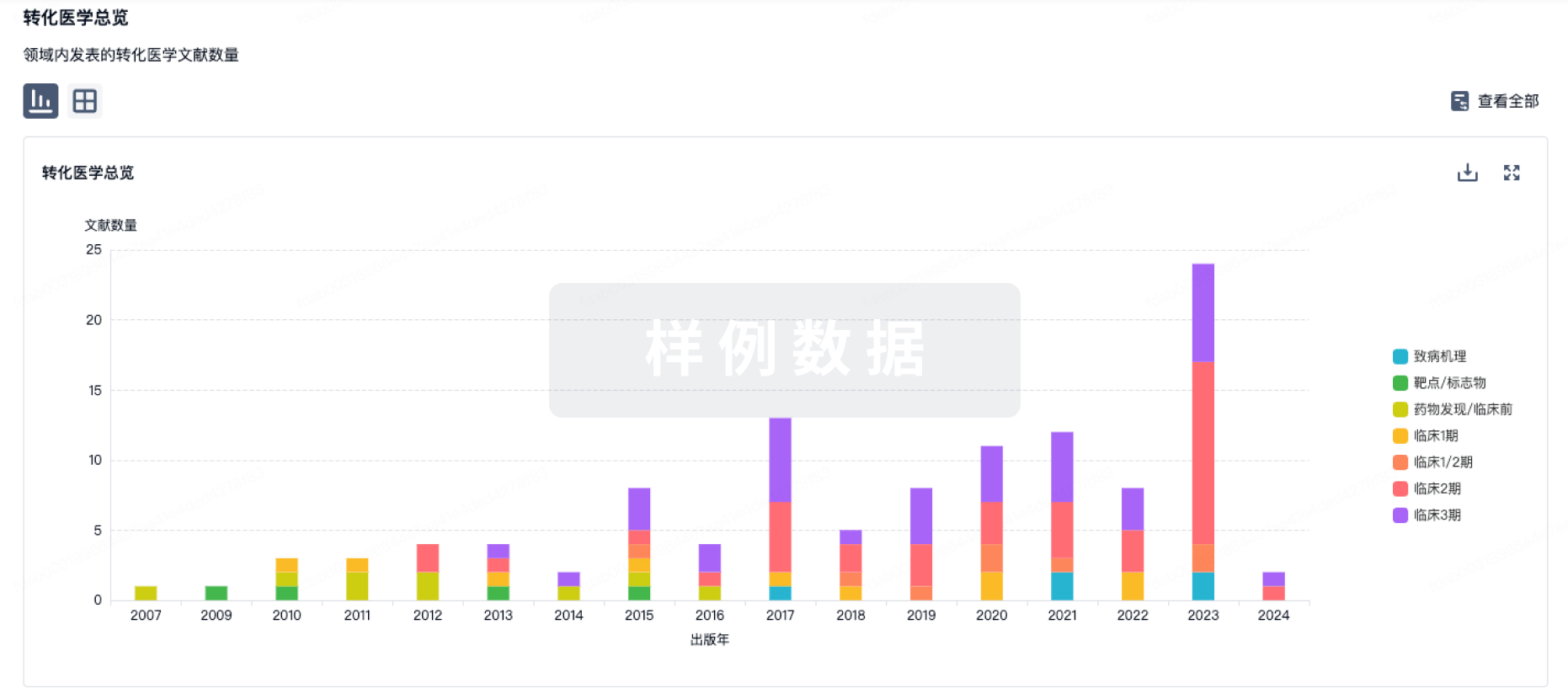
100 项与 Loncastuximab 相关的转化医学
登录后查看更多信息
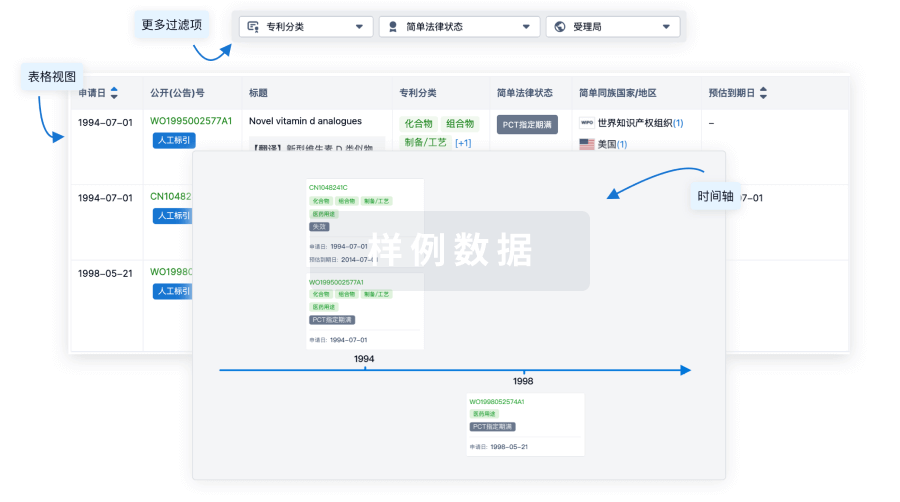
100 项与 Loncastuximab 相关的专利(医药)
登录后查看更多信息
6
项与 Loncastuximab 相关的文献(医药)2023-07-01·Cancer research and treatment
Efficacy of Salvage Treatments in Relapsed or Refractory Diffuse Large B-Cell Lymphoma Including Chimeric Antigen Receptor T-Cell Therapy: A Systematic Review and Meta-Analysis.
Review
作者: Kim, Seok Jin ; Yoon, Sang Eun ; Cho, Jinhyun ; Kim, Won Seog ; Kim, Jinchul
2022-07-01·European review for medical and pharmacological sciences
Treatments for relapsed-refractory diffuse large B-cell lymphoma: comparison of overall survival outcomes observed with four novel agents.
Article
作者: Caccese, E ; Messori, A
2022-05-01·Clinical Lymphoma Myeloma and Leukemia4区 · 医学
The AntiCD19 Antibody Drug Immunoconjugate Loncastuximab Achieves Responses in DLBCL Relapsing After AntiCD19 CAR-T Cell Therapy
4区 · 医学
Article
作者: Solh, Melhem ; Hamadani, Mehdi ; Reid, Erin ; Ardeshna, Kirit M ; Caimi, Paolo F ; Kahl, Brad S ; Lunning, Matthew ; Zain, Jasmine ; Ai, Weiyun
4
项与 Loncastuximab 相关的新闻(医药)2024-10-09
摘要:化学免疫疗法和细胞疗法是复发/难治性(R/R)淋巴瘤治疗的主要手段。这些治疗中出现的耐药性和常见毒性限制了它们在实现期望的响应率和持久缓解方面的作用。抗体-药物偶联物(ADC)是一种新型靶向疗法,已证明在治疗包括淋巴瘤在内的各种癌症中具有显著的疗效。迄今为止,已有三种ADC药物被批准用于不同类型的淋巴瘤,这标志着该领域取得了重大进展。在本文中,我们旨在回顾ADC的概念及其在淋巴瘤治疗中的应用,分析目前批准的药物,并讨论ADC开发正在进行的进展。
1.引言
淋巴瘤是一组来自不同类型淋巴细胞(B细胞、T细胞或自然杀伤(NK)细胞)在不同成熟阶段的克隆性增殖的恶性肿瘤。过去几十年来,不同类型淋巴瘤的发病率一直在增加。化学免疫疗法和细胞疗法仍然是不同亚型淋巴瘤常用的治疗手段。大多数化疗方案的治疗效果指数较窄,导致广泛的毒性。此外,耐药性的出现是最常见的原因之一,阻碍了它在复发和难治性(R/R)情况下的使用。针对表面抗原的单克隆抗体,如利妥昔单抗和奥比妥珠单抗,已经彻底改变了淋巴瘤的治疗。抗体-药物偶联物(ADCs)是一种高度靶向的药物,将针对特定表面抗原的单克隆抗体(mAb)与细胞毒素分子连接起来。毒素只传递给表达表面抗原的细胞,具有高度的肿瘤特异性和有限的系统暴露。美国食品药品监督管理局(FDA)已经批准了三种用于治疗淋巴瘤的ADC药物,分别是本妥昔单抗、波拉图单抗和洛卡图单抗。
在本文中,我们将回顾ADC的概念,重点关注它们的结构、工程和在淋巴瘤治疗中的作用。此外,我们将提供目前批准的ADC在这一设置中的综合分析,以及正在进行的进展的概述。这包括突出来自临床前和临床试验的有希望的结果,以及讨论下一代ADC开发的未来方向。
2.ADC的基本结构
ADC由抗体、药物(有效载荷或细胞毒素)和连接子组成。抗体结合恶性细胞表面表达的特定抗原。一旦结合,ADC被内化,细胞毒素有效载荷释放到细胞内,导致细胞周期终止和凋亡。在周围目标阴性细胞中也可以看到细胞毒性效应,当药物扩散到它们中并引起“旁观者杀伤”时,这是一种当有效载荷从被内化和降解的ADC释放或当药物释放到细胞外空间后从目标细胞释放时发生的细胞死亡。值得注意的是,为了获得更好的结果和更少的副作用,抗原和抗体之间的结合需要尽可能特异性。有效载荷的内化率、连接子的稳定性和相应抗体的选择是影响ADC在临床实践中使用的一些变量。
2.1. 单克隆抗体
选择合适的抗体是ADC工程中的关键步骤;它通常被设计为特异性结合癌细胞表面表达的目标抗原。理想的单克隆抗体应具有低免疫原性、低交叉反应性、长的血浆半衰期,以及对肿瘤细胞表面抗原的高结合亲和力。最常用的类别是免疫球蛋白G(IgG),更具体地说是IgG1亚型,因其血清稳定性。在ADC开发的早期阶段,主要使用小鼠来源的抗体。然而,这些抗体报告有很高的失败率,可能归因于它们缺乏临床效益,同时引起严重的免疫原性相关的不良效应。这些ADC也被人类抗小鼠抗体迅速清除,限制了它们的疗效。此外,这些早期ADC中使用的连接子在人体循环中不稳定,导致有效载荷过早释放,大大降低了效果并增加了毒性。自从出现显著降低免疫原性的人源化小鼠单克隆抗体以来,已经取代了小鼠抗体,导致更优化的设计,如2000年FDA批准的针对CD33阳性急性髓系白血病患者的首个ADC药物吉妥单抗奥佐米星。迄今为止,已有十四种ADC获得FDA市场批准,其中三种如前所述已获批准用于治疗淋巴瘤。其中,只有本妥昔单抗使用嵌合抗体。嵌合抗体是通过融合不同物种的域(例如,整个小鼠或兔的可变区与人类来源的恒定域)设计的。相比之下,人源化抗体含有嵌入人类来源的Fab区和恒定区的外来氨基酸段。因此,它们较少免疫原性,是更安全的选择。在全人抗体中,没有一部分是小鼠来源的,与人类化抗体相比,它们在免疫反应中的发生率更低;例如FDA批准的enfortumab vedotin。
2.2. 有效载荷
ADC的理想有效载荷应具有低免疫原性、长半衰期、小分子量、在抗体的水性环境中良好的溶解度、在循环和溶酶体中的高稳定性、体外亚纳摩尔半最大抑制浓度(IC-50)以及有助于与抗体结合的官能团,同时保持ADC的内化特性。每个抗体平均结合两到四个强效的细胞毒素分子。目前,ADC设计中最受欢迎的两类有效载荷是微管破坏剂和DNA靶向剂(图1)。
图1. 设计ADC时常用的十种不同有效载荷的分子结构
微管抑制剂可以根据它们的作用机制分为两大类。第一组包括微管稳定剂。这些药物通过抑制微管解聚和促进聚合来增强丝状体的稳定性,使丝状体功能降低。第二组由破坏微管的物质组成,阻止微管蛋白组装和成熟微管的发展。在ADC开发中使用和研究的主要微管抑制剂包括长春碱类、紫杉醇类、auristatins、美登素类、隐孔菌素、海葵素和圆盘菌素。auristatins如单甲基auristatin E (MMAE)通过阻止α-和β-微管蛋白单体聚合并触发凋亡来破坏微管并阻止细胞分裂。结合区域位于两个纵向排列的微管二聚体的β1-微管蛋白和α2-微管蛋白亚基之间。根据体外研究结果,auristatin-微管蛋白键合形成环状或螺旋形聚集体,改变微管的功能。长春碱类如长春新碱或长春碱,以及隐孔菌素和多拉斯他汀,诱导微管形成类似的弯曲结构构象。
在细胞周期的任何阶段,DNA损伤剂通过双链断裂、烷基化、插入和交联四种主要机制可以杀死癌细胞。最常用的DNA损伤有效载荷是卡利烯胺、二酮霉素、吡咯并苯并二氮杂环(PBD)、多柔比星和喜树碱类似物。针对BCL-2抑制剂、剪接体抑制剂和针对RNA聚合酶II的转录抑制剂等靶向药物是具有不同作用机制的额外有效载荷。
值得注意的是,根据FDA对15种含有PBD有效载荷的ADCs的肿瘤学分析,PBD有效载荷的毒性概况更高,这表明常见的不良事件包括可能的血管渗漏综合征、转氨酶升高、骨髓抑制、胃肠事件、代谢效应、肌肉骨骼事件、神经病变、呼吸困难和肾损伤,所有这些都源于PBD的非靶向输送;该分析表明,2013年至2017年间47%的PBD偶联ADCs的新药申请被中止。这些高效ADCs发生危及生命的毒性的更高发生率是一个限制。
目前减轻PBD毒性的机制包括药物-连接子组分的聚乙二醇化,这显著提高了ADC的耐受性。另一种机制是使用对氨基苄氧羰基(PABC)自毁间隔基,在连接臂-药物中;该间隔基具有稳定的二硫键,允许在细胞内快速释放自由有效载荷,从而实现更好的血浆稳定性和与可裂解连接臂相比提高的毒性。后一项研究认为,肽连接的和二硫键连接的PBD ADC在两种不同的淋巴瘤模型中提供了相似的疗效,并且二硫键连接的PBD ADC具有更好的安全性。第三种机制是通过减少PBD结构中的一个亚胺官能团进行化学修饰,从而将DNA交联的PBD二聚体转变为DNA烷基化代谢物,称为吲哚喹喔啉二聚体(IGN),这在小鼠肿瘤模型中实现了更有效的载荷释放,其中小鼠能够耐受更高剂量的IGN偶联ADC。
近期在有效载荷方面也取得了进展。主要的进展是免疫调节ADC,如干扰素基因刺激剂(STING)激动剂、Toll样受体(TLR)激动剂和使用蛋白酶体靶向嵌合体(PROTAC)策略的目标蛋白降解剂(TPD)。STING激动剂激活干扰素和其他细胞因子的产生,从而增强免疫和抗肿瘤反应。将STING激动剂作为有效载荷纳入ADC可以实现其向肿瘤目标的传递,具有更高的疗效和由于免疫激活导致的过度炎症反应而减少的毒性。STING激动剂的例子包括DMXAA、c-di-AMP、c-di-GMP、cGAMP、ADU-S100、MK-1454、SB11285、BMS-986301、E7766、MSA-1和MSA-2;它们主要在乳腺癌中被探索。TLR激动剂通过增强肿瘤微环境中抗原呈递细胞的抗原呈递,改善先天和适应性抗肿瘤免疫,从而促进更多细胞毒性T细胞的促进和活性。它们在局部癌症中发挥作用,例如,BCG(TLR2/4激动剂)用于膀胱非浸润性癌,AS04(TLR4激动剂)用于宫颈癌,以及咪喹莫特(TLR7激动剂)用于表皮基底细胞癌。目前,许多TLR激动剂正在作为ADC中的有效载荷在癌症免疫疗法中进行研究。一个例子是BDC-1001(TLR7/TLR8激动剂与抗HER2抗体偶联的ADC),在临床前模型中显示出有希望的结果。目前正在进行一项I/II期临床试验,该试验正在招募表达HER2的晚期实体瘤患者(NCT04278144)。PROTAC是一种催化作用于小剂量的催化剂,它通过泛素化介导的蛋白水解作用靶向特定的蛋白质。当PROTAC有效载荷与抗体偶联时,它会产生PROTAC催化行为和抗体的组织特异性的新型组合,具有更好的疗效和更少的限制。在表达HER2的细胞中存在成功的例子。这些在ADC设计中的微妙改进具有巨大的潜力,通过不断的研究可以为肿瘤学带来更好的结果,并为包括淋巴瘤在内的其他癌症类型的发展打开大门。
2.3. 化学连接臂
连接臂是成功开发ADC的最重要和最复杂的部分,因为它们形成了治疗和抗体之间的联系。它们的结合机制、稳定性和化学性质对于防止意外释放药物进入血流以及在癌细胞内吞后促进容易裂解至关重要,允许有效载荷仅在预期的地点释放。它们在确定ADC的药代动力学、药效学和治疗窗口方面至关重要。目前FDA批准的ADC使用两类连接臂,它们在有效载荷释放机制上有所不同:可裂解和不可裂解连接臂。最常用的四种可裂解连接臂是β-葡萄糖醛酸酶敏感连接臂、谷胱甘肽(GSH)敏感二硫键连接臂、卡他蛋白B敏感连接臂和腙连接臂。前面描述的旁观者效应,它影响肿瘤微环境中的正常细胞和没有或低目标表达的肿瘤细胞,更有可能发生在使用可裂解连接臂的ADC中。
不可裂解连接臂与可裂解连接臂相比,具有更好的血浆稳定性、较低的非目标毒性和抗蛋白水解降解的能力,因为它们与抗体的氨基酸残基具有不可还原的键。通常,不可裂解连接臂由硫醚或马来酰亚胺己酰基团形成。附着在由降解的抗体衍生的氨基酸残基上的不可裂解连接臂必须在ADC内化后,由细胞质和溶酶体蛋白酶完全分解抗体部分才能释放有效载荷。图2展示了一般的基本结构。
图2. ADC的一般基本结构。ADC由一个嵌合或人源化(免疫原性较低)的抗体组成,该抗体对淋巴瘤癌细胞表面表达的抗原具有强烈的结合活性。抗体应在循环中具有较高的半衰期,以便被输送到目标细胞表面。抗体与不同结构的有效载荷(主要是微管抑制剂或DNA相互作用)相连,这些是具有理想药物/抗体比例的高效药物。抗体与有效载荷之间的连接是通过可裂解或不可裂解的连接臂实现的,这些连接臂应具有精确的结合、在循环中的稳定性,并确保在目标处有效分配有效载荷。
3.FDA批准用于淋巴瘤的ADC
截至2023年,已有三种ADC获得了FDA对各种类型淋巴瘤的批准,分别是Brentuximab Vedotin(BV)、Polatuzumab Vedotin(PV)和Loncastuximab Tesirine(LT),如表1所示。
Brentuximab Vedotin(BV)由针对CD30的IgG1嵌合单克隆抗体“cAC10”和细胞毒素MMAE组成,它们通过一个稳定的连接臂(Cathepsin可裂解连接臂和对氨基苄基-羰基间隔基)结合在一起。嵌合单克隆抗体cAC10与CD30结合,随后通过内吞作用和随后与溶酶体的囊泡融合,在溶酶体中,溶酶体半胱氨酸蛋白酶裂解连接臂,释放MMAE直接进入癌细胞内,从而导致癌细胞毒性。抗体和MMAE之间的连接系统设计为在循环中稳定,由马来酰亚胺己酰基间隔基、蛋白酶敏感的二肽Val-Cit、自毁PABC基团以及二肽和药物之间的附加间隔基组成。后者具有自裂解的能力,并有助于卡他蛋白B进入其裂解序列。马来酰亚胺部分与抗体重链和轻链中的半胱氨酸残基的末端硫醇形成硫醚键,将连接臂连接到抗体。由蛋白酶裂解Cit-PABC酰胺键产生的不稳定PABC取代的MMAE中间体,通过自发的1,6-消除反应,产生自由的MMAE分子、CO2和对氨基苄基醇。值得注意的是,CD30在恶性淋巴瘤细胞上表达非常强,在正常组织上表达较少。与单独的抗体相比,BV可以使CD30+细胞系的生长停滞高达340倍。BV的结构和作用机制如图3所示。cHL的恶性Reed-Sternberg细胞以表达CD30为特征,CD30是肿瘤坏死因子超家族的成员,鉴于其对一小部分活化的B细胞、T细胞和嗜酸性粒细胞的表达限制,它代表了单克隆抗体治疗的理想靶点。BV在未经治疗的cHL患者和R/R疾病中表现出显著的活性,导致在这些情况下获得FDA批准。
图3. BV的结构和作用机制。它由一个针对淋巴瘤细胞上CD30抗原的单克隆抗体组成。结合后,整个ADC-抗原复合物被细胞内运输到溶酶体,在那里释放MMAE(有效载荷),干扰细胞核中的微管结构,导致细胞周期停滞和凋亡。
ECHELON-1 III期试验将1334名未经治疗的III期或IV期cHL患者随机分配接受BV-AVD(Brentuximab Vedotin、Adriamycin、Vinblastine、Dacarbazine)或ABVD(Adriamycin、Bleomycin、Vinblastine、Dacarbazine)。试验显示BV-AVD组的2年修正无进展生存期(PFS)为82%,而ABVD组为77%,风险比(HR)为0.77,6年总生存期(OS)分别为93.9%和89.4%,HR为0.59。基于ECHELON-1的结果,FDA批准BV与化疗联合用于成人未经治疗的III期或IV期cHL的治疗。最近,SWOG S1826试验被开发出来,比较BV-AVD与N-AVD(Nivolumab、Adriamycin、Vinblastine、Dacarbazine)对儿童和成人新诊断的晚期cHL(III期或IV期)患者的疗效。S1826研究表明,Nivo-AVD的1年PFS(94%)优于BV-AVD(86%),HR为0.48,并且两组的不良事件(AE)概况相当,因此它目前是未经治疗的cHL的一线治疗的首选方案。
尽管年轻患者更容易耐受多药化疗方案,但由于多种因素,包括合并症、身体状况差、无法耐受全剂量化疗以及治疗相关AEs增加,老年cHL人群的治疗结果较差。一项多中心II期研究评估了60岁及以上患者的序贯BV方案,随后进行AVD化疗,并在随后进行BV维持治疗。研究报告了84%的2年PFS率和93%的2年OS率。这种序贯方法提高了这一脆弱人群中cHL的治愈率,是新诊断cHL老年人的首选方案。
在R/R cHL环境中,BV最初在自体造血干细胞移植(ASCT)失败的患者中进行了研究。BV单药治疗显示总响应率(ORR)为75%,完全缓解(CR)为34%,中位无进展生存期(mPFS)为5.6个月。值得注意的是,CR患者的中位持续响应时间(mDOR)为20.5个月。这些结果导致BV首次获得FDA批准,用于治疗ASCT失败或至少两个先前的多药化疗方案失败的cHL患者。随后,AETHERA III期试验包括了接受过ASCT并具有以下不利风险之一的cHL复发难治性疾病患者,例如原发性难治性HL、初次缓解<12个月的复发HL,或一线治疗后复发时的结外受累。AETHERA研究表明,ASCT后早期巩固使用BV将mPFS提高到42.9个月,而对照组为24.1个月,HR为0.57。基于AETHERA试验,FDA随后扩大了BV的批准范围,用于治疗ASCT巩固后有高复发或进展风险的cHL患者。
除了前述的FDA批准外,BV还根据CheckMate 744 II期研究的结果,被国家综合癌症网络(NCCN)指南推荐与Nivolumab联合用于复发或难治性cHL患者的二线或后续治疗。该研究评估了涉及Nivolumab加BV,随后对次优反应患者使用BV加Bendamustine的风险分层响应适应方法。CheckMate 744研究表明,59%接受BV和Nivolumab治疗的患者,以及94%随后接受BV和Bendamustine治疗的患者,实现了完全分子反应(CMR)。这些结果明显优于历史上60至70%的CMR率,为R/R环境中的更高治愈率奠定了基础。
正在进行的BV在cHL的试验如图2所示。
BV在CD30阳性T细胞淋巴瘤中的作用
系统性间变性大细胞淋巴瘤(sALCL)中CD30的普遍表达,以及在外周T细胞淋巴瘤-未另行指明(PTCL-NOS)、血管免疫母细胞性T细胞淋巴瘤(AITL)和成人T细胞白血病或淋巴瘤(ATLL)等亚型中的高表达,为在T细胞淋巴瘤中靶向CD30提供了强有力的理由。
一项针对至少一种联合化疗方案失败后的R/R ALCL患者的II期研究显示,86%的患者实现了客观反应,其中57%为CR,mDOR为12.6个月。这项研究的结果导致FDA批准BV用于R/R PTCL。ECHELON-2试验旨在比较BV与环磷酰胺、多柔比星和泼尼松(A+CHP)联合使用与标准CHOP(环磷酰胺、多柔比星、长春新碱和泼尼松)治疗未经治疗的CD30阳性PTCL患者的疗效和安全性。A+CHP显示出48.2个月的mPFS,与CHOP的20.8个月相比,具有可比的安全性概况。5年PFS分别为A+CHP的51.4%和CHOP的43%(HR 0.7),5年OS分别为A+CHP的70.1%和CHOP的61%(HR 0.72),两组之间的安全性概况相当。随后的亚组分析显示,S-ALCL主要从A+CHP中受益,而AITL和PTCL-NOS亚组的益处尚不明确。
除了PTCL,BV在皮肤T细胞淋巴瘤(CTCL)中的作用也得到了探索。ALCANZA III期试验包括了接受过一线系统治疗的原发性皮肤间变性大细胞淋巴瘤(pcALCL)或表达CD30的蕈样真菌病(MF)的患者。在平均45.9个月的随访中,试验偏爱BV组,ORR为54.7%对12.5%,mPFS为16.7对3.5个月。同样,与医生选择相比,BV组的下一次治疗的中位时间显著更长(14.2对5.6个月;HR 0.27)。基于ALCANZA试验的结果,FDA批准BV用于治疗接受过先前系统治疗的pcALCL或表达CD30的MF患者。目前,BV正在许多早期阶段的试验中进行评估,这些试验包括在表2中。
波拉图珠单抗(PV)由一种抗CD79B的人源化IgG1单克隆抗体组成,通过一个可被蛋白酶裂解的马来酰亚胺己酰基-缬氨酸-PABC肽段连接臂与MMAE结合。一旦波拉图珠单抗与CD79b结合,它就会被内吞并通过内质网运输到溶酶体,在那里发生连接臂裂解,导致有效载荷释放到细胞内诱导凋亡。PV的结构和作用机制如图4所示。
图4. PV的结构和作用机制。PV由一个针对淋巴瘤细胞上的CD79b抗原的单克隆抗体组成。结合后,整个ADC-抗原复合物被内吞到内质体,并与溶酶体融合。然后连接臂被裂解以释放MMAE(有效载荷),这反过来导致细胞核中的有丝分裂停止和细胞死亡。
5.1. PV在弥漫大B细胞淋巴瘤中的应用
弥漫大B细胞淋巴瘤(DLBCL)是非霍奇金淋巴瘤(NHL)最常见的形式。虽然利妥昔单抗的加入显著提高了CHOP化疗的治愈率,但大约40-50%的患者最初反应后会出现难治性疾病或复发。
POLARIX是一项具有里程碑意义的III期研究,评估了PV加入R-CHP(利妥昔单抗、环磷酰胺、多柔比星、泼尼松)在DLBCL一线治疗中的疗效,并与R-CHOP进行了比较。POLARIX证明了pola-R-CHP组2年PFS为76.7%对70.2%,(分层HR 0.73)。两组的整体安全性概况相似。值得注意的是,pola-R-CHP的益处在60岁以上的患者、国际预后指数(IPI)在3到5之间的患者以及具有活化B细胞样亚型的DLBCL患者中观察到。相反,在60岁或以下的患者、有大量疾病、较低IPI评分或滤泡中心B细胞样亚型的DLBCL患者中没有明显益处。基于POLARIX试验,pola-R-CHP是第一个在DLBCL一线治疗中证明比R-CHOP具有更好PFS的方案,并获得了FDA对先前未经治疗的DLBCL、未另行指明(NOS)、高级别B细胞淋巴瘤(HGBL)或IPI评分为2或更高的患者的批准。
POLAR BEAR III期试验比较了mini-R-CHOP与pola-mini-R-CHP作为老年DLBCL患者的一线治疗。初步安全性数据显示,两种方案在老年人(69%在80至90岁之间)和脆弱人群中(16%脆弱,12%的ECOG表现状态为3)都是可耐受的,用波拉图珠单抗替代长春新碱并没有导致3到4级血液学毒性或神经病变的发生率更高。值得注意的是,pola-mini-R-CHP组的胃肠道不良事件频率更高(31%对16%)。基于POLARIX试验的结果,人们倾向于假设pola-mini-R-CHP可能显示出比mini-R-CHOP更好的PFS。因此,这项研究的结果备受期待。
在R/R DLBCL环境中,评估PV安全性和有效性的第一项试验是Ib/II期试验,该试验比较了PV与利妥昔单抗(R)和苯达莫司汀(B)联合使用与单独BR对不适合移植的R/R DLBCL的疗效。pola-BR组显示更高的CR(40%对17.5%),更长的mPFS(9.5对3.7个月,HR 0.36),以及更高的mOS(12.4对4.7个月,HR 0.42)。然而,它导致了更高比例的3到4级中性粒细胞减少症(46.2%对33.3%)、贫血(28.2%对17.9%)和血小板减少症(41%对23.1%),尽管3到4级感染的发生率相似(23.1%对20.5%)。与PV相关的周围神经病变在43.6%的患者中观察到,但大多数是1到2级并解决了。这项试验导致了2019年6月pola-BR的初步批准及其在这种情况下的广泛使用。
波拉图珠单抗的另一个有希望的组合在Ib/II期试验中得到证明,该试验结合了Mosunetuzumab,一种针对CD20和CD3的人源化IgG1双特异性抗体,在R/R DLBCL、HGBCL、转化的FL或3b级FL中。在平均23.9个月的随访中,59.2%的患者对波拉图珠单抗加Mosunetuzumab有反应,45.9%的患者达到了CR。mPFS为11.4个月,mOS为23.3个月。这种方案被良好耐受,最常见的AE是25%患者的中性粒细胞减少症。总的来说,这些结果表明波拉图珠单抗和Mosunetuzumab的组合可以在不适合移植的R/R LBCL中带来具有临床意义的反应和有利的安全性概况。
5.2. PV在其他B细胞非霍奇金淋巴瘤(B-NHL)中的应用
除了DLBCL,包括PV的联合疗法也在惰性B-NHL中进行了探索。在Ib/II期试验中,评估了波拉图珠单抗、奥比妥珠单抗(G)和来普尼(Len)联合治疗R/R FL的安全性和有效性。在平均27个月的随访后,结果显示ORR为76%,CR率高达63%,尽管没有达到预先设定的活性阈值。在平均43.3个月的随访后,mPFS和mOS尚未达到,而4年的里程碑PFS为53%。这些结果与R/R FL的现有标准化疗选择相当,并支持在FL中进一步研究Pola-G-Len方案。
PV的疗效也在套细胞淋巴瘤(MCL)中进行了研究。在一项针对R/R MCL的II期研究中,PV与Mosunetuzumab联合用于先前接受过两线或以上治疗的患者,包括布鲁顿酪氨酸激酶抑制剂(BTKi),并显示出75%的高ORR和70%的CR。然而,需要更多的结果数据来评估其在MCL中的作用,对于对化疗免疫疗法和BTKi耐药的患者迫切需要新的方案。
6.隆卡图珠单抗
CD19是一种在B细胞分化的最早阶段直到浆细胞发育过程中表达的表面糖蛋白。除了正常的B细胞,CD19也在大多数B细胞淋巴瘤中表达。与CD20相比,CD19表现出更均匀的表达,并在抗CD20靶向治疗后的小部分CD20阴性肿瘤中保留,使其成为免疫疗法和联合疗法的选择性靶点。隆卡图珠单抗(LT,ADCT-402)是一种ADC,由一种人源化抗CD19单克隆抗体组成,通过一个可被卡他蛋白裂解的连接臂与高度细胞毒性的DNA小沟交叉链接吲哚喹喔啉二聚体毒素(PBD二聚体)结合。由于其快速的内吞动力学、运输到溶酶体和在循环中的稳定性,LT是针对CD19最有效的ADC。LT的结构和作用机制如图5所示。
图5. LT的结构和作用机制。LT由单克隆抗体Loncastuximab通过可裂解连接臂(统称为Tesirine)与PBD二聚体(有效载荷)相连。该抗体与淋巴瘤细胞上的CD19抗原结合,之后整个复合物被内吞并合并到溶酶体中。接着,PBD被释放到细胞质中,它移动到细胞核,在那里发生DNA交叉链接,导致细胞死亡。
6.1. LT在弥漫大B细胞淋巴瘤中的应用
LT在人体I期研究中显示出对R/R NHL具有临床意义的活性,这导致了LOTIS-2研究,该研究评估了其在R/R DLBCL中的疗效。LT显示出48.3%的ORR,其中50%的应答者达到了CR。虽然mPFS为4.9个月,但达到CR者的mDOR为13.4个月。它展示了通常被良好耐受的安全概况,中性粒细胞减少症是最常见的3级AE(26%),其次是血小板减少症(18%)和γ-谷氨酰转移酶升高(17%)。显著的抗肿瘤活性、持久的反应和可接受的安全概况导致了2021年FDA批准用于治疗经过两线或以上系统治疗后的R/R大B细胞淋巴瘤。批准包括那些有DLBCL NOS、由低级别淋巴瘤引起的DLBCL和HGBL。
在具有里程碑意义的LOTIS-2研究之后,LT与其他靶向疗法的组合,如LOTIS-3中的ibrutinib和LOTIS-5中的单克隆抗CD20抗体rituximab对R-GemOX(利妥昔单抗、吉西他滨和奥沙利铂)进行了评估,但目前尚不清楚这些组合是否会进入临床应用(表2)。
6.2. LT在滤泡性淋巴瘤中的应用
LT在复发/难治性非霍奇金淋巴瘤(R/R NHL)的I期研究中进行了评估,其中在滤泡性淋巴瘤(FL)中显示了78.6%的客观反应率(ORR)。在2023年美国血液学会(ASH)会议上,最近展示了将LT与利妥昔单抗联合应用于R/R FL的II期试验的非常鼓舞人心的结果。该试验显示了95.2%的客观反应率,其中包括66.7%的完全缓解(CR)和28.6%的部分缓解(PR)的比率。
7.其他正在研究、开发和评估用于治疗淋巴瘤的抗体药物偶联物
7.1 针对CD19的抗体药物偶联物
7.1.1 科尔图珠单抗拉伐坦辛
科尔图珠单抗拉伐坦辛(SAR3419)是一种IgG1抗体(huB4),通过二硫键交联剂SPDB与细胞毒素药物DM4相连,靶向CD19。CD19是一种在血液形成分化过程中的B淋巴细胞系高度表达的蛋白,从早期B细胞到成熟B细胞,并在大多数B细胞恶性肿瘤中保持表达。两项II期试验已经研究了科尔图珠单抗拉伐坦辛作为单药或联合用药的使用。一项正在进行的试验正在检查其在R/R DLBCL患者中单药治疗的使用,初步数据显示ORR为44%;然而,mPFS、mOS和DOR尚未得出。它具有可接受的安全性概况,药物在41名患者中有4名因不良事件而中断。另一项试验检查了科尔图珠单抗拉伐坦辛与利妥昔单抗联合用于DLBCL患者,显示出ORR为31.1%,在复发疾病患者中疗效最高(ORR 58.3%),与难治疾病(ORR 43%)或一线治疗(ORR 15.4%)形成对比。总体而言,它显示出mPFS为3.9个月,mOS为9个月,DOR为8.6个月。
7.1.2 德尼珠单抗马佛多汀
德尼珠单抗马佛多汀(SGN-19A或SGN-CD19A)是另一种针对CD19的ADC。它是一种抗体(hBU12-491),通过不可裂解的马来酰亚胺己酰基连接臂与MMAF偶联。一项主要纳入了B-ALL患者(n = 59)的I期试验,以及侵袭性B细胞淋巴瘤(n = 6)和伯基特白血病/淋巴瘤(n = 6),显示DOR为27个月。每3周给药一次,在B-ALL中显示CRc(CR+CRi+CRp)为35%。在六名伯基特白血病/淋巴瘤患者和六名B-LBL患者中,每组只有一名达到CR。最常见的AEs是发热(54%)和恶心(52%)。另一项主要纳入了R/R DLBCL(n = 53),以及MCL(n = 5)和FL(n = 3)的I期试验,与前一次试验相比,在DLBCL中显示出略高的活性,ORR为33%,CR为22%,复发病例的DOR为39周,难治病例为41周。最常见的AEs与眼睛相关:视力模糊(65%)和干眼(52%)。德尼珠单抗马佛多汀在两项II期试验中进一步与化疗联合研究,一项将其与RICE化疗联合用于R/R DLBCL或3B级FL,与单独RICE进行比较,而另一项研究了其与R-CHOP或R-CHP联合对照R-CHOP单独作为DLBCL或3B级FL的一线治疗;然而,这两项试验都被赞助商终止。
7.2 针对CD22的抗体药物偶联物
7.2.1 伊诺珠单抗奥佐加霉素
CD22是一种135 kDa的I型跨膜糖蛋白,是一种在未成熟和成熟B细胞上表达的B细胞系特异性蛋白。它在B细胞恶性肿瘤包括大多数淋巴瘤和白血病中上调表达。目前有两种针对CD22的ADC正在淋巴瘤中进行研究。第一种是伊诺珠单抗奥佐加霉素(CMC-544),一种IgG4 kappa单克隆抗体,带有N-乙酰-γ-卡利奇霉素二甲基肼,一种卡利奇霉素的半合成衍生物,通过4'-乙酰苯氧基丁酸连接,于2017年8月获得FDA批准用于R/R B细胞ALL。一项I期试验研究了其在R/R B细胞NHL患者中的应用,显示79名入组患者的ORR为39%,在FL中为68%,在DLBCL中为15%。然而,DOR很短,DLBCL的mPFS为10.4个月,FL为49天。患者中有90%出现最常见的AE,即血小板减少。一项针对顽固性B细胞NHL(n = 81)的II期试验显示了类似的结果,ORR为67%,CR为31%,mPFS为12.7个月。
7.2.2 匹那珠单抗韦德汀
匹那珠单抗韦德汀(Pina,DCDT2980S,RG-7593)是一种抗CD22的单克隆IgG1抗体,通过可裂解的马来酰亚胺己酰基-缬氨酸-PABC连接臂与MMAF偶联。一项I期试验显示,与利妥昔单抗联合使用相比,作为单药治疗使用时显示出更高的疗效,DLBCL组的ORR分别为25%和17%。在慢性淋巴细胞性白血病(CLL)中未见客观反应。在II期试验ROMULUS中进一步检查了其与利妥昔单抗的联合使用,与R-pola相比,在DLBCL患者中显示出更优越的反应,但在FL患者中没有;DLBCL队列在R-Pina(n = 42)上显示ORR为60%,CR为26%,而R-Pola(n = 39)上为ORR 54%,CR 21%。在这项试验中,两者的AEs相当,R-pina组DLBCL队列的3-5级AEs为79%,R-Pola为77%。在FL队列中,AEs略低,R-Pina和R-Pola的3-4级AEs分别为62%和50%。
7.3 针对CD25的抗体药物偶联物
卡米达卢单抗特西林
CD25是一种I型跨膜蛋白,是白细胞介素-2受体α链,是一种在活化的B细胞、活化和调节性T细胞以及髓系前体上表达的蛋白,在包括淋巴瘤和白血病在内的各种肿瘤中过度表达。卡米达卢单抗特西林(ADCT-301,HuMax-TAC)是一种IgG1单克隆抗体,通过可被卡他蛋白裂解的缬氨酸-丙氨酸二肽连接臂与PBD二聚体弹头(SG3199)偶联。一项I期试验检查了其在R/R cHL(n = 133)和R/R NHL(n = 56)中的疗效,其中在cHL患者中显示出71%的优越ORR和42%的CR,与R/R NHL相比(ORR 38%和CR 9%)。3级及以上AEs包括GGT水平升高(15%)、皮疹(12%)和贫血(11%)。更重要的是,3.8%的患者出现了严重的神经系统事件,包括吉兰-巴雷综合征(GBS)/多神经根病变,27.4%的患者因不良反应而中断治疗。尽管研究报告的CR令人鼓舞,但FDA建议不要提交用于治疗R/R HL的批准文件,因此其未来仍不明朗。
7.4 针对CD37的抗体药物偶联物
纳拉图珠单抗艾美曲辛
CD37是一种参与细胞膜组织和共刺激信号的跨膜蛋白,主要在成熟B细胞上表达,在T细胞、巨噬细胞/单核细胞和粒细胞上表达较少。它在成熟的B细胞恶性肿瘤中高度表达,如CLL,在DLBCL中表达不一,CD37阳性范围从40%到90%的病例,而在急性淋巴细胞性白血病(ALL)和HL中低表达或缺失。纳拉图珠单抗艾美曲辛(IMGN529)是一种IgG1单克隆抗体,通过硫醚连接臂N-succinimidyl-4-(N-maleimidomethyl) cyclohexane-1-carboxylate (SMCC)与美登木素DM1偶联,靶向CD37。
纳拉图珠单抗艾美曲辛最初在R/R B细胞淋巴瘤的I期试验中研究,结果显示最小的效果,总有效率(ORR)为13%。然而,纳拉图珠单抗艾美曲辛与利妥昔单抗联合的II期试验结果显示,在DLBCL中ORR更高,达到44.7%,完全缓解(CR)为31.6%,在FL中的响应率略高,ORR为57%,CR为36%。在中位随访15个月和21.8个月时,DLBCL和FL亚组的中位持续缓解时间(mDOR)尚未达到。治疗总体上被良好耐受,如在FACT-Lym QoL的淋巴瘤子量表上平均提高了三点的生命质量(QoL)测量所示。总体而言,目前尚不清楚它是否会进入III期研究。
7.5 针对CD70的抗体药物偶联物
Vorsetuzumab Mafodotin
CD70是一种共刺激分子,也是肿瘤坏死因子超家族的成员,它在抗原激活的B细胞、T细胞、NK细胞和成熟的树突状细胞上短暂表达。它在实体瘤和血液学恶性肿瘤中异常表达。Vorsetuzumab Mafodotin (SGN-75)是一种ADC,靶向CD70分子和微管毒素分子,连接到单甲基奥瑞斯他汀F(MMAF)。在R/R CD70+ NHL的I期试验中显示出不可接受的毒性,主要是血小板减少症。此外,SGN-CD70A是一种通过稳定、可被蛋白酶裂解的肽基连接臂与PBD二聚体偶联的工程半胱氨酸单克隆抗体(EC-mAb),靶向CD70。同样,它也与不可接受的毒性相关,并且只有适度的活性。
7.6 针对ROR1的抗体药物偶联物
7.6.1. Zilovertamab Vedotin
ROR1是一种酪氨酸激酶跨膜受体,表达在未成熟的B淋巴细胞、内分泌腺和小肠上。它在血液学恶性肿瘤中高度表达,尤其是B细胞淋巴瘤。Zilovertamab Vedotin (MK 2140或VLS-101)是一种针对ROR1的人源化IgG1单克隆抗体,通过可被蛋白酶裂解的连接臂与MMAE偶联。在一项具有里程碑意义的I期试验中,Zilovertamab Vedotin在R/R MCL患者中显示出47%的ORR,CR为20%,在R/R DLBCL患者中ORR为60%。II期waveLINE-004研究,将Zilovertamab Vedotin作为R/R DLBCL的单药治疗,显示出略低的疗效,ORR为30%,有10%的患者实现了CR。最常见的3-4级AEs是中性粒细胞减少症(18%),其次是贫血(15%)。目前有额外的研究正在进行招募;一项是将Zilovertamab Vedotin与R-CHP联合用于DLBCL的前线治疗的II期试验,另一项是评估其与R-GemOX联合对照R-GemOX单独用于R/R DLBCL的II/III期研究。
7.6.2. Cirmtuzumab-ADC-7
另一种针对ROR1的ADC是Cirmtuzumab,一种针对ROR1的单克隆抗体,通过UC-961连接臂与MMAE偶联。在I/II期,Cirmtuzumab与ibrutinib联合用于R/R MCL或治疗未经验(TN)或R/R CLL的管理。在MCL队列中,Cirmtuzumab显示出80%的ORR,35%的患者实现了CR。值得注意的是,在中位随访14.9个月时,mPFS尚未达到。在CLL队列中,结果随着成熟仍然令人鼓舞,TN和R/R CLL患者的mPFS在中位随访14个月和7个月时也未达到。总体而言,该研究正在进行中,结果看起来很有希望。
7.7 临床前开发中的ADCs
7.7.1. 新型CD30靶向ADC:SGN-35C
SGN-35C在组成上与BV相似,都是抗CD30抗体,但在连接臂上有所不同,它连接的是一种新型的喜树碱衍生的拓扑异构酶1抑制剂有效载荷。在CD30阳性ALCL和HL细胞系上进行的体外和体内研究,包括那些对BV有抗性的细胞系,显示出治疗诱导的细胞毒性。值得注意的是,这种效果扩展到了CD30阴性细胞,表明了旁观者效应。非人灵长类动物模型也证实了其安全性。下一步是人类临床试验,目前正在计划中。
7.7.2. CD19靶向ADC:IKS03
IKS03由一种针对CD19的人源化抗体组成,设计用于位点特异性结合PBD前药有效载荷。它通过生物结合激活,产生一种药物与抗体比率为2的偶联物。体外和体内研究已经证明了其在多种CD19阳性淋巴瘤细胞系中的有效细胞毒性,最值得注意的是在含有经常在R/R NHL中观察到的遗传异常的MCL和DLBCL异种移植模型中,如CCND1 t(11;14)易位和三重打击淋巴瘤,涉及BCL-2、BCL-6和c-MYC的基因重排。此外,与其他使用PBD前药的ADC相比,它展示了更低的非特异性有效载荷从偶联物中的释放率,包括LT。目前正在进行I期临床试验NCT05365659,以评估其在晚期B细胞NHL患者中的安全性。
7.7.3. CXCR5靶向ADC:VIP924
VIP924是一种首创的ADC,靶向CXCR5,由一种可被legumain裂解的连接臂和一种微管蛋白抑制剂(KSPi)有效载荷组成。CXCR5是一种趋化因子受体,在B细胞和T细胞来源的淋巴瘤上高度表达,并参与调节肿瘤细胞侵袭、生长和迁移的途径。一项体内研究比较了VIP924与PV和LT在MCL的人性化小鼠模型中的效果。结果表明VIP924在抑制肿瘤生长、提高存活率和耐受性方面的优势。值得注意的是,与LT不同,VIP924组的动物没有经历细胞减少症。这些有希望的结果支持在人类临床试验中进行进一步研究的需求。
8.ADCs的未来发展方向
最近在设计位点特异性ADCs、利用双特异性抗体以及修改可裂解连接臂方面取得了进展,以期使ADCs更有效、更高效,同时最小化毒性。一种新颖的偶联化学方法涉及位点特异性附着,其中一些技术利用抗体中的天然链间二硫键,而其他技术则需要生物工程将酶促偶联标签整合到抗体序列中。尽管在淋巴瘤中尚未探索,但位点特异性偶联已在实体恶性肿瘤(如乳腺癌、卵巢癌和胰腺癌)中得到评估。其中一种应用是ThioMab技术,它涉及使用工程化半胱氨酸进行位点特异性偶联。使用这种技术生产的ADC包括抗MUC16 ADC,它由在曲妥珠单抗的轻链和重链的特定位置插入半胱氨酸残基组成,然后与MMAE上的硫醇基团结合。此外,pClick技术提供位点特异性偶联;然而,它使用天然抗体和近距离激活的交联剂,不涉及任何生物工程。ThioBridge技术包括一种可裂解的连接臂,也使用天然抗体,并由三碳桥接附着提供增强的稳定性。此外,最近创新的AJICAP第二代技术通过利用硫酯化学的选择性裂解反应,实现了无聚集挑战的位点特异性ADC的生产,并有望成为无需抗体工程的位点特异性ADC。最后,通过不同的方法(如糖基重塑、转谷氨酰胺酶或脂酸连接酶方法)对天然抗体进行无标签酶促修饰,作为推进ADC发展的潜在工具具有潜力。
一类有前景的ADCs由双价双特异性抗体组成,如在HER-2靶向ADC中所示。双特异性抗体靶向两个不重叠的表位,随后诱导受体聚集和内化。这类ADCs已在乳腺癌中显示出疗效,并且在临床前研究中检查了MET过表达肿瘤,提供了有效的细胞毒性。
关于连接臂的最新进展,工作集中在制造稳定以避免非目标有效载荷释放的连接臂,但也容易在目标部位裂解以有效传递。这导致制造具有pH和微环境依赖性裂解的连接臂,允许ADCs在细胞内释放有效载荷。
这些进展正处于开发或临床前阶段研究中,有望提高下一代ADCs在包括淋巴瘤在内的各种癌症中的治疗效果。
9.结论
ADCs是革新了霍奇金和非霍奇金淋巴瘤治疗的新方法。抗体、连接臂和有效载荷的进步将导致ADCs的进一步发展,对淋巴瘤具有更高的特异性和细胞毒性。虽然获得抗性将是一个限制因素,但与其他新型药物的联合疗法,如单克隆抗体、分子靶向疗法和双特异性抗体,将为新的突破性治疗铺平道路。我们迫切需要创新的I期研究,以更好地理解ADCs在不同疾病环境中的作用,因为我们的目标是提高淋巴恶性肿瘤的治愈率。
抗体药物偶联物免疫疗法细胞疗法
2024-04-19
前言:20世纪初,Paul Ehrlich提出了药物靶向递送的概念,即“魔术子弹”。理想状态下,它可以精准递送药物到靶细胞,发挥杀伤作用,同时对正常组织无害。随后,抗体-药物偶联的概念被提出,它将单克隆抗体的靶标特异性和细胞毒性分子的抗肿瘤特性结合在一起。历经几十年的尝试,直到2000年靶向CD33的ADC药物Mylotarg(Gemtuzumab Ozogamicin)出现,ADC的发展才取得了实质性的成功,尽管经历了退市、再上市的波折。目前,除了市场上已有的11种经FDA批准的ADC药物,还有超过100种ADCs处于临床试验的不同开发阶段。抗体-药物偶联物 1. ADC的结构ADC由抗体、细胞毒性载荷和化学连接子组成(如图1)。图1 ADC示意图 2. 靶抗原(Antigen)目前,ADC药物的靶抗原主要包括靶向血液恶性肿瘤的CD19、CD22、CD30、CD33和CD79b,以及靶向实体癌的HER2、trop2、nectin4、组织因子和叶酸受体α (FRa)。靶抗原的选择对ADC的设计至关重要:抗原应在肿瘤细胞中单独或高表达,以降低脱靶毒性。抗原-抗体应具有高结合力,以促进复合物的内化。尽量选择靶细胞表面的抗原表位,以便被识别。选择非分泌型抗原,避免抗原分泌导致ADC结合到肿瘤部位外。 3. 抗体(Antibody)理想的抗体片段应能促进有效内化,具有高抗原亲和力,保持较长的血浆半衰期,低免疫原性。单抗的分子量大,占ADC分子量的90%以上,利于减少药物在健康组织中的分布或渗透。而在肿瘤组织中,因为肿瘤的血管系统的渗漏性,使ADC很好地扩散和渗透。 4. 连接子(Linker)ADC的多种特性受到化学连接子的影响,包括特异性、稳定性、效力和毒性。根据在细胞中释放载荷的方式不同,有两种类型的连接子,包括可裂解和不可裂解(如图2)。图2 ADC连接子类型目前,有些ADC利用“旁观者杀伤”作用进行设计,将细胞毒性作用扩展到肿瘤区抗原低表达或阴性的细胞。这一机制要求ADC分子:具有可裂解的连接子和非极性、自由膜渗透的有效载荷。例如,Enhertu (T-DXd)具有可裂解的酶连接子,而目前唯一批准使用不可裂解连接子的ADC是Kadcyla,采用了不可裂解的硫醚连接子。 5. 细胞毒性载荷(Payload)理想情况下,细胞毒性有效载荷应具有以下特性:高效体外细胞毒活性高在体循环中稳定性高在制剂环境中溶解度高易与抗体结合免疫原性低分子量小半衰期长在目前批准的ADC中,主要有两类细胞毒性药物用作有效载荷:微管抑制剂或DNA损伤剂(如图3)。图3 细胞毒性载荷的主要种类及代表ADC药物 6. 偶联除了抗体、连接子和有效载荷的选择外,偶联的方法对ADC的成功构建也很重要。抗体上的赖氨酸和半胱氨酸残基提供了偶联反应位点。传统的偶联方法,小分子毒素会随机偶联在抗体上,药物抗体比(DAR)分布较宽,在0-8范围内。而理想的DAR是2-4,因为较低的DAR会降低疗效,而太高的DAR不利于抗体结构、稳定性和抗原-抗体结合,导致清除速度加快,降低临床活性。 7. 作用机制当ADC到达靶细胞,单克隆抗体识别并结合细胞表面抗原,然后ADC抗原复合物通过内吞作用进入癌细胞,形成早期内体,成熟后与溶酶体融合。释放的活性小分子药物杀伤细胞,导致细胞凋亡或死亡(如图4)。此外,单克隆抗体的Fc部分也能介导免疫相关的细胞毒性。当ADC的抗体与癌细胞的特异性抗原表位结合后,抗原介导的下游信号通路被抑制也会诱导细胞毒性。例如,Trastuzumab Emtansine(T-DM1)中曲妥珠单抗与HER2受体结合,抑制HER2与HER1、HER3或HER4之间异源二聚体的形成,阻断癌细胞存活和增殖的信号转导通路,诱导细胞凋亡。图4 ADC作用机制 8. ADC引发的不良反应ADC的每个成分以及偶联方法都会影响临床疗效和安全性。表1列举了11种ADC的不良反应。表1 ADC药物不良反应FDA批准的11种ADCs Gemtuzumab OzogamicinGemtuzumab ozogamicin(GO,CMA-676)由人源化抗CD33单克隆抗体、卡奇霉素、可切割的连接子组成。抗体与CD33抗原结合后,细胞毒素的内化和释放,从而诱导双链DNA断裂和细胞死亡。2000年5月17日,GO(Mylotarg, Pfizer)被加速批准用于治疗老年复发性CD33阳性急性白血病(AML)患者,但基于安全性和有效性数据于2010年退市。最初的推荐剂量为9 mg/m2,每2周注射2次。2017年9月1日,FDA批准GO作为单药治疗成人复发或难治性(R/R)CD33阳性AML,以及新诊断的成人和1个月及以上儿科患者CD33阳性AML联合化疗。推荐剂量为3mg/m2。 Brentuximab VedotinBrentuximab vedotin(BV)是一种靶向CD30的ADC,由嵌合lgG1抗体cAC10、 MMAE和蛋白酶可切割的连接子组成。内化后,蛋白水解释放MMAE,MMAE通过破坏微管系统诱导细胞周期阻滞和凋亡。由于MMAE具有旁观者效应,BV在表达CD30的组织异质性肿瘤中也有效。2011年8月19日,FDA加速批准了BV(Adcetris, Seattle Genetics)的两种适应症,包括用于治疗霍奇金淋巴瘤患者和用于治疗至少一次多药化疗方案失败后的全身性间变性大细胞淋巴瘤(ALCL)患者。2017年11月9日,FDA批准BV用于治疗既往接受过全身治疗的表达CD30的蕈样真菌病(MF)或原发性皮肤间变性大细胞淋巴瘤(pcALCL)患者。2018年3月20日,BV联合化疗被批准用于治疗新诊断的III/IV期经典霍奇金淋巴瘤成人患者。2018年11月16日,FDA批准BV联合化疗治疗新诊断的全身性间变性大细胞淋巴瘤和其他表达CD30的外周血T细胞淋巴瘤(PTCL)。2022年11月10日,FDA批准BV联合阿霉素、长春新碱、依托泊苷、强的松和环磷酰胺治疗2岁以上儿科患者先前未治疗的高风险经典霍奇金淋巴瘤(cHL)。 Ado-Trastuzumab EmtansineAdo-Trastuzumab Emtansine(Kadcyla)是一种靶向Her2的ADC,由人源化抗Her2 IgG1单抗(曲妥珠单抗)、小分子细胞毒素DM1和不可切割的连接子组成。在体循环和肿瘤微环境中能维持较高的稳定性。其中,曲妥珠单抗与HER2受体亚基I结合后,经溶酶体蛋白水解,释放DM-1。DM-1与微管蛋白结合破坏细胞内的微管网络,从而导致细胞周期阻滞和细胞凋亡。2013年2月22日,FDA批准Trastuzumab Emtansine(Kadcyla,罗氏)用于曾接受曲妥珠单抗和紫杉烷治疗的转移性Her2阳性乳腺癌患者治疗。2019年5月3日,FDA批准Kadcyla作为单一药物用于接受新辅助曲妥珠单抗治疗后残留疾病的Her2阳性乳腺癌患者的辅助治疗。 Inotuzumab OzogamycinInotuzumab ozogamicin由一种人源化抗CD22单克隆抗体,通过酸不稳定的腙连接子与卡奇霉素偶联。CD22是一种内吞受体,是B细胞急性淋巴细胞白血病(ALL)的特异性标志物,在90%以上的B细胞恶性肿瘤患者中表达。一旦ADC与CD22受体结合,该复合物被内化到靶细胞内,触发卡奇霉素的释放,卡奇霉素通过与DNA双螺旋的小沟结合并引起位点特异性双链DNA切割,从而诱导细胞凋亡。2017年8月17日,FDA批准Inotuzumab ozogamicin
(Besponsa, Pfizer)用于治疗复发或难治性B细胞前体ALL成人患者。 Polatuzumab Vedotin PiiqPolatuzumab vedotin是一种由抗CD79b单克隆抗体、蛋白酶可切割的连接子和MMAE偶联。2019年6月10日,FDA加速批准了Polatuzumab vedotin (Polivy,
Roche)联合苯达莫司汀和利妥昔单抗用于治疗接受两种或两种以上治疗后复发或难治性弥漫性大B细胞淋巴瘤。 Enfortumab VedotinEnfortumab vedotin(EV)是一种靶向nectin-4的ADC,由一种靶向nectin-4的人单克隆抗体、蛋白酶可切割的连接子、MMAE偶联。Nectin-4是一种细胞粘附分子,在97%的尿路上皮癌中过表达,并与肿瘤生长和增殖有关。2019年12月18日,FDA加速批准EV (Padcev, Seagen)用于局部晚期或转移性尿路上皮癌的成年患者,这些患者先前接受过程序性死亡受体-1(PD-1)抑制剂或程序性死亡配体受体-1(PD-L1)抑制剂以及含铂化疗药物的治疗。2021年7月9日,FDA批准将EV用于已接受PD-1抑制剂或PD-L1抑制剂和含铂治疗的晚期或转移性尿路上皮癌成人患者,或不符合含顺铂治疗条件且至少接受过一种既往治疗的患者。2023年4月3日,FDA加速批准了对局部晚期或转移性尿路上皮癌且不符合含顺铂化疗条件的患者强制使用vedotin+pembrolizumab的治疗方案。 Trastuzumab DeruxtecanFam-trastuzumab
deruxtecan(T-DXd)由靶向Her2的曲妥珠单抗、可切割的四肽连接子和细胞毒性拓扑异构酶I抑制剂组成。研究表明T-DXd对Her2高或低表达的肿瘤细胞或Her2突变的肿瘤细胞都有效,其原因可能包括:1)T-DXd的DAR值高达8,因此具有高效的有效载荷;2)释放的有效载荷具有较高的膜透性,使其能够进入邻近的肿瘤细胞,产生旁观者效应;3)新型基于四肽的连接子在血浆中具有很高的稳定性。2019年12月,FDA加速批准了fam-trastuzumab deruxtecan
(Enhertu, Daiichi Sankyo)用于不可切除或转移性HER2阳性乳腺癌患者,这些患者曾接受过两种或两种以上HER2靶向治疗方案的转移性治疗。2021年1月15日,被批准用于治疗先前接受过曲妥珠单抗治疗的局部晚期或转移性Her2阳性胃或胃食管交界处腺癌患者。2022年5月4日,被批准用于不可切除或转移性Her2阳性乳腺癌患者,这些患者曾接受过Her2靶向治疗。2022年8月11日,FDA延长并加速批准了不可切除或转移性HER2(ERBB2)突变激活的非小细胞肺癌(NSCLC)的治疗进展。 Sacituzumab GovitecanSacituzumab govitecan由一种靶向Trop-2的单抗,通过酸不稳定的腙可切割连接子与SN-38偶联组成。Trop-2是一种跨膜糖蛋白,在多种实体肿瘤中过表达,是癌症治疗的重要靶点。SN-38是一种拓扑异构酶-1抑制剂,是化疗药物伊立替康的活性代谢物。给药后,ADC与肿瘤细胞上的Trop-2结合,并促使SN-38释放,引发DNA损伤,随后导致细胞周期阻滞。由于SN-38的膜透性,它可以在不被内化的情况下刺激附近细胞的抗肿瘤作用,发挥旁观者效应。2020年4月22日,sacituzumab govitecan
(Trodelvy,Immunomedics)获得FDA加速批准用于对既往接受过两种或两种以上转移性疾病治疗的成人转移性三阴性乳腺癌的治疗。2021年4月7日,获得FDA的常规批准,用于不可切除的局部晚期或转移性三阴性乳腺癌患者,这些患者先前接受过至少两种全身治疗,其中至少一种治疗是针对转移性疾病。2021年4月13日,FDA加速批准了用于先前接受PD-1或PD-L1抑制剂治疗的晚期或转移性尿路上皮癌患者。2023年2月3日,FDA延长了对sacituzumab govitecan用于激素阳性和Her-2/neu阴性转移性乳腺癌患者的批准。 Loncastuximab Tesirine-lpylLoncastuximab tesirine由一种靶向CD19的抗体,通过可切割的酶型连接子与细胞毒性烷基化剂SG3199偶联而成。SG3199是一种合成的PBD二聚体,通过促进DNA链间交联的形成阻止细胞分裂,具有强大的细胞毒性作用。2021年4月23日,Loncastuximab
tesirine(Zynlonta, ADC Therapeutics)获得FDA加速批准,用于弥漫性大B细胞淋巴瘤(DLBCL)患者。 Tisotumab VedotinTisotumab vedotin由一种靶向组织因子(TF-011)的单克隆抗体、一种可切割的mc-VC-PABC连接子和MMAE组成。研究显示,相对正常宫颈组织,TF在宫颈癌组织中大量表达。一旦vedotin与TF结合,MMAE就会被传递到细胞中,从而阻断微管蛋白聚合并终止细胞分裂。2021年9月20日,FDA批准了tisotumab vedotin (Tivdak,
Genmab/Seagen)用于复发或转移性宫颈癌的成年患者,虽接受了化疗,但疾病进展未终止。 Mirvetuximab Soravtansine-GynxMirvetuximab soravtansine由靶向叶酸受体α(FRα)的抗体和微管蛋白靶向细胞毒剂DM4组成,由可切割的二硫键连接子连接。与抗原结合后,ADC被内化,DM4被释放,随后抑制微管,导致细胞周期阻滞和凋亡。游离的DM4及其代谢物可以扩散并杀伤邻近细胞,发挥 “旁观者效应”。2022年11月14日,FDA加速批准mirvetuximab
soravtansine(Elahere, lmmunoGen)用于叶酸受体α(FRα)阳性、铂耐药上皮性卵巢癌、输卵管癌或原发性腹膜癌的成人治疗既往接受过1-3次全身治疗方案。获批后退市的2种ADCs Belantamab Mafodotin-BlmfBelantamab mafodotin由一种靶向B细胞成熟抗原(BCMA)的lgG抗体,通过不可切割的马来酰亚胺基己酰(MC)连接子与MMAF偶联。BCMA是一种在恶性浆细胞上大量表达的细胞表面蛋白,是治疗多发性骨髓瘤的一个很重要的靶点。一旦belantamab maodotin与BCMA结合,该复合物内化并在溶酶体中降解,MMAF释放,诱导生长阻滞和细胞凋亡。2020年8月5日,FDA加速批准Belantamab mafodotin(Blenrep,
GSK)用于复发或难治性多发性骨髓瘤的成人患者,这些患者之前接受过至少四种治疗,其必须包括抗CD38单克隆抗体、免疫调节剂和蛋白酶体抑制剂。然而,2022年11月,应FDA要求,belantamab从美国退市。但目前GSK仍在开展相关临床研究,积极探索其临床价值,如表2。表2 Belantamab mafodotin开展中的临床信息汇总 Moxetumomab pasudotox-TdfkMoxetumomab pasudotox是一种被视为ADC的免疫毒素,由抗CD22单克隆抗体共价连接到假单胞菌外毒素a(PE38)的38kDa片段上。免疫毒素的Fv部分与CD22结合,内化后,通过催化延伸因子-2(EF-2)中二苯二胺残基的ADP核糖基化诱导凋亡。2018年9月13日,FDA批准Moxetumomab
pasudotox(Lumoxiti, AstraZeneca)最用于复发或难治性毛细胞白血病患者,这些患者之前接受过至少两种全身治疗,包括核类似物治疗。然而,在2022年11月,由于临床使用率很低,moxetuomomab宣布于2023年7月撤出美国市场,且moxetumomab的上市后研究也被终止。已上市的国产ADC 维迪西妥单抗维迪西妥单抗(爱地希)是中国首个原创抗体偶联(ADC)药物,由靶向Her2的单克隆抗体,蛋白酶可剪切的ADC连接子(MC-Val-Cit-PAB)与MMAE偶联而成。2021年6月和2021年12月,维迪西妥单抗(爱地希,荣昌生物)获中国药监局批准上市销售,适用于至少接受过2种系统化疗的HER2过表达局部晚期或转移性胃癌(包括胃食管结合部腺癌)患者的治疗,以及2+或3+的局部晚期或转移性尿路上皮癌的治疗。ADC的毒性作用“魔术子弹”概念是相对理想的,其毒理机制主要包括三类:第一种:靶向抗原的正常组织表达——靶毒性。例如,采用Tisotumab vedotin治疗会导致患者产生出血性并发症。此外,MMAE直接递送到组织因子表达的细胞外会导致结膜炎;Sacituzumab govitecan会刺激皮肤和胰腺(Trop阳性)产生皮疹和高血糖。第二种:由细胞毒性载荷决定的特定毒性,如骨髓抑制。例如,卡奇霉素会造成血小板减少和肝功能障碍;MMAE可引起周围神经病变;DM1可诱导胃肠道效应、血小板减少和中性粒细胞减少;拓扑异构酶1抑制剂SN38则与胃肠道副作用相关;烷基化剂SG3199 (PBD二聚体)与γ-谷氨酰转肽酶升高和液体潴留有关,包括可能由血管损伤引起的胸腔积液等。第三种:细胞毒性载荷释放后导致的器官特异性“脱靶”毒性。例如,Trastuzumab emtansine和Trastuzumab-deruxtecan会引起的间质性肺炎(ILD)。携带美登素类毒素的ADC由于脱靶作用,造成眼毒性。ADC开发面临的多种挑战 1) 靶向肿瘤特异性抗原的高亲和力抗体的开发具有挑战。高抗原亲和力并不代表较高的肿瘤穿透性。细胞表面抗原的表达和分布决定了ADC在某一适应症中的治疗效果。 2) ADC的药代动力学和药效学更为复杂,给成药性带来了很大挑战。FcRn介导的抗体清除会将ADC转移到细胞外室进行再循环,导致抗体半衰期较长。细胞毒性载荷在肝脏代谢,经肾脏或粪便排出体外,因此会受到肝肾功能的影响,并改变药物间的相互作用。 3) ADC的耐药性也是很大的挑战,包括有效载荷、抗原表达水平下调以及细胞内运输途径改变所产生的耐药性。ADC未来的前进方向目前ADCs在临床上的成功应用展示出其广阔的前景,从技术迭代优化的角度,未来可集中在:(1) 改进ADC的设计和递送;(2) 开发具有免疫治疗特性或辐射特性的新型有效载荷。 Ø ADC设计和递送的改进a) 改进连接子化学或修饰偶联技术,以提高肿瘤部位递送的特异性和减少脱靶毒性。例如,引入聚乙二醇化的间隔物来提高ADC分子的亲水性,从而改善药代动力学、耐受性和疗效。引入葡萄糖醛酸苷片段用于保护连接体免受体循环中非特异性肽酶的切割,以减少脱靶毒性。 b) 优化有效载荷的化学结构。例如,将与DNA交联的PBD二聚体的化学结构进行重新排列可以更有效地释放游离载荷。此外,开发的有效载荷结合敏感增强剂(PBSE),可以与ADC共同给药,以减少组织中释放的有效载荷的暴露并促进血浆清除。 c) 精确控制DAR,并通过共轭到更稳定的位置以提高有效载荷的稳定性。 d) 开发双特异性抗体偶联物。例如,靶向HER2和CD63的双特异性ADC在HER2阳性肿瘤细胞中表现出更好的内化和溶酶体积累。 e) 开发肽-药物偶联物(Peptide-drug conjugates,
PDCs),利用多肽链靶向肿瘤抗原。例如,已被FDA批准用于恶性肿瘤的治疗的2种PDC:Lu 177标记DOTA-TATE(放射性核素),用于治疗生长抑素受体阳性的胃肠胰腺神经内分泌肿瘤(GEP-NETS);美法仑氟苯胺(Melflufen),用于治疗复发或难治性多发性骨髓瘤患者,但后来退出市场。 f) 开发携带不同细胞毒性载荷的ADC。 Ø 开发具有免疫治疗特性或放射特性的新型有效载荷 a) 开发免疫刺激抗体偶联物(ISACs)。ISACs通过抗体介导的免疫刺激剂的靶向递送,刺激促炎细胞因子涌入,最终激活树突状细胞和T细胞的抗肿瘤应答。虽然尚无ISACs获得FDA的批准,但不少企业布局了这一赛道。例如,2022年6月28日,Astellas Pharma与Sutro Biopharma宣布共同开发新型免疫刺激抗体药物偶联物。 b) 开发放射性同位素类的有效载荷。例如,Lu 177成功获批上市。近几年,在国内医保改革、经济下行、国际形势多变、产品内卷严重等多重因素影响下,生物药行业整体处于增速下降阶段,面临着严峻的考验。因此,技术的创新和产品多样化开发显得尤为重要。而后疫情时代,ADC药物俨然成为创新药开发的主力军,具有广阔的市场前景。参考资料[1] Tsuchikama K, An Z.
Antibody-drug conjugates: recent advances in conjugation and linker
chemistries. Protein Cell. 2018 Jan;9(1):33-46.[2] Hofland P, Portillo S. What
are Antibody-drug Conjugates? – ADC Review / Journal of Antibody-drug
Conjugates – March 22, 2019. DOI: 10.14229/jadc.2019.03.22.001.[3] Gogia P, Ashraf H, Bhasin
S, Xu Y. Antibody-Drug Conjugates: A Review of Approved Drugs and Their
Clinical Level of Evidence. Cancers (Basel). 2023 Jul 30;15(15):3886.[4] https://clinicaltrials.gov[5] https://www.remegen.cn/index.php[6] 药物说明书识别微信二维码,添加生物制品圈小编,符合条件者即可加入生物制品微信群!请注明:姓名+研究方向!版权声明本公众号所有转载文章系出于传递更多信息之目的,且明确注明来源和作者,不希望被转载的媒体或个人可与我们联系(cbplib@163.com),我们将立即进行删除处理。所有文章仅代表作者观点,不代表本站立场。
抗体药物偶联物上市批准
2024-01-16
·创鉴汇
▎药明康德内容团队编辑回顾2023年,抗体药物偶联物(ADC)药物已成为最热赛道之一,从辉瑞的大手笔收购ADC药物公司Seagen,到ADC代表国产创新药密集出海。ADC正逐步成为肿瘤领域的主流疗法。那么,在ADC药物管线中,又有哪些有望在2024年中国获批上市、造福病患呢?本文将结合中国国家药品监督管理局药品审评中心(CDE)公开信息及其他公开披露数据,盘点有望于2024年在中国获批的ADC药物,仅供读者参阅。A166(舒泰来)构成:曲妥珠单抗(HER2)+可裂解Linker+微管蛋白抑制剂(Duo-5)适应症:乳腺癌A166是通过赖氛酸定点定量偶联、具有创新Linker和高活性毒素小分子的第三代HER2 ADC,具有良好的血液稳定性。凭借关键2期临床研究,其上市申请已于2023年5月11日被受理,预计今年内可获批上市,拟治疗既往经二线及以上抗HER2治疗失败的HER2阳性不可切除的局部晚期、复发或转移性乳腺癌患者。同时,A166也在积极探索对HER2阳性胃癌或胃食管结合部腺癌、结直肠癌和非小细胞肺癌等适应症的治疗,已有多项临床试验在同步开展中。此外,对于已申报上市申请的乳腺癌适应症,一项与已获批同类药物进行对比的3期临床试验正在进行中。SKB264(Sacituzumab tirumotecan,MK-2870,佳泰莱)构成:Sacituzumab(TROP2)+可裂解Linker+拓扑异构酶I抑制剂适应症:三阴乳腺癌SKB264是由科伦博泰拥有自主知识产权的靶向TROP2的人源化单克隆抗体、可酶促裂解的Linker和新型拓扑异构酶I抑制剂组合而成的新一代抗体偶联药物,结合了单抗对肿瘤细胞表面靶抗原的特异性和细胞毒性药物的高效性。其用于治疗既往经二线及以上标准治疗的不可手术切除的局部晚期、复发或转移性三阴乳腺癌(TNBC)的3期临床达到主要研究终点,上市申请已于2023年12月9日被受理并被CDE纳入优先审评,预计最早今年可获批上市。同时,SKB264也在积极探索对非小细胞肺癌(NSCLC)的治疗,针对EGFR突变的NSCLC已进展至3期临床研究。SKB264的海外权益已于2022年授权给默沙东,针对非小细胞肺癌、子宫内膜癌的多项全球多中心3期临床研究正在同步开展。维恩妥尤单抗(Enfortumab vedotin)构成:Enfortumab(nectin-4)+可裂解Linker+微管蛋白抑制剂(MMAE)适应症:尿路上皮癌维恩妥尤单抗是安斯泰来和Seagen开发的First-in-class直接作用于 Nectin-4 的抗体偶联药物;其ADC链接技术来自Seagen,靶点鉴定由安斯泰来完成。在美国,维恩妥尤单抗于 2019首次获批上市,适应症为既往已接受一种PD-1/L1抑制剂治疗、并且在手术前(新辅助,neoadjuvant)或手术后(辅助,adjuvant)已接受了一种含铂化疗方案的局部晚期或转移性尿路上皮癌成人患者;2021 年扩大适应症,用于治疗顺铂不耐受且既往接受过一线或多线系统治疗的局部晚期或转移性尿路上皮癌成人患者。基于维恩妥尤单抗治疗既往接受PD-1/PD-L1抑制剂和含铂化疗治疗的局部晚期或转移性尿路上皮癌的中国患者的2期临床研究(EV-203)达到主要临床终点,客观缓解率(ORR)为37.5%, 中位无进展生存时间(mPFS)为4.67个月,其上市申请已于2023年3月10日被受理,预计今年可获批上市。索米妥昔单抗(Mirvetuximab soravtansine)构成:Mirvetuximab(FRα)+可裂解Linker+微管蛋白抑制剂(DM4)适应症:上皮性卵巢癌、输卵管癌或原发性腹膜癌索米妥昔单抗是ImmunoGen开发的一种靶向叶酸受体α(FRα)的First-in-class 抗体偶联药物,也是美国FDA批准的第一种用于治疗铂耐药疾病的ADC,于2022年基于关键性单臂研究SORAYA临床研究数据,ORR为32.4%,获得FDA加速批准上市。华东医药全资子公司中美华东于2020年license in该款药物的大中华区权益。索米妥昔单抗的上市申请已于2023年10月26日获受理并被CDE纳入优先评审,拟用于治疗既往接受过1-3种系统治疗的FRα阳性的铂类耐药的上皮性卵巢癌、输卵管癌或原发性腹膜癌成年患者,预计最早今年可获批上市。泰朗妥昔单抗(Loncastuximab tesirine)构成:Loncastuximab(CD19)+可裂解Linker+DNA损伤剂(PBD)适应症:大B细胞淋巴瘤泰朗妥昔单抗是全球First-in-class靶向CD19的抗体偶联药物,与表达CD19的肿瘤细胞结合时后被细胞内化,随后释放吡咯并苯二氮杂䓬二聚体(PBD)细胞毒素。PBD与DNA小沟结合并抑制DNA复制,阻断细胞周期从而导致肿瘤细胞死亡。2021年泰朗妥昔单抗获得美国FDA加速批准上市,单药用于治疗至少接受过2线及以上系统治疗的复发/难治性弥漫性大B细胞淋巴瘤(R/R DLBCL)成年患者。2020年12月,ADC Therapeutics与瓴路药业宣布成立合资公司Overland ADCT BioPharma, 瓴路药业获得ADC Therapeutics 的包括泰朗妥昔单抗在内的4款ADC药物大中华区和新加坡权益。基于泰朗妥昔单抗单药用于治疗R/R DLBCL中国患者的2期临床研究(OL-ADCT-402-001)达到主要临床终点,其上市申请已于2023年7月13获受理并被CDE纳入优先评审,预计今年可获批上市。读者们请星标⭐创鉴汇,第一时间收到推送免责声明:药明康德内容团队专注介绍全球生物医药健康研究进展。本文仅作信息交流之目的,文中观点不代表药明康德立场,亦不代表药明康德支持或反对文中观点。本文也不是治疗方案推荐。如需获得治疗方案指导,请前往正规医院就诊。版权说明:本文由药明康德内容团队根据公开资料整理编辑,欢迎个人转发至朋友圈,谢绝媒体或机构未经授权以任何形式转发/复制至其他平台。转发授权请在「创鉴汇」微信公众号留言联系我们。更多数据内容推荐点击“在看”,分享创鉴汇健康新动态
临床3期优先审批临床2期抗体药物偶联物上市批准
100 项与 Loncastuximab 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 肿瘤 | 药物发现 | 瑞士 | 2013-10-11 | |
| 肿瘤 | 药物发现 | 美国 | 2013-10-11 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或

核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

标准版
¥16800
元/账号/年
新药情报库 | 省钱又好用!
立即使用
来和芽仔聊天吧
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用

